Diagnostic thresholds US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diagnostic thresholds. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diagnostic thresholds US Medical PG Question 1: A 36-year-old female presents to clinic inquiring about the meaning of a previous negative test result from a new HIV screening test. The efficacy of this new screening test for HIV has been assessed by comparison against existing gold standard detection of HIV RNA via PCR. The study includes 1000 patients, with 850 HIV-negative patients (by PCR) receiving a negative test result, 30 HIV-negative patients receiving a positive test result, 100 HIV positive patients receiving a positive test result, and 20 HIV positive patients receiving a negative test result. Which of the following is most likely to increase the negative predictive value for this test?
- A. Decreased prevalence of HIV in the tested population (Correct Answer)
- B. Increased prevalence of HIV in the tested population
- C. Increased number of false positive test results
- D. Increased number of false negative test results
- E. Decreased number of false positive test results
Diagnostic thresholds Explanation: ***Decreased prevalence of HIV in the tested population***
- A **lower prevalence** of a disease in the population means there are fewer actual cases, making a **negative test result** more reliable in ruling out the disease.
- This increases the probability that a person with a negative test truly does not have the disease, thus elevating the **negative predictive value (NPV)**.
*Increased prevalence of HIV in the tested population*
- A **higher prevalence** means there are more actual cases of HIV in the population.
- In this scenario, a negative test result is less reassuring, as there's a greater chance of missing a true positive case, leading to a **decreased NPV**.
*Increased number of false positive test results*
- **False positives** are instances where a test indicates disease when it's not present; they do not directly impact the ability of a negative test to predict absence of disease.
- While they affect the **positive predictive value (PPV)**, they do not directly alter the reliability of a negative result to exclude disease, so the NPV is not increased.
*Increased number of false negative test results*
- **False negatives** occur when a test indicates no disease, but the disease is actually present.
- An increase in false negatives directly implies that a negative test result is less trustworthy, leading to a **decrease in the NPV**.
*Decreased number of false positive test results*
- A decrease in false positive results primarily improves the **positive predictive value (PPV)**.
- While it indicates a more accurate test overall, it does not directly affect NPV, which measures the reliability of a negative test result in ruling out disease.
Diagnostic thresholds US Medical PG Question 2: A group of neurologists develop a new blood test for Alzheimer's. They are optimistic about the test, as they have found that for any given patient, the test repeatedly produces very similar results. However, they find that the new test results are not necessarily consistent with the gold standard of diagnosis. How would this new test most accurately be described?
- A. Valid and reliable
- B. Reliable (Correct Answer)
- C. Valid
- D. Biased
- E. Neither valid nor reliable
Diagnostic thresholds Explanation: ***Reliable***
- The test produces **similar results repeatedly** upon repeated measures, indicating high **reliability** or **precision**.
- Reliability refers to the **consistency** of a measure, even if it is not accurate.
*Valid and reliable*
- While the test is **reliable**, it is explicitly stated that the results are **not consistent with the gold standard**, meaning it lacks **validity**.
- A test must be both **consistent** (reliable) and **accurate** (valid) to be described as valid and reliable.
*Valid*
- **Validity** refers to the **accuracy** of a test, or how well it measures what it is supposed to measure.
- The test is explicitly stated to **not be consistent with the gold standard**, indicating a lack of agreement with the true measure of Alzheimer's.
*Biased*
- **Bias** refers to a **systematic error** in measurement that can lead to consistently high or low results compared to the true value.
- While the test might be biased due to its lack of consistency with the gold standard, "biased" is not the most accurate single descriptor of its measurement properties given the information provided.
*Neither valid nor reliable*
- The test is described as producing **very similar results repeatedly**, which directly indicates it has **high reliability**.
- Therefore, stating it is neither valid nor reliable is incorrect, as it possesses reliability.
Diagnostic thresholds US Medical PG Question 3: A family doctor in a rural area is treating a patient for dyspepsia. The patient had chronic heartburn and abdominal pain for the last 2 months and peptic ulcer disease due to a suspected H. pylori infection. For reasons relating to affordability and accessibility, the doctor decides to perform a diagnostic test in the office that is less invasive and more convenient. Which of the following is the most likely test used?
- A. Steiner's stain
- B. Culture of organisms from gastric specimen
- C. Stool antigen test (Correct Answer)
- D. Detection of the breakdown products of urea in biopsy
- E. Serology (ELISA testing)
Diagnostic thresholds Explanation: ***Stool antigen test***
- This **non-invasive** and **cost-effective** test detects *H. pylori* antigens in stool, making it suitable for a rural setting with limited resources.
