ROC curves US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for ROC curves. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
ROC curves US Medical PG Question 1: A researcher is trying to determine whether a newly discovered substance X can be useful in promoting wound healing after surgery. She conducts this study by enrolling the next 100 patients that will be undergoing this surgery and separating them into 2 groups. She decides which patient will be in which group by using a random number generator. Subsequently, she prepares 1 set of syringes with the novel substance X and 1 set of syringes with a saline control. Both of these sets of syringes are unlabeled and the substances inside cannot be distinguished. She gives the surgeon performing the surgery 1 of the syringes and does not inform him nor the patient which syringe was used. After the study is complete, she analyzes all the data that was collected and performs statistical analysis. This study most likely provides which level of evidence for use of substance X?
- A. Level 3
- B. Level 1 (Correct Answer)
- C. Level 4
- D. Level 5
- E. Level 2
ROC curves Explanation: ***Level 1***
- The study design described is a **randomized controlled trial (RCT)**, which is considered the **highest level of evidence (Level 1)** in the hierarchy of medical evidence.
- Key features like **randomization**, **control group**, and **blinding (double-blind)** help minimize bias and strengthen the validity of the findings.
*Level 2*
- Level 2 evidence typically comprises **well-designed controlled trials without randomization** (non-randomized controlled trials) or **high-quality cohort studies**.
- While strong, they do not possess the same level of internal validity as randomized controlled trials.
*Level 3*
- Level 3 evidence typically includes **case-control studies** or **cohort studies**, which are observational designs and carry a higher risk of bias compared to RCTs.
- These studies generally do not involve randomization or intervention assignment by the researchers.
*Level 4*
- Level 4 evidence is usually derived from **case series** or **poor quality cohort and case-control studies**.
- These studies provide descriptive information or investigate associations without strong control for confounding factors.
*Level 5*
- Level 5 evidence is the **lowest level of evidence**, consisting of **expert opinion** or **animal research/bench research**.
- This level lacks human clinical data or systematic investigative rigor needed for higher evidence levels.
ROC curves US Medical PG Question 2: A scientist in Boston is studying a new blood test to detect Ab to the parainfluenza virus with increased sensitivity and specificity. So far, her best attempt at creating such an exam reached 82% sensitivity and 88% specificity. She is hoping to increase these numbers by at least 2 percent for each value. After several years of work, she believes that she has actually managed to reach a sensitivity and specificity even greater than what she had originally hoped for. She travels to South America to begin testing her newest blood test. She finds 2,000 patients who are willing to participate in her study. Of the 2,000 patients, 1,200 of them are known to be infected with the parainfluenza virus. The scientist tests these 1,200 patients’ blood and finds that only 120 of them tested negative with her new test. Of the following options, which describes the sensitivity of the test?
- A. 82%
- B. 86%
- C. 98%
- D. 90% (Correct Answer)
- E. 84%
ROC curves Explanation: ***90%***
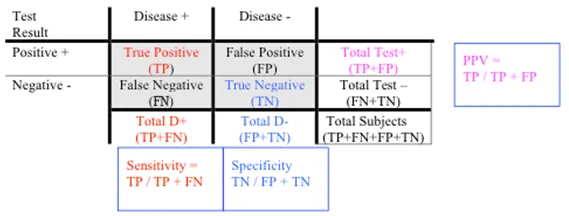
- **Sensitivity** is calculated as the number of **true positives** divided by the total number of individuals with the disease (true positives + false negatives).
- In this scenario, there were 1200 infected patients (total diseased), and 120 of them tested negative (false negatives). Therefore, 1200 - 120 = 1080 patients tested positive (true positives). The sensitivity is 1080 / 1200 = 0.90, or **90%**.
*82%*
- This value was the **original sensitivity** of the test before the scientist improved it.
- The question states that the scientist believes she has achieved a sensitivity "even greater than what she had originally hoped for."
*86%*
- This value is not directly derivable from the given data for the new test's sensitivity.
- It might represent an intermediate calculation or an incorrect interpretation of the provided numbers.
*98%*
- This would imply only 24 false negatives out of 1200 true disease cases, which is not the case (120 false negatives).
- A sensitivity of 98% would be significantly higher than the calculated 90% and the initial stated values.
*84%*
- This value is not derived from the presented data regarding the new test's performance.
- It could be mistaken for an attempt to add 2% to the original 82% sensitivity, but the actual data from the new test should be used.
ROC curves US Medical PG Question 3: An investigator is measuring the blood calcium level in a sample of female cross country runners and a control group of sedentary females. If she would like to compare the means of the two groups, which statistical test should she use?
- A. Chi-square test
- B. Linear regression
- C. t-test (Correct Answer)
- D. ANOVA (Analysis of Variance)
- E. F-test
ROC curves Explanation: ***t-test***
- A **t-test** is appropriate for comparing the means of two independent groups, such as the blood calcium levels between runners and sedentary females.
- It assesses whether the observed difference between the two sample means is statistically significant or occurred by chance.
*Chi-square test*
- The **chi-square test** is used to analyze categorical data to determine if there is a significant association between two variables.
- It is not suitable for comparing continuous variables like blood calcium levels.
*Linear regression*
- **Linear regression** is used to model the relationship between a dependent variable (outcome) and one or more independent variables (predictors).
- It aims to predict the value of a variable based on the value of another, rather than comparing means between groups.
*ANOVA (Analysis of Variance)*
- **ANOVA** is used to compare the means of **three or more independent groups**.
- Since there are only two groups being compared in this scenario, a t-test is more specific and appropriate.
*F-test*
- The **F-test** is primarily used to compare the variances of two populations or to assess the overall significance of a regression model.
- While it is the basis for ANOVA, it is not the direct test for comparing the means of two groups.
ROC curves US Medical PG Question 4: A 27-year-old man interested in pre-exposure therapy for HIV (PrEP) is being evaluated to qualify for a PrEP study. In order to qualify, patients must be HIV- and hepatitis B- and C-negative. Any other sexually transmitted infections require treatment prior to initiation of PrEP. The medical history is positive for a prior syphilis infection and bipolar affective disorder, for which he takes lithium. On his next visit, the liver and renal enzymes are within normal ranges. HIV and hepatitis B and C tests are negative. Which of the following about the HIV test is true?
- A. It is a quantitative test used for screening purposes.
- B. It is a qualitative test used for screening purposes. (Correct Answer)
- C. A secondary reagent is needed to interpret the results.
- D. A known antigen binds directly to the patient's serum.
- E. An unknown antigen binds to the known serum.
ROC curves Explanation: ***It is a qualitative test used for screening purposes.***
- **HIV screening tests** (e.g., 4th generation antibody/antigen combination assays) are typically **qualitative**, meaning they detect the presence or absence of HIV markers, not their exact amount.
- These tests are primarily used for broad **screening** of populations to identify potential cases of HIV infection.
*It is a quantitative test used for screening purposes.*
- **Quantitative tests** for HIV, such as viral load tests, measure the amount of virus in the blood and are typically used for monitoring disease progression or treatment effectiveness, not for initial screening.
- Screening tests are designed for high sensitivity to detect infection, even with low viral loads or early antibody responses, making a quantitative measurement less relevant for initial screening.
*A secondary reagent is needed to interpret the results.*
- While some complex immunoassays might involve multiple steps, modern **HIV screening tests** often use advanced technologies that directly yield results, making a separate secondary reagent for interpretation generally unnecessary.
- The results are typically indicated by a color change or a signal detected by an instrument, without requiring an additional interpretive reagent.
*A known antigen binds directly to the patient's serum.*
- **HIV antibody tests** detect **antibodies** produced by the patient's immune system in response to HIV infection.
- In such tests, **known HIV antigens** (from the test kit) bind to **HIV-specific antibodies present in the patient's serum**, not to serum components directly.
- This option is incorrect because it omits the critical role of antibodies as the target molecules being detected.
*An unknown antigen binds to the known serum.*
- This statement describes a different type of immunological assay where an unknown antigen is being identified using a known antibody, which is contrary to how **HIV screening tests** for infection are typically structured.
- **HIV screening tests** use known components (e.g., HIV antigens or antibodies) in the test kit to detect unknown components (e.g., HIV antibodies or viral antigens) in the patient's sample.
ROC curves US Medical PG Question 5: A pharmaceutical corporation is developing a research study to evaluate a novel blood test to screen for breast cancer. They enrolled 800 patients in the study, half of which have breast cancer. The remaining enrolled patients are age-matched controls who do not have the disease. Of those in the diseased arm, 330 are found positive for the test. Of the patients in the control arm, only 30 are found positive. What is this test’s sensitivity?
- A. 330 / (330 + 30)
- B. 330 / (330 + 70) (Correct Answer)
- C. 370 / (30 + 370)
- D. 370 / (70 + 370)
- E. 330 / (400 + 400)
ROC curves Explanation: ***330 / (330 + 70)***
- **Sensitivity** measures the proportion of actual **positives** that are correctly identified as such.
- In this study, there are **400 diseased patients** (half of 800). Of these, 330 tested positive (true positives), meaning 70 tested negative (false negatives). So sensitivity is **330 / (330 + 70)**.
*330 / (330 + 30)*
- This calculation represents the **positive predictive value**, which is the probability that subjects with a positive screening test truly have the disease. It uses **true positives / (true positives + false positives)**.
- It does not correctly calculate **sensitivity**, which requires knowing the total number of diseased individuals.
