Specificity calculation and interpretation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Specificity calculation and interpretation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Specificity calculation and interpretation US Medical PG Question 1: A mother presents to the family physician with her 16-year-old son. She explains, "There's something wrong with him doc. His grades are getting worse, he's cutting class, he's gaining weight, and his eyes are often bloodshot." Upon interviewing the patient apart from his mother, he seems withdrawn and angry at times when probed about his social history. The patient denies abuse and sexual history. What initial test should be sent to rule out the most likely culprit of this patient's behavior?
- A. Complete blood count
- B. Sexually transmitted infection (STI) testing
- C. Blood culture
- D. Urine toxicology screen (Correct Answer)
- E. Slit lamp examination
Specificity calculation and interpretation Explanation: ***Urine toxicology screen***
- The patient's presentation with **declining grades**, **cutting class**, **weight gain**, **bloodshot eyes**, and **irritability** are classic signs of **substance abuse** in an adolescent.
- A **urine toxicology screen** is the most appropriate initial test to detect common illicit substances, especially given the clear signs pointing towards drug use.
*Slit lamp examination*
- This test is used to examine the **anterior segment of the eye**, including the conjunctiva, cornea, iris, and lens.
- While the patient has **bloodshot eyes**, this specific test would be more relevant for ruling out ocular infections or injuries, not for diagnosing the underlying cause of systemic behavioral changes.
*Complete blood count*
- A **complete blood count (CBC)** measures different components of the blood, such as red blood cells, white blood cells, and platelets.
- A CBC is a general health indicator and while it can detect infections or anemia, it is not specific or sensitive enough to identify the cause of the behavioral changes described.
*Sexually transmitted infection (STI) testing*
- Although the patient denies sexual history, all adolescents presenting with certain risk factors or symptoms may warrant STI testing in a broader health assessment.
- However, in this scenario, the primary cluster of symptoms (poor grades, cutting class, bloodshot eyes, irritability) points more directly to substance abuse than to an STI.
*Blood culture*
- A **blood culture** is used to detect the presence of bacteria or other microorganisms in the bloodstream, indicating a systemic infection (sepsis).
- The patient's symptoms are not indicative of an acute bacterial bloodstream infection, and a blood culture would not be the initial test for the presented behavioral changes.
Specificity calculation and interpretation US Medical PG Question 2: A scientist in Boston is studying a new blood test to detect Ab to the parainfluenza virus with increased sensitivity and specificity. So far, her best attempt at creating such an exam reached 82% sensitivity and 88% specificity. She is hoping to increase these numbers by at least 2 percent for each value. After several years of work, she believes that she has actually managed to reach a sensitivity and specificity even greater than what she had originally hoped for. She travels to South America to begin testing her newest blood test. She finds 2,000 patients who are willing to participate in her study. Of the 2,000 patients, 1,200 of them are known to be infected with the parainfluenza virus. The scientist tests these 1,200 patients’ blood and finds that only 120 of them tested negative with her new test. Of the following options, which describes the sensitivity of the test?
- A. 82%
- B. 86%
- C. 98%
- D. 90% (Correct Answer)
- E. 84%
Specificity calculation and interpretation Explanation: ***90%***
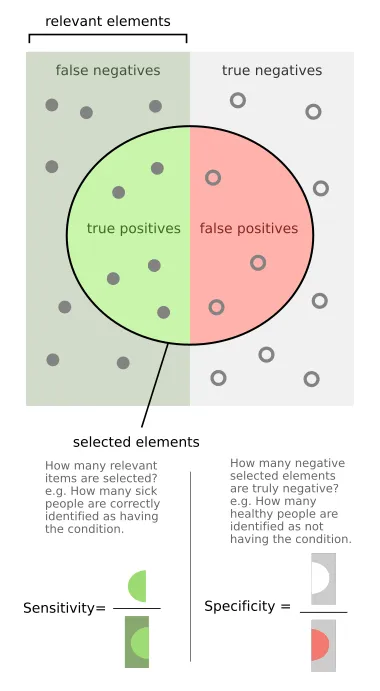
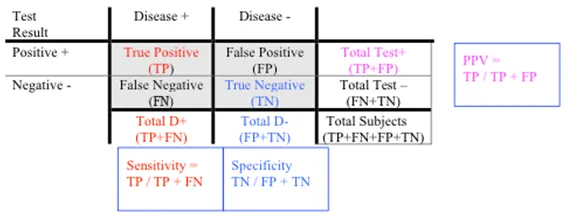
- **Sensitivity** is calculated as the number of **true positives** divided by the total number of individuals with the disease (true positives + false negatives).