- It is highly sensitive and specific, useful for both initial diagnosis and confirming eradication after treatment.
*Steiner's stain*
- **Steiner's stain** (Steiner silver stain) is primarily used for histological visualization of *Legionella* species, and **not for** *H. pylori* detection in routine clinical practice.
- It requires an **endoscopic biopsy**, making it more invasive and costly than the stool antigen test.
*Culture of organisms from gastric specimen*
- This method requires an **endoscopic biopsy** and specialized culture facilities, which may not be available in a rural doctor's office.
- It is more expensive and time-consuming, and primarily used when **antibiotic resistance** is suspected.
*Detection of the breakdown products of urea in biopsy*
- This refers to the **rapid urease test** (e.g., CLOtest), which is performed on a **gastric biopsy** obtained during endoscopy.
- While quick, it is an **invasive procedure** requiring endoscopy, which contradicts the patient's and doctor's preferences for a less invasive test.
*Serology (ELISA testing)*
- **Serology** detects antibodies to *H. pylori* but cannot differentiate between **active infection** and **past exposure**.
- Its utility in monitoring eradication is limited, and it's generally not recommended as the primary diagnostic test due to its inability to confirm active infection.
Diagnostic thresholds US Medical PG Question 4: An investigator is measuring the blood calcium level in a sample of female cross country runners and a control group of sedentary females. If she would like to compare the means of the two groups, which statistical test should she use?
- A. Chi-square test
- B. Linear regression
- C. t-test (Correct Answer)
- D. ANOVA (Analysis of Variance)
- E. F-test
Diagnostic thresholds Explanation: ***t-test***
- A **t-test** is appropriate for comparing the means of two independent groups, such as the blood calcium levels between runners and sedentary females.
- It assesses whether the observed difference between the two sample means is statistically significant or occurred by chance.
*Chi-square test*
- The **chi-square test** is used to analyze categorical data to determine if there is a significant association between two variables.
- It is not suitable for comparing continuous variables like blood calcium levels.
*Linear regression*
- **Linear regression** is used to model the relationship between a dependent variable (outcome) and one or more independent variables (predictors).
- It aims to predict the value of a variable based on the value of another, rather than comparing means between groups.
*ANOVA (Analysis of Variance)*
- **ANOVA** is used to compare the means of **three or more independent groups**.
- Since there are only two groups being compared in this scenario, a t-test is more specific and appropriate.
*F-test*
- The **F-test** is primarily used to compare the variances of two populations or to assess the overall significance of a regression model.
- While it is the basis for ANOVA, it is not the direct test for comparing the means of two groups.
Diagnostic thresholds US Medical PG Question 5: You conduct a medical research study to determine the screening efficacy of a novel serum marker for colon cancer. The study is divided into 2 subsets. In the first, there are 500 patients with colon cancer, of which 450 are found positive for the novel serum marker. In the second arm, there are 500 patients who do not have colon cancer, and only 10 are found positive for the novel serum marker. What is the overall sensitivity of this novel test?
- A. 450 / (450 + 10)
- B. 490 / (10 + 490)
- C. 490 / (50 + 490)
- D. 450 / (450 + 50) (Correct Answer)
- E. 490 / (450 + 490)
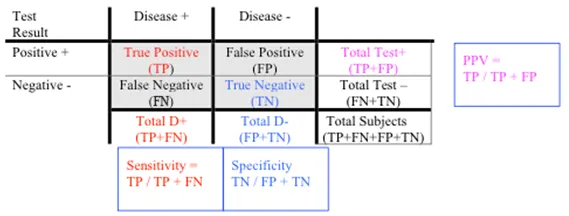
Diagnostic thresholds Explanation: ***450 / (450 + 50)***
- **Sensitivity** is defined as the proportion of actual positive cases that are correctly identified by the test.
- In this study, there are **500 patients with colon cancer** (actual positives), and **450 of them tested positive** for the marker, while **50 tested negative** (500 - 450 = 50). Therefore, sensitivity = 450 / (450 + 50) = 450/500 = 0.9 or 90%.
*450 / (450 + 10)*
- This formula represents **Positive Predictive Value (PPV)**, which is the probability that a person with a positive test result actually has the disease.
- It incorrectly uses the total number of **test positives** in the denominator (450 true positives + 10 false positives) instead of the total number of diseased individuals, which is needed for sensitivity.