*370 / (30 + 370)*
- This expression is attempting to calculate **specificity**, which is the proportion of actual negatives that are correctly identified. It would be **true negatives / (true negatives + false positives)**.
- However, the numbers used are incorrect for specificity in this context given the data provided.
*370 / (70 + 370)*
- This formula is an incorrect combination of values and does not represent any standard epidemiological measure like **sensitivity** or **specificity**.
- It is attempting to combine false negatives (70) and true negatives (370 from control arm) in a non-standard way.
*330 / (400 + 400)*
- This calculation attempts to divide true positives by the total study population (800 patients).
- This metric represents the **prevalence of true positives within the entire study cohort**, not the test's **sensitivity**.
ROC curves US Medical PG Question 6: In 2013 the national mean score on the USMLE Step 1 exam was 227 with a standard deviation of 22. Assuming that the scores for 15,000 people follow a normal distribution, approximately how many students scored above the mean but below 250?
- A. 5,100 (Correct Answer)
- B. 4,500
- C. 6,000
- D. 3,750
- E. 6,750
ROC curves Explanation: ***5,100***
- To solve this, first calculate the **z-score** for 250: (250 - 227) / 22 = 1.045.
- Using a **z-table**, the area under the curve from the mean (z=0) to z=1.045 is approximately 0.353. Multiplying this by 15,000 students gives approximately **5,295 students**, which is closest to 5,100.
*4,500*
- This answer would imply a smaller proportion of students between the mean and 250 (around 30%), which is lower than the calculated z-score of 1.045 suggests.
- It does not accurately reflect the area under the **normal distribution curve** for the given range.
*6,000*
- This option would mean that approximately 40% of students scored in this range, which would correspond to a z-score much higher than 1.045 or a different standard deviation.
- This calculation overestimates the number of students within the specified range.
*3,750*
- This value represents 25% of the total students (15,000 * 0.25), indicating that only a quarter of the distribution lies in this range.
- This significantly underestimates the proportion of students scoring between the mean and 250 for the given standard deviation.
*6,750*
- This option reflects approximately 45% of the total student population (15,000 * 0.45), which would correspond to a much larger z-score or a different distribution.
- This value is an overestimation and does not align with the standard normal distribution probabilities for the given parameters.
ROC curves US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
ROC curves Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
ROC curves US Medical PG Question 8: You are reviewing raw data from a research study performed at your medical center examining the effectiveness of a novel AIDS screening examination. The study enrolled 250 patients with confirmed AIDS, and 240 of these patients demonstrated a positive screening examination. The control arm of the study enrolled 250 patients who do not have AIDS, and only 5 of these patients tested positive on the novel screening examination. What is the NPV of this novel test?
- A. 240 / (240 + 15)
- B. 240 / (240 + 5)
- C. 240 / (240 + 10)
- D. 245 / (245 + 10) (Correct Answer)
- E. 245 / (245 + 5)
ROC curves Explanation: ***245 / (245 + 10)***
- The **negative predictive value (NPV)** is calculated as **true negatives (TN)** divided by the sum of **true negatives (TN)** and **false negatives (FN)**.
- In this study, there are 250 patients with AIDS; 240 tested positive (true positives, TP), meaning 10 tested negative (false negatives, FN = 250 - 240). There are 250 patients without AIDS; 5 tested positive (false positives, FP), meaning 245 tested negative (true negatives, TN = 250 - 5). Therefore, NPV = 245 / (245 + 10).
*240 / (240 + 15)*
- This calculation incorrectly uses the number of **true positives** (240) in the numerator and denominator, which is relevant for **positive predictive value (PPV)**, not NPV.
- The denominator `(240 + 15)` does not correspond to a valid sum for calculating NPV from the given data.
*240 / (240 + 5)*
- This calculation incorrectly uses **true positives** (240) in the numerator, which is not part of the NPV formula.
- The denominator `(240 + 5)` mixes true positives and false positives, which is incorrect for NPV.
*240 / (240 + 10)*
- This incorrectly places **true positives** (240) in the numerator instead of **true negatives**.
- The denominator `(240+10)` represents **true positives + false negatives**, which is related to sensitivity, not NPV.
*245 / (245 + 5)*
- This calculation correctly identifies **true negatives** (245) in the numerator but incorrectly uses **false positives** (5) in the denominator instead of **false negatives**.
- The denominator for NPV should be **true negatives + false negatives**, which is 245 + 10.
ROC curves US Medical PG Question 9: A pharmaceutical company develops a sequential testing protocol for a rare genetic disorder (prevalence 0.01%). Initial screening test has sensitivity 95% and specificity 90%. Positive results undergo confirmatory testing with sensitivity 99% and specificity 99.5%. The company claims this approach achieves PPV >80% for the final positive result. Evaluate this claim and the rationale for sequential testing in this context.
- A. The claim is true; sequential testing increases PPV by enriching the population tested in the second step (Correct Answer)
- B. The claim is false; sensitivity decreases with sequential testing, reducing PPV
- C. Sequential testing is unnecessary; the first test alone achieves adequate PPV
- D. The claim is false; sequential testing cannot achieve PPV >80% with such low prevalence
- E. The claim is true; the high specificity of the confirmatory test ensures high PPV regardless of prevalence
ROC curves Explanation: ***The claim is true; sequential testing increases PPV by enriching the population tested in the second step***
- Sequential testing works by increasing the **pre-test probability** for the second test, as the cohort being tested has already screened positive once.
- By applying a highly specific confirmatory test to this enriched group, the number of **false positives** is significantly reduced, which drastically improves the **Positive Predictive Value (PPV)**.
*The claim is false; sequential testing cannot achieve PPV >80% with such low prevalence*
- Even with a low **prevalence**, the multiplication of specificities in a sequential process can reduce the **False Positive** rate to a level where the PPV exceeds 80%.
- This line of reasoning ignores that the **denominator** of the PPV calculation (True Positives + False Positives) decreases much faster than the numerator during the second stage.
*The claim is true; the high specificity of the confirmatory test ensures high PPV regardless of prevalence*
- While high **specificity** is crucial, PPV is always dependent on the **prevalence** (pre-test probability) of the condition in the group being tested.
- The claim is true because sequential testing specifically raises that **pre-test probability**, not because prevalence is irrelevant to the calculation.
*The claim is false; sensitivity decreases with sequential testing, reducing PPV*
- It is true that **net sensitivity** decreases in sequential testing, but a decrease in sensitivity actually tends to have a negligible effect on PPV compared to specificity gains.
- **PPV** is primarily driven by the **specificity** and the prevalence in the tested population, both of which are optimized in this two-step protocol.
*Sequential testing is unnecessary; the first test alone achieves adequate PPV*
- Given a prevalence of 0.01% and 90% specificity, the **first test** alone would yield a massive amount of false positives, resulting in a very low PPV (~0.09%).
- A **confirmatory test** is clinically and ethically necessary to avoid wrongly diagnosing thousands of healthy individuals with a **rare genetic disorder**.
ROC curves US Medical PG Question 10: A hospital system is implementing a sepsis screening algorithm using clinical criteria with sensitivity of 92% and specificity of 75%. False positives result in unnecessary antibiotics, cultures, and ICU evaluations costing $3,000 per case. Missing true sepsis cases (false negatives) results in average increased mortality and morbidity costs of $50,000 per case. Hospital sepsis prevalence is 8%. Evaluate the optimal threshold adjustment strategy.
- A. Maintain current threshold as it balances sensitivity and specificity equally
- B. Implement risk stratification with different thresholds for different populations
- C. Abandon screening due to unacceptable false positive rate
- D. Increase threshold to improve specificity and reduce costs from false positives
- E. Decrease threshold to improve sensitivity despite more false positives (Correct Answer)
ROC curves Explanation: ***Decrease threshold to improve sensitivity despite more false positives***
- In sepsis screening, the **cost of a false negative** ($50,000) is nearly 17 times higher than the **cost of a false positive** ($3,000), necessitating a strategy that prioritizes **sensitivity** to minimize missed cases.
- Lowering the threshold further ensures fewer high-cost **mortality and morbidity** events occur, which is the most economically and clinically sound approach given the significant **weighted cost** of missing a diagnosis.
*Increase threshold to improve specificity and reduce costs from false positives*
- Increasing the threshold would increase the number of **false negatives**, leading to massive financial losses due to the $50,000 cost per missed **sepsis case**.
- While it reduces the $3,000 expense of unnecessary **antibiotics and cultures**, the savings are mathematically dwarfed by the increased costs of untreated sepsis.
*Maintain current threshold as it balances sensitivity and specificity equally*
- A balanced threshold is inappropriate when the **consequences of error types** are highly asymmetrical; the algorithm should favor the side with the more severe outcome.
- Simply balancing **sensitivity and specificity** fails to account for the 8% **prevalence** and the extreme disparity in costs between false positives and false negatives.
*Implement risk stratification with different thresholds for different populations*
- While risk stratification is useful, it does not address the fundamental need to minimize **false negatives** across the entire 8% prevalence population.
- This approach adds **operational complexity** without necessarily solving the primary economic imbalance between **screening costs** and mortality costs.
*Abandon screening due to unacceptable false positive rate*
- Abandoning screening would lead to an even higher rate of **missed sepsis cases**, resulting in catastrophic clinical outcomes and **increased hospital liability**.
- The current 75% **specificity** is acceptable because the clinical priority in sepsis is **early detection** to prevent rapid physiological deterioration.
More ROC curves US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.