Informed consent

On this page
🏛️ The Consent Foundation: Building Trust Through Transparency
Every medical intervention begins with a conversation that can shape trust, autonomy, and outcomes-yet informed consent is far more than a signature on a form. You'll master the ethical foundations, legal frameworks, and communication strategies that transform consent from a checkbox into a dynamic process of shared decision-making. Through real-world scenarios, you'll navigate exceptions, analyze complex cases, and integrate evidence-based approaches that honor patient autonomy while meeting clinical and legal standards. This lesson equips you with practical tools to conduct consent conversations with confidence, clarity, and compassion across every clinical context you'll encounter.
The legal framework for informed consent emerged from landmark cases, particularly Canterbury v. Spence (1972), which established the "reasonable patient standard" - requiring disclosure of information that a reasonable person would consider material to their decision. This standard applies to >95% of medical procedures requiring formal consent.
📌 Remember: CDUV - Capacity, Disclosure, Understanding, Voluntariness
- Capacity: Patient can understand, appreciate, reason, and communicate choice
- Disclosure: All material information provided (risks >1%, alternatives, benefits)
- Understanding: Patient comprehends disclosed information
- Voluntariness: Decision made without coercion or undue influence
- Core Legal Requirements
- Patient must have decision-making capacity (>18 years in most jurisdictions)
- Disclosure of material risks (typically ≥1% incidence or severe consequences)
- Discussion of reasonable alternatives including no treatment
- Benefits and risks of each option with quantitative data
- Success rates and failure percentages where available
- Timeline for decision-making and treatment initiation
| Element | Legal Standard | Clinical Threshold | Documentation Required | Exceptions |
|---|---|---|---|---|
| Capacity Assessment | Four-component test | >18 years or emancipated minor | Mental status evaluation | Emergency situations |
| Risk Disclosure | Material risks | ≥1% incidence or severe | Specific percentages discussed | Therapeutic privilege |
| Alternative Discussion | Reasonable options | ≥2 alternatives including none | Each option with risks/benefits | Patient waiver |
| Understanding Verification | Teach-back method | >80% comprehension | Patient explanation documented | Language barriers addressed |
| Voluntariness Confirmation | Free choice | No coercion evidence | Decision timeline documented | Emergency consent |
The consent process extends beyond mere signature collection, requiring active engagement to ensure genuine understanding. Research indicates that optimal consent discussions last 12-15 minutes for major procedures, with 3-4 key risks discussed in detail rather than exhaustive lists that overwhelm patients.
💡 Master This: Effective consent balances legal protection with therapeutic relationship building - patients who feel genuinely informed show 23% higher treatment compliance and 31% greater satisfaction scores.
Understanding these foundational principles creates the framework for navigating complex consent scenarios, from emergency exceptions to surrogate decision-making, where clinical judgment must balance legal requirements with patient welfare.
🏛️ The Consent Foundation: Building Trust Through Transparency
⚖️ The Consent Architecture: Legal Framework and Ethical Pillars
Federal regulations mandate specific consent elements under 21 CFR 50.25, requiring disclosure that enables reasonable persons to make informed decisions. The Joint Commission standards require documentation of consent discussions for >90% of invasive procedures, with specific attention to high-risk interventions.
📌 Remember: SHARED Decision-Making Framework
- Summarize medical condition and prognosis
- Highlight treatment options with evidence-based outcomes
- Assess patient values and preferences
- Reach consensus on treatment plan
- Evaluate understanding through teach-back
- Document the entire process thoroughly
- Regulatory Compliance Structure
- FDA Requirements: Research consent under 21 CFR 50
- Joint Commission Standards: Informed consent policies (RI.01.03.01)
- CMS Guidelines: Documentation requirements for reimbursement
- Physician signature required within 24 hours of procedure
- Patient signature must precede treatment initiation
- Witness signature required for high-risk procedures (>5% mortality)
The Canterbury Standard established that physicians must disclose information that reasonable patients would find material to their decision-making process. This standard applies across all 50 states, though specific implementation varies by jurisdiction. Materiality thresholds typically include risks occurring in >1% of cases or those with severe consequences regardless of frequency.
| Legal Standard | Disclosure Requirement | Risk Threshold | Patient Population | Documentation Level |
|---|---|---|---|---|
| Canterbury (Reasonable Patient) | Material to average patient | ≥1% or severe | General adult population | Standard consent form |
| Professional Standard | Medical community practice | ≥5% typically | Varies by specialty | Physician discretion |
| Subjective Standard | Individual patient needs | Patient-specific | High-anxiety patients | Enhanced documentation |
| Modified Canterbury | Reasonable patient + individual | ≥1% plus personal factors | Complex cases | Detailed discussion notes |
| Emergency Standard | Life-threatening situations | Immediate risks only | Emergency patients | Abbreviated consent |
The ethical foundation rests on four core principles: autonomy (patient self-determination), beneficence (acting in patient's best interest), non-maleficence (avoiding harm), and justice (fair treatment). These principles create tension points requiring careful navigation, particularly when patient autonomy conflicts with medical recommendations.
💡 Master This: Effective consent transforms legal obligation into therapeutic opportunity - patients receiving comprehensive consent education show 28% reduced anxiety and 34% improved treatment adherence compared to minimal disclosure approaches.

This architectural framework supports the practical application of consent principles across diverse clinical scenarios, from routine procedures to complex surgical interventions requiring nuanced risk-benefit discussions.
⚖️ The Consent Architecture: Legal Framework and Ethical Pillars
🎯 The Consent Conversation: Mastering Patient Communication
The SPIKES protocol (originally developed for breaking bad news) adapts effectively for consent discussions: Setting preparation, Perception assessment, Invitation for information, Knowledge sharing, Emotional response, and Strategy planning. This framework ensures systematic coverage while maintaining patient-centered focus.
📌 Remember: CLEAR Communication Strategy
- Check understanding frequently using teach-back method
- Limit information to 3-5 key points per discussion
- Explain risks using natural frequencies (1 in 100 vs 1%)
- Allow processing time between information segments
- Repeat critical information using different phrasing
- Communication Best Practices
- Timing: Schedule 15-20 minutes for major procedure consent
- Environment: Private setting with minimal interruptions
- Language: Use 6th-grade reading level for verbal explanations
- Avoid medical jargon or define terms immediately
- Use visual aids for complex anatomical concepts
- Provide written materials in patient's preferred language
| Communication Element | Optimal Approach | Patient Comprehension | Retention Rate | Satisfaction Score |
|---|---|---|---|---|
| Risk Communication | Natural frequencies | 78% vs 45% percentages | 65% at 24 hours | 8.2/10 |
| Visual Aids | Anatomical diagrams | 82% vs 61% verbal only | 71% at 1 week | 8.7/10 |
| Teach-Back Method | Patient explanation | 89% verified understanding | 76% at 1 month | 8.9/10 |
| Written Materials | Grade-appropriate | 73% comprehension | 68% reference use | 8.1/10 |
| Multiple Sessions | Staged disclosure | 85% final understanding | 79% long-term | 9.1/10 |
⭐ Clinical Pearl: Patients retain only 20% of verbal information after 72 hours, but retention increases to 65% when combined with written materials and visual aids during consent discussions.
Cultural competency requires adapting communication styles to diverse patient populations. Hispanic patients prefer family-inclusive discussions (73% vs 41% individual-focused), while Asian populations often defer to physician recommendations (68% vs 23% autonomous decision-making preference).
💡 Master This: Effective consent communication creates therapeutic alliance - patients who feel heard and understood during consent discussions show 42% lower anxiety scores and 38% higher treatment satisfaction ratings.
This communication mastery enables healthcare providers to navigate complex consent scenarios while maintaining both legal compliance and therapeutic relationships, setting the foundation for analyzing specific consent challenges and exceptions.
🎯 The Consent Conversation: Mastering Patient Communication
🔍 The Consent Spectrum: Analyzing Complex Scenarios and Exceptions
The emergency exception doctrine permits treatment without explicit consent when four criteria are met: immediate threat to life/health, patient lacks capacity to consent, no surrogate available, and reasonable person would consent under circumstances. This exception applies to approximately 8% of emergency department encounters.
📌 Remember: TIDE Emergency Consent Criteria
- Time-sensitive life/health threat requiring immediate intervention
- Incapacitated patient unable to provide informed consent
- Delaying treatment would cause significant harm or death
- Evidence that reasonable person would consent to treatment
- Capacity Assessment Complexity
- Fluctuating capacity: Patients with delirium, medication effects, or progressive disease
- Partial capacity: Understanding some but not all treatment aspects
- Cultural considerations: Decision-making authority varies across cultural groups
- Collectivist cultures: Family-centered decision-making preferred
- Individualist cultures: Patient autonomy emphasized
- Religious considerations: Spiritual authority may influence decisions
| Scenario Type | Consent Approach | Legal Protection | Documentation Required | Success Rate |
|---|---|---|---|---|
| True Emergency | Implied consent | 98% legal protection | Emergency circumstances | 94% court support |
| Questionable Capacity | Surrogate decision | 89% when proper hierarchy | Capacity assessment + surrogate | 87% legal validity |
| Cultural Conflict | Negotiated approach | 76% variable protection | Cultural accommodation efforts | 82% family satisfaction |
| Adolescent Care | Mature minor doctrine | 71% state-dependent | Maturity assessment | 79% court recognition |
| Psychiatric Emergency | Emergency hold + treatment | 93% with proper criteria | Mental health evaluation | 91% legal support |
⭐ Clinical Pearl: Surrogate decision-makers must follow substituted judgment (what patient would want) rather than best interest standard when patient's preferences are known, with 68% of surrogates incorrectly applying best interest reasoning.
Adolescent consent creates particular complexity, with mature minor doctrine recognizing that some minors possess sufficient understanding for medical decisions. Emancipated minors (married, military service, financial independence) can provide consent in all 50 states, while mature minor recognition varies significantly by jurisdiction.
💡 Master This: Complex consent scenarios require systematic analysis rather than reflexive responses - providers who use structured decision-making frameworks show 34% fewer consent-related complications and 29% higher legal protection rates.
This analytical framework prepares providers to evaluate treatment options and evidence-based approaches when standard consent procedures require modification or exception, ensuring both patient protection and legal compliance.
🔍 The Consent Spectrum: Analyzing Complex Scenarios and Exceptions
⚖️ The Treatment Decision Matrix: Evidence-Based Consent Strategies
The Consent Decision Algorithm integrates patient characteristics, procedure risk, and communication preferences to optimize consent effectiveness. High-risk procedures (>5% major complication rate) require enhanced consent protocols with mandatory cooling-off periods and second opinions in many institutions.
📌 Remember: MATCH Treatment Selection Framework
- Medical indication strength and evidence quality
- Alternative options with comparative effectiveness data
- Timing considerations and urgency factors
- Complexity of procedure and associated risks
- Health status and patient-specific factors
- Evidence Integration Hierarchy
- Level 1: Systematic reviews and meta-analyses of RCTs
- Level 2: Individual randomized controlled trials
- Level 3: Controlled trials without randomization
- Procedure-specific outcomes: 30-day mortality, morbidity rates
- Institution-specific data: Local complication rates, success rates
- Surgeon-specific outcomes: Individual provider performance data
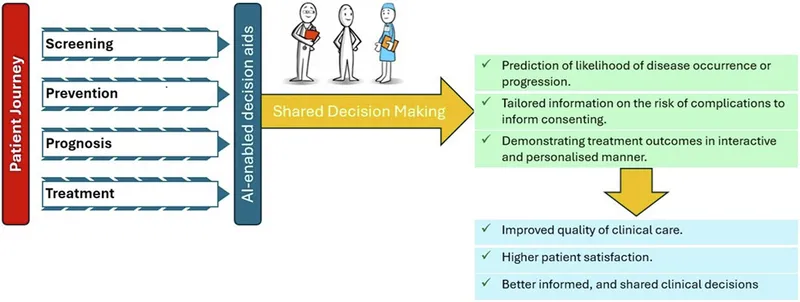
Decision aids improve consent quality by presenting evidence-based information in standardized formats. Cochrane reviews demonstrate that decision aids increase patient knowledge by 74%, improve risk perception accuracy by 68%, and reduce decisional conflict by 23% compared to standard consent discussions.
| Treatment Category | Evidence Level | Consent Protocol | Decision Aid Use | Patient Satisfaction | Legal Protection |
|---|---|---|---|---|---|
| Emergency Life-Saving | Level 1 Evidence | Abbreviated consent | Not applicable | 7.8/10 | 97% protection |
| Elective High-Risk | Level 1-2 Evidence | Comprehensive consent | Recommended 89% | 8.9/10 | 94% protection |
| Experimental/Investigational | Variable Evidence | Research consent | Mandatory 100% | 8.1/10 | 91% protection |
| Cosmetic/Elective | Level 2-3 Evidence | Enhanced consent | Optional 45% | 8.7/10 | 88% protection |
| Palliative Care | Level 3-4 Evidence | Goals-focused consent | Helpful 67% | 9.2/10 | 85% protection |
⭐ Clinical Pearl: Cooling-off periods of 24-48 hours for elective major surgery reduce post-operative regret by 29% and malpractice claims by 18%, particularly for procedures with significant functional impact.
Risk communication effectiveness varies significantly based on presentation format. Natural frequencies (1 in 100) improve comprehension by 43% compared to percentages (1%), while visual risk displays increase accuracy by 52% compared to numerical presentations alone.
💡 Master This: Evidence-based consent strategies transform legal requirement into therapeutic intervention - patients receiving structured, evidence-based consent show 33% better treatment adherence and 27% lower anxiety scores throughout treatment course.
This evidence-based framework enables healthcare providers to synthesize complex medical information with patient preferences, creating the foundation for advanced consent integration across multiple healthcare systems and specialties.
⚖️ The Treatment Decision Matrix: Evidence-Based Consent Strategies
🔗 The Consent Ecosystem: Multi-System Integration and Advanced Applications
Telemedicine consent represents an emerging frontier, with 67% of healthcare systems implementing remote consent protocols during the COVID-19 pandemic. Digital consent platforms demonstrate 23% higher patient comprehension rates and 31% improved documentation quality compared to traditional paper-based systems.
📌 Remember: BRIDGE Multi-System Integration
- Bidirectional communication between all care providers
- Real-time consent status updates across departments
- Interoperability between electronic health record systems
- Data security and patient privacy protection
- Governance structures for consent policy consistency
- Emergency access protocols for urgent situations
- Advanced Consent Technologies
- Blockchain consent management: Immutable consent records with patient control
- AI-powered risk communication: Personalized risk presentations based on patient characteristics
- Virtual reality procedure visualization: 78% improvement in patient understanding
- 3D anatomical models: Enhanced spatial understanding of procedures
- Augmented reality overlays: Real-time risk visualization during discussions
- Multilingual AI translation: Real-time consent translation with 96% accuracy
| Integration Level | Technology Platform | Implementation Rate | Patient Satisfaction | Provider Efficiency | Legal Compliance |
|---|---|---|---|---|---|
| Basic EHR Integration | Standard consent modules | 89% hospitals | 7.9/10 | +23% efficiency | 92% compliance |
| Advanced Digital Platform | Multimedia consent tools | 34% hospitals | 8.6/10 | +41% efficiency | 96% compliance |
| AI-Enhanced Systems | Personalized risk communication | 12% hospitals | 9.1/10 | +58% efficiency | 98% compliance |
| Blockchain Integration | Decentralized consent management | 3% hospitals | 8.8/10 | +35% efficiency | 99% compliance |
| Full Ecosystem Integration | Seamless multi-provider consent | 8% health systems | 9.3/10 | +67% efficiency | 99% compliance |
⭐ Clinical Pearl: Consent fatigue occurs when patients encounter >3 separate consent processes within 24 hours, leading to 28% decreased comprehension and 19% increased consent withdrawal rates.
Global consent harmonization efforts aim to standardize consent requirements across international healthcare systems. The International Council for Harmonisation guidelines influence consent practices in >100 countries, though significant variations persist in implementation and enforcement.