*490 / (10 + 490)*
- This is actually the correct formula for **specificity**, not sensitivity.
- Specificity = TN / (FP + TN) = 490 / (10 + 490) = 490/500 = 0.98 or 98%, which measures the proportion of actual negative cases correctly identified.
- The question asks for sensitivity, not specificity.
*490 / (50 + 490)*
- This formula incorrectly mixes **true negatives (490)** with **false negatives (50)** in an attempt to calculate specificity.
- The correct specificity formula should use false positives (10), not false negatives (50), in the denominator: 490 / (10 + 490).
*490 / (450 + 490)*
- This calculation incorrectly combines **true negatives (490)** and **true positives (450)** in the denominator, which does not correspond to any standard epidemiological measure.
- Neither sensitivity nor specificity uses both true positives and true negatives in the denominator.
Diagnostic thresholds US Medical PG Question 6: A medical research study is beginning to evaluate the positive predictive value of a novel blood test for non-Hodgkin’s lymphoma. The diagnostic arm contains 700 patients with NHL, of which 400 tested positive for the novel blood test. In the control arm, 700 age-matched control patients are enrolled and 0 are found positive for the novel test. What is the PPV of this test?
- A. 400 / (400 + 0) (Correct Answer)
- B. 700 / (700 + 300)
- C. 400 / (400 + 300)
- D. 700 / (700 + 0)
- E. 700 / (400 + 400)
Diagnostic thresholds Explanation: ***400 / (400 + 0) = 1.0 or 100%***
- The **positive predictive value (PPV)** is calculated as **True Positives / (True Positives + False Positives)**.
- In this scenario, **True Positives (TP)** are the 400 patients with NHL who tested positive, and **False Positives (FP)** are 0, as no control patients tested positive.
- This gives a PPV of 400/400 = **1.0 or 100%**, indicating that all patients who tested positive actually had the disease.
*700 / (700 + 300)*
- This calculation does not align with the formula for PPV based on the given data.
- The denominator `(700+300)` suggests an incorrect combination of various patient groups.
*400 / (400 + 300)*
- The denominator `(400+300)` incorrectly includes 300, which is the number of **False Negatives** (patients with NHL who tested negative), not False Positives.
- PPV focuses on the proportion of true positives among all positive tests, not all diseased individuals.
*700 / (700 + 0)*
- This calculation incorrectly uses the total number of patients with NHL (700) as the numerator, rather than the number of positive test results in that group.
- The numerator should be the **True Positives** (400), not the total number of diseased individuals.
*700 / (400 + 400)*
- This calculation uses incorrect values for both the numerator and denominator, not corresponding to the PPV formula.
- The numerator 700 represents the total number of patients with the disease, not those who tested positive, and the denominator incorrectly sums up values that don't represent the proper PPV calculation.
Diagnostic thresholds US Medical PG Question 7: A student health coordinator plans on leading a campus-wide HIV screening program that will be free for the entire undergraduate student body. The goal is to capture as many correct HIV diagnoses as possible with the fewest false positives. The coordinator consults with the hospital to see which tests are available to use for this program. Test A has a sensitivity of 0.92 and a specificity of 0.99. Test B has a sensitivity of 0.95 and a specificity of 0.96. Test C has a sensitivity of 0.98 and a specificity of 0.93. Which of the following testing schemes should the coordinator pursue?
- A. Test A on the entire student body followed by Test B on those who are positive
- B. Test A on the entire student body followed by Test C on those who are positive
- C. Test C on the entire student body followed by Test B on those who are positive
- D. Test C on the entire student body followed by Test A on those who are positive (Correct Answer)
- E. Test B on the entire student body followed by Test A on those who are positive
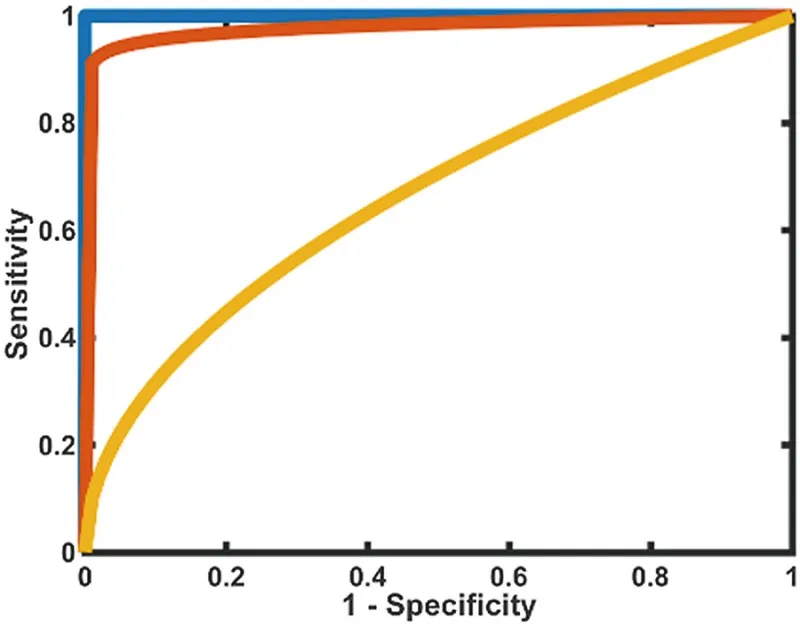
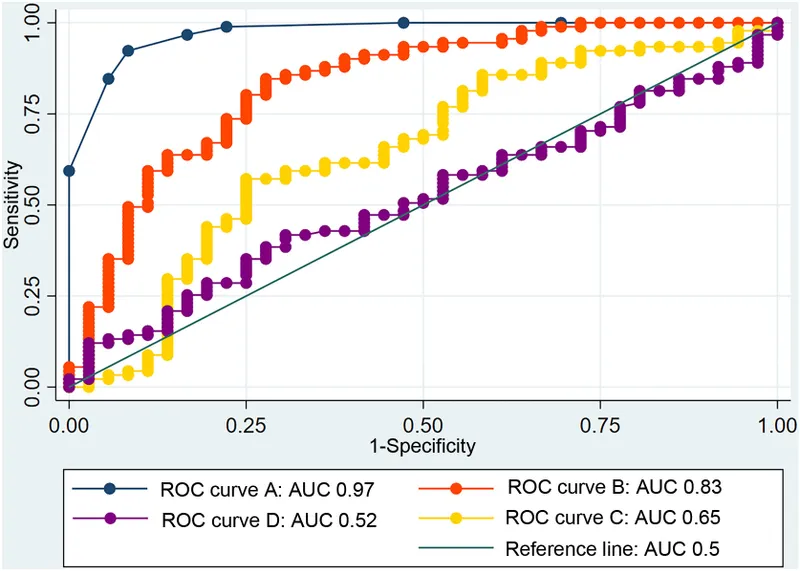
Diagnostic thresholds Explanation: ***Test C on the entire student body followed by Test A on those who are positive***
- To "capture as many correct HIV diagnoses as possible" (maximize true positives), the initial screening test should have the **highest sensitivity**. Test C has the highest sensitivity (0.98).
- To "capture as few false positives as possible" (maximize true negatives and confirm diagnoses), the confirmatory test should have the **highest specificity**. Test A has the highest specificity (0.99).
*Test A on the entire student body followed by Test B on those who are positive*
- Starting with Test A (sensitivity 0.92) would miss more true positive cases than starting with Test C (sensitivity 0.98), failing the goal of **capturing as many cases as possible**.
- Following with Test B (specificity 0.96) would result in more false positives than following with Test A (specificity 0.99).
*Test A on the entire student body followed by Test C on those who are positive*
- This scheme would miss many true positive cases initially due to Test A's lower sensitivity compared to Test C.
- Following with Test C would introduce more false positives than necessary, as it has a lower specificity (0.93) than Test A (0.99).
*Test C on the entire student body followed by Test B on those who are positive*
- While Test C is a good initial screen for its high sensitivity, following it with Test B (specificity 0.96) is less optimal than Test A (specificity 0.99) for minimizing false positives in the confirmation step.
- This combination would therefore yield more false positives in the confirmatory stage than using Test A.
*Test B on the entire student body followed by Test A on those who are positive*
- Test B has a sensitivity of 0.95, which is lower than Test C's sensitivity of 0.98, meaning it would miss more true positive cases at the initial screening stage.
- While Test A provides excellent specificity for confirmation, the initial screening step is suboptimal for the goal of capturing as many diagnoses as possible.
Diagnostic thresholds US Medical PG Question 8: A pharmaceutical corporation is developing a research study to evaluate a novel blood test to screen for breast cancer. They enrolled 800 patients in the study, half of which have breast cancer. The remaining enrolled patients are age-matched controls who do not have the disease. Of those in the diseased arm, 330 are found positive for the test. Of the patients in the control arm, only 30 are found positive. What is this test’s sensitivity?