- In this scenario, there were 1200 infected patients (total diseased), and 120 of them tested negative (false negatives). Therefore, 1200 - 120 = 1080 patients tested positive (true positives). The sensitivity is 1080 / 1200 = 0.90, or **90%**.
*82%*
- This value was the **original sensitivity** of the test before the scientist improved it.
- The question states that the scientist believes she has achieved a sensitivity "even greater than what she had originally hoped for."
*86%*
- This value is not directly derivable from the given data for the new test's sensitivity.
- It might represent an intermediate calculation or an incorrect interpretation of the provided numbers.
*98%*
- This would imply only 24 false negatives out of 1200 true disease cases, which is not the case (120 false negatives).
- A sensitivity of 98% would be significantly higher than the calculated 90% and the initial stated values.
*84%*
- This value is not derived from the presented data regarding the new test's performance.
- It could be mistaken for an attempt to add 2% to the original 82% sensitivity, but the actual data from the new test should be used.
Specificity calculation and interpretation US Medical PG Question 3: An investigator is measuring the blood calcium level in a sample of female cross country runners and a control group of sedentary females. If she would like to compare the means of the two groups, which statistical test should she use?
- A. Chi-square test
- B. Linear regression
- C. t-test (Correct Answer)
- D. ANOVA (Analysis of Variance)
- E. F-test
Specificity calculation and interpretation Explanation: ***t-test***
- A **t-test** is appropriate for comparing the means of two independent groups, such as the blood calcium levels between runners and sedentary females.
- It assesses whether the observed difference between the two sample means is statistically significant or occurred by chance.
*Chi-square test*
- The **chi-square test** is used to analyze categorical data to determine if there is a significant association between two variables.
- It is not suitable for comparing continuous variables like blood calcium levels.
*Linear regression*
- **Linear regression** is used to model the relationship between a dependent variable (outcome) and one or more independent variables (predictors).
- It aims to predict the value of a variable based on the value of another, rather than comparing means between groups.
*ANOVA (Analysis of Variance)*
- **ANOVA** is used to compare the means of **three or more independent groups**.
- Since there are only two groups being compared in this scenario, a t-test is more specific and appropriate.
*F-test*
- The **F-test** is primarily used to compare the variances of two populations or to assess the overall significance of a regression model.
- While it is the basis for ANOVA, it is not the direct test for comparing the means of two groups.
Specificity calculation and interpretation US Medical PG Question 4: The World Health Organization suggests the use of a new rapid diagnostic test for the diagnosis of malaria in resource-limited settings. The new test has a sensitivity of 70% and a specificity of 90% compared to the gold standard test (blood smear). The validity of the new test is evaluated at a satellite health center by testing 200 patients with a positive blood smear and 150 patients with a negative blood smear. How many of the tested individuals are expected to have a false negative result?
- A. 60 (Correct Answer)
- B. 15
- C. 135
- D. 155
- E. 195
Specificity calculation and interpretation Explanation: ***Correct Option: 60***
- **False negatives** occur in individuals who have the disease but test negative. This is directly related to the test's **sensitivity**.
- Given a sensitivity of 70%, 30% of actual positive cases (100% - 70%) will be missed. With 200 patients having a positive blood smear (meaning they have malaria), 30% of 200 is 0.30 × 200 = **60**.
*Incorrect Option: 15*
- This number represents the expected number of **false positives** (150 patients without disease × 10% false positive rate = 15).
- However, the question asks for **false negatives**, not false positives.
*Incorrect Option: 135*
- This value represents the number of **true negatives** (150 patients without malaria × 90% specificity = 135).
- It does not represent false negative results.
*Incorrect Option: 155*
- This appears to be a distractor number that doesn't correspond to any standard diagnostic test calculation in this scenario.
- It does not represent false negatives or any meaningful combination of the given parameters.
*Incorrect Option: 195*
- This number might be derived from incorrectly applying formulas or miscalculating the relationship between sensitivity and false negatives.
- It does not represent the correct calculation for false negatives.
Specificity calculation and interpretation US Medical PG Question 5: A 21-year-old U.S. born first year medical student with no prior hospital or healthcare work presents to the physician for a routine physical exam. The patient is HIV negative, denies drug use, and denies sick contacts. The physician places a purified protein tuberculin test in the patient's right forearm intradermally. What is the proper time to read the test and induration diameter that would indicate a positive test result?
- A. 36 hours and 7mm diameter
- B. 48 hours and 11mm diameter
- C. 72 hours and 16mm diameter (Correct Answer)
- D. 96 hours and 14mm diameter
- E. 24 hours and 18mm diameter
Specificity calculation and interpretation Explanation: ***72 hours and 16mm diameter***
- The **purified protein derivative (PPD) test** should ideally be read between 48 and 72 hours after administration to allow for the **Type IV hypersensitivity reaction** to fully develop.
- For individuals with no known risk factors for tuberculosis and no prior exposure, an induration of **≥15 mm** is considered a positive result. A 16mm diameter falls within this range.
*36 hours and 7mm diameter*
- **36 hours** is too early to accurately read a PPD test, as the delayed-type hypersensitivity reaction may not have fully manifested.
- A **7mm induration** would generally be considered negative in a low-risk individual, as the threshold for positivity in this group is higher.
*48 hours and 11mm diameter*
- While **48 hours** is within the acceptable window for reading a PPD test, an **11mm induration** is not considered positive for a young, low-risk individual without any predisposing conditions like HIV or organ transplant.
- The threshold for a positive result in this demographic is typically **≥15 mm**.
*96 hours and 14mm diameter*
- **96 hours** (4 days) is generally too late to accurately read a PPD test, as the reaction may begin to fade, leading to a potentially false negative.
- A **14mm induration** is still below the positive threshold of ≥15mm for a low-risk individual.
*24 hours and 18mm diameter*
- **24 hours** is significantly too early to read a PPD test, as the immune response will not have fully developed, leading to unreliable results.
- While **18mm induration** would be a positive result, the timing makes the reading invalid.
Specificity calculation and interpretation US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Specificity calculation and interpretation Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Specificity calculation and interpretation US Medical PG Question 7: You are reviewing raw data from a research study performed at your medical center examining the effectiveness of a novel AIDS screening examination. The study enrolled 250 patients with confirmed AIDS, and 240 of these patients demonstrated a positive screening examination. The control arm of the study enrolled 250 patients who do not have AIDS, and only 5 of these patients tested positive on the novel screening examination. What is the NPV of this novel test?
- A. 240 / (240 + 15)
- B. 240 / (240 + 5)
- C. 240 / (240 + 10)
- D. 245 / (245 + 10) (Correct Answer)
- E. 245 / (245 + 5)
Specificity calculation and interpretation Explanation: ***245 / (245 + 10)***
- The **negative predictive value (NPV)** is calculated as **true negatives (TN)** divided by the sum of **true negatives (TN)** and **false negatives (FN)**.
- In this study, there are 250 patients with AIDS; 240 tested positive (true positives, TP), meaning 10 tested negative (false negatives, FN = 250 - 240). There are 250 patients without AIDS; 5 tested positive (false positives, FP), meaning 245 tested negative (true negatives, TN = 250 - 5). Therefore, NPV = 245 / (245 + 10).
*240 / (240 + 15)*
- This calculation incorrectly uses the number of **true positives** (240) in the numerator and denominator, which is relevant for **positive predictive value (PPV)**, not NPV.
- The denominator `(240 + 15)` does not correspond to a valid sum for calculating NPV from the given data.
*240 / (240 + 5)*
- This calculation incorrectly uses **true positives** (240) in the numerator, which is not part of the NPV formula.
- The denominator `(240 + 5)` mixes true positives and false positives, which is incorrect for NPV.
*240 / (240 + 10)*
- This incorrectly places **true positives** (240) in the numerator instead of **true negatives**.
- The denominator `(240+10)` represents **true positives + false negatives**, which is related to sensitivity, not NPV.
*245 / (245 + 5)*
- This calculation correctly identifies **true negatives** (245) in the numerator but incorrectly uses **false positives** (5) in the denominator instead of **false negatives**.
- The denominator for NPV should be **true negatives + false negatives**, which is 245 + 10.
Specificity calculation and interpretation US Medical PG Question 8: A pharmaceutical company develops a sequential testing protocol for a rare genetic disorder (prevalence 0.01%). Initial screening test has sensitivity 95% and specificity 90%. Positive results undergo confirmatory testing with sensitivity 99% and specificity 99.5%. The company claims this approach achieves PPV >80% for the final positive result. Evaluate this claim and the rationale for sequential testing in this context.
- A. The claim is true; sequential testing increases PPV by enriching the population tested in the second step (Correct Answer)
- B. The claim is false; sensitivity decreases with sequential testing, reducing PPV
- C. Sequential testing is unnecessary; the first test alone achieves adequate PPV
- D. The claim is false; sequential testing cannot achieve PPV >80% with such low prevalence
- E. The claim is true; the high specificity of the confirmatory test ensures high PPV regardless of prevalence
Specificity calculation and interpretation Explanation: ***The claim is true; sequential testing increases PPV by enriching the population tested in the second step***
- Sequential testing works by increasing the **pre-test probability** for the second test, as the cohort being tested has already screened positive once.
- By applying a highly specific confirmatory test to this enriched group, the number of **false positives** is significantly reduced, which drastically improves the **Positive Predictive Value (PPV)**.
*The claim is false; sequential testing cannot achieve PPV >80% with such low prevalence*
- Even with a low **prevalence**, the multiplication of specificities in a sequential process can reduce the **False Positive** rate to a level where the PPV exceeds 80%.
- This line of reasoning ignores that the **denominator** of the PPV calculation (True Positives + False Positives) decreases much faster than the numerator during the second stage.
*The claim is true; the high specificity of the confirmatory test ensures high PPV regardless of prevalence*
- While high **specificity** is crucial, PPV is always dependent on the **prevalence** (pre-test probability) of the condition in the group being tested.
- The claim is true because sequential testing specifically raises that **pre-test probability**, not because prevalence is irrelevant to the calculation.
*The claim is false; sensitivity decreases with sequential testing, reducing PPV*
- It is true that **net sensitivity** decreases in sequential testing, but a decrease in sensitivity actually tends to have a negligible effect on PPV compared to specificity gains.
- **PPV** is primarily driven by the **specificity** and the prevalence in the tested population, both of which are optimized in this two-step protocol.
*Sequential testing is unnecessary; the first test alone achieves adequate PPV*
- Given a prevalence of 0.01% and 90% specificity, the **first test** alone would yield a massive amount of false positives, resulting in a very low PPV (~0.09%).
- A **confirmatory test** is clinically and ethically necessary to avoid wrongly diagnosing thousands of healthy individuals with a **rare genetic disorder**.
Specificity calculation and interpretation US Medical PG Question 9: A hospital system is implementing a sepsis screening algorithm using clinical criteria with sensitivity of 92% and specificity of 75%. False positives result in unnecessary antibiotics, cultures, and ICU evaluations costing $3,000 per case. Missing true sepsis cases (false negatives) results in average increased mortality and morbidity costs of $50,000 per case. Hospital sepsis prevalence is 8%. Evaluate the optimal threshold adjustment strategy.
- A. Maintain current threshold as it balances sensitivity and specificity equally
- B. Implement risk stratification with different thresholds for different populations
- C. Abandon screening due to unacceptable false positive rate
- D. Increase threshold to improve specificity and reduce costs from false positives
- E. Decrease threshold to improve sensitivity despite more false positives (Correct Answer)
Specificity calculation and interpretation Explanation: ***Decrease threshold to improve sensitivity despite more false positives***
- In sepsis screening, the **cost of a false negative** ($50,000) is nearly 17 times higher than the **cost of a false positive** ($3,000), necessitating a strategy that prioritizes **sensitivity** to minimize missed cases.