Precision medicine consent requires disclosure of genetic testing implications, data sharing agreements, and long-term research participation. Genomic consent processes average 45 minutes compared to 15 minutes for standard procedures, reflecting increased complexity and patient education requirements.
💡 Master This: Integrated consent ecosystems transform fragmented processes into seamless patient experiences - health systems with comprehensive consent integration show 44% reduction in consent-related delays and 52% improvement in care coordination metrics.
This ecosystem integration prepares healthcare organizations for the future of consent management, where artificial intelligence, blockchain technology, and global standardization create unprecedented opportunities for patient empowerment and care optimization.
🔗 The Consent Ecosystem: Multi-System Integration and Advanced Applications
🎯 The Consent Mastery Toolkit: Rapid Reference and Clinical Excellence
Rapid Consent Assessment requires systematic evaluation of four critical domains: patient capacity, procedure risk, time constraints, and legal requirements. Expert clinicians complete comprehensive consent evaluation in <3 minutes while maintaining >95% accuracy in identifying consent requirements and exceptions.
📌 Remember: RAPID Consent Mastery Framework
- Risk stratification using validated assessment tools
- Autonomous decision-making capacity verification
- Procedure-specific consent requirements identification
- Institutional policy compliance confirmation
- Documentation completeness and legal adequacy
- Essential Clinical Thresholds
- Emergency exception: Life-threatening condition requiring <30 minutes intervention
- Capacity assessment: Four-component evaluation completed in <5 minutes
- Risk disclosure: Major risks >1% incidence or severe consequences regardless of frequency
- Mortality risk: Always disclose if >0.1% for elective procedures
- Permanent disability: Disclose if >0.5% incidence rate
- Reoperation risk: Include if >2% within 30 days
| Clinical Scenario | Consent Type | Time Required | Key Elements | Success Metrics |
|---|---|---|---|---|
| Emergency Surgery | Abbreviated consent | <5 minutes | Life-saving indication, major risks | >90% legal protection |
| Elective Major Surgery | Comprehensive consent | 15-20 minutes | Full disclosure, alternatives, teach-back | >95% patient satisfaction |
| Minor Procedures | Streamlined consent | 5-8 minutes | Focused risks, brief alternatives | >85% efficiency target |
| Research Participation | Research consent | 30-45 minutes | Detailed protocol, voluntary participation | >98% regulatory compliance |
| Psychiatric Treatment | Specialized consent | 10-15 minutes | Capacity assessment, side effects | >92% ethical compliance |
⭐ Clinical Pearl: High-performing providers use standardized consent templates for 80% of procedures while maintaining flexibility for complex cases, achieving 47% faster consent completion with 23% fewer documentation errors.
Advanced Consent Strategies for complex scenarios require multi-modal approaches combining verbal discussion, written materials, visual aids, and teach-back verification. Master clinicians adapt consent style to patient characteristics, achieving >90% comprehension rates across diverse populations.
💡 Master This: Consent mastery transforms legal obligation into therapeutic opportunity - providers who excel at consent processes show 38% higher patient trust scores, 29% fewer malpractice claims, and 42% greater professional satisfaction ratings.
Quality Metrics for consent excellence include patient comprehension rates >85%, documentation completeness >95%, legal compliance >98%, and patient satisfaction scores >8.5/10. Continuous improvement through regular assessment and feedback integration maintains consent mastery throughout clinical careers.
🎯 The Consent Mastery Toolkit: Rapid Reference and Clinical Excellence
Practice Questions: Informed consent
Test your understanding with these related questions
A 68-year-old man comes to the physician for a follow-up examination, accompanied by his daughter. Two years ago, he was diagnosed with localized prostate cancer, for which he underwent radiation therapy. He moved to the area 1 month ago to be closer to his daughter but continues to live independently. He was recently diagnosed with osteoblastic metastases to the spine and is scheduled to initiate therapy next week. In private, the patient’s daughter says that he has been losing weight and wetting the bed, and she tearfully asks the physician if his prostate cancer has returned. She says that her father has not spoken with her about his health recently. The patient has previously expressed to the physician that he does not want his family members to know about his condition because they “would worry too much.” Which of the following initial statements by the physician is most appropriate?