- A. 330 / (330 + 30)
- B. 330 / (330 + 70) (Correct Answer)
- C. 370 / (30 + 370)
- D. 370 / (70 + 370)
- E. 330 / (400 + 400)
Diagnostic thresholds Explanation: ***330 / (330 + 70)***
- **Sensitivity** measures the proportion of actual **positives** that are correctly identified as such.
- In this study, there are **400 diseased patients** (half of 800). Of these, 330 tested positive (true positives), meaning 70 tested negative (false negatives). So sensitivity is **330 / (330 + 70)**.
*330 / (330 + 30)*
- This calculation represents the **positive predictive value**, which is the probability that subjects with a positive screening test truly have the disease. It uses **true positives / (true positives + false positives)**.
- It does not correctly calculate **sensitivity**, which requires knowing the total number of diseased individuals.
*370 / (30 + 370)*
- This expression is attempting to calculate **specificity**, which is the proportion of actual negatives that are correctly identified. It would be **true negatives / (true negatives + false positives)**.
- However, the numbers used are incorrect for specificity in this context given the data provided.
*370 / (70 + 370)*
- This formula is an incorrect combination of values and does not represent any standard epidemiological measure like **sensitivity** or **specificity**.
- It is attempting to combine false negatives (70) and true negatives (370 from control arm) in a non-standard way.
*330 / (400 + 400)*
- This calculation attempts to divide true positives by the total study population (800 patients).
- This metric represents the **prevalence of true positives within the entire study cohort**, not the test's **sensitivity**.
Diagnostic thresholds US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Diagnostic thresholds Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Diagnostic thresholds US Medical PG Question 10: A pharmaceutical company develops a sequential testing protocol for a rare genetic disorder (prevalence 0.01%). Initial screening test has sensitivity 95% and specificity 90%. Positive results undergo confirmatory testing with sensitivity 99% and specificity 99.5%. The company claims this approach achieves PPV >80% for the final positive result. Evaluate this claim and the rationale for sequential testing in this context.
- A. The claim is true; sequential testing increases PPV by enriching the population tested in the second step (Correct Answer)
- B. The claim is false; sensitivity decreases with sequential testing, reducing PPV
- C. Sequential testing is unnecessary; the first test alone achieves adequate PPV
- D. The claim is false; sequential testing cannot achieve PPV >80% with such low prevalence
- E. The claim is true; the high specificity of the confirmatory test ensures high PPV regardless of prevalence
Diagnostic thresholds Explanation: ***The claim is true; sequential testing increases PPV by enriching the population tested in the second step***
- Sequential testing works by increasing the **pre-test probability** for the second test, as the cohort being tested has already screened positive once.
- By applying a highly specific confirmatory test to this enriched group, the number of **false positives** is significantly reduced, which drastically improves the **Positive Predictive Value (PPV)**.
*The claim is false; sequential testing cannot achieve PPV >80% with such low prevalence*
- Even with a low **prevalence**, the multiplication of specificities in a sequential process can reduce the **False Positive** rate to a level where the PPV exceeds 80%.
- This line of reasoning ignores that the **denominator** of the PPV calculation (True Positives + False Positives) decreases much faster than the numerator during the second stage.
*The claim is true; the high specificity of the confirmatory test ensures high PPV regardless of prevalence*
- While high **specificity** is crucial, PPV is always dependent on the **prevalence** (pre-test probability) of the condition in the group being tested.
- The claim is true because sequential testing specifically raises that **pre-test probability**, not because prevalence is irrelevant to the calculation.
*The claim is false; sensitivity decreases with sequential testing, reducing PPV*
- It is true that **net sensitivity** decreases in sequential testing, but a decrease in sensitivity actually tends to have a negligible effect on PPV compared to specificity gains.
- **PPV** is primarily driven by the **specificity** and the prevalence in the tested population, both of which are optimized in this two-step protocol.
*Sequential testing is unnecessary; the first test alone achieves adequate PPV*
- Given a prevalence of 0.01% and 90% specificity, the **first test** alone would yield a massive amount of false positives, resulting in a very low PPV (~0.09%).
- A **confirmatory test** is clinically and ethically necessary to avoid wrongly diagnosing thousands of healthy individuals with a **rare genetic disorder**.
More Diagnostic thresholds US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.