- Lowering the threshold further ensures fewer high-cost **mortality and morbidity** events occur, which is the most economically and clinically sound approach given the significant **weighted cost** of missing a diagnosis.
*Increase threshold to improve specificity and reduce costs from false positives*
- Increasing the threshold would increase the number of **false negatives**, leading to massive financial losses due to the $50,000 cost per missed **sepsis case**.
- While it reduces the $3,000 expense of unnecessary **antibiotics and cultures**, the savings are mathematically dwarfed by the increased costs of untreated sepsis.
*Maintain current threshold as it balances sensitivity and specificity equally*
- A balanced threshold is inappropriate when the **consequences of error types** are highly asymmetrical; the algorithm should favor the side with the more severe outcome.
- Simply balancing **sensitivity and specificity** fails to account for the 8% **prevalence** and the extreme disparity in costs between false positives and false negatives.
*Implement risk stratification with different thresholds for different populations*
- While risk stratification is useful, it does not address the fundamental need to minimize **false negatives** across the entire 8% prevalence population.
- This approach adds **operational complexity** without necessarily solving the primary economic imbalance between **screening costs** and mortality costs.
*Abandon screening due to unacceptable false positive rate*
- Abandoning screening would lead to an even higher rate of **missed sepsis cases**, resulting in catastrophic clinical outcomes and **increased hospital liability**.
- The current 75% **specificity** is acceptable because the clinical priority in sepsis is **early detection** to prevent rapid physiological deterioration.
Specificity calculation and interpretation US Medical PG Question 10: A 58-year-old man with chronic cough undergoes evaluation for tuberculosis. A tuberculin skin test (TST) is positive (15mm induration). TST has sensitivity of 80% and specificity of 95% in immunocompetent adults. However, he received BCG vaccination as a child in Asia. Local TB prevalence is 0.5%, but his occupational exposure increases his pre-test probability to 10%. Evaluate the most appropriate interpretation and management approach.
- A. Calculate post-test probability and obtain interferon-gamma release assay (IGRA) (Correct Answer)
- B. Repeat TST in 2 weeks to confirm
- C. Treat empirically regardless of test characteristics
- D. Positive test confirms TB; start treatment immediately
- E. False positive due to BCG; no further testing needed
Specificity calculation and interpretation Explanation: ***Calculate post-test probability and obtain interferon-gamma release assay (IGRA)***
- In individuals previously vaccinated with **BCG**, the **Tuberculin Skin Test (TST)** can yield **false positives** because the test cross-reacts with BCG antigens, whereas **IGRA** is more specific.
- Clinical decision-making requires integrating **pre-test probability** (10% in this case) with test characteristics to determine **post-test probability** before starting long-term therapy.
*Positive test confirms TB; start treatment immediately*
- A positive **TST** in a patient with a **BCG vaccination** history does not automatically confirm infection; it lacks the specificity to distinguish between vaccination and actual **Mycobacterium tuberculosis** infection.
- Starting **antitubercular therapy** immediately without ruling out a false positive or assessing for **active versus latent disease** violates standard diagnostic protocols.
*False positive due to BCG; no further testing needed*
- While **BCG** causes false positives, the patient’s **occupational exposure** and a significant **15mm induration** make infection plausible; dismissing the result is unsafe.
- High-risk individuals require definitive testing, usually via **IGRA**, to ensure **latent tuberculosis infection (LTBI)** is not overlooked.
*Repeat TST in 2 weeks to confirm*
- Repeating a **TST** within a short window can lead to the **booster effect**, where the second test appears positive due to immunological memory rather than new infection.
- Re-testing with the same diagnostic tool does not solve the underlying issue of **BCG cross-reactivity**; a different, more specific test is required.
*Treat empirically regardless of test characteristics*
- Empirical treatment ignores the potential for **medication toxicity** (e.g., hepatotoxicity from Isoniazid) in a patient who might not actually have **LTBI**.
- Evidence-based medicine requires utilizing **sensitivity, specificity, and prevalence** to justify treatment, especially when more specific tests like **IGRA** are available.
More Specificity calculation and interpretation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 )
)
