Principles of medical ethics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Principles of medical ethics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Principles of medical ethics US Medical PG Question 1: A 79-year-old male presents to your office for his annual flu shot. On physical exam you note several linear bruises on his back. Upon further questioning he denies abuse from his daughter and son-in-law, who live in the same house. The patient states he does not want this information shared with anyone. What is the most appropriate next step, paired with its justification?
- A. Breach patient confidentiality, as this patient's care should be discussed with the daughter as she is his primary caregiver
- B. See the patient back in 2 weeks and assess whether the patient's condition has improved, as his condition is not severe
- C. Do not break patient confidentiality, as elder abuse reporting is not mandatory
- D. Do not break patient confidentiality, as this would potentially worsen the situation
- E. Breach patient confidentiality, as this patient is a potential victim of elder abuse and reporting is mandated in most states (Correct Answer)
Principles of medical ethics Explanation: ***Breach patient confidentiality, as this patient is a potential victim of elder abuse and reporting is mandated in most states***
- As a physician, there is a **legal and ethical obligation** to report suspected elder abuse in most US states, even when the patient denies it and requests confidentiality.
- Physicians are typically **mandatory reporters** under state law, and must report to Adult Protective Services or law enforcement when elder abuse is suspected.
- The patient's safety and legal requirements outweigh the right to confidentiality in jurisdictions with mandatory reporting laws.
*Breach patient confidentiality, as this patient's care should be discussed with the daughter as she is his primary caregiver*
- Breaching confidentiality to discuss this with the daughter would be inappropriate, especially since the daughter and son-in-law are the **suspected abusers**.
- Discussing with the primary caregiver is only appropriate if the patient has given **explicit consent** and there are no suspicions of abuse from that caregiver.
*See the patient back in 2 weeks and assess whether the patient's condition has improved, as his condition is not severe*
- This option is inappropriate because it delays intervention in a potentially **dangerous situation**.
- Suspected abuse warrants **immediate action** to ensure the patient's safety, regardless of the perceived severity of current injuries.
*Do not break patient confidentiality, as elder abuse reporting is not mandatory*
- In **most states**, physicians have **mandatory reporting laws** for elder abuse, making this statement generally incorrect.
- Physicians are typically considered "mandated reporters" and are legally required to report suspected abuse to the appropriate authorities in their jurisdiction.
*Do not break patient confidentiality, as this would potentially worsen the situation*
- While this is a valid concern in some situations, the **primary responsibility** of a physician is to protect vulnerable patients from harm.
- Reporting suspected abuse initiates protective measures and is legally required in most states, as the potential benefit of intervention outweighs the risk of worsening the situation.
Principles of medical ethics US Medical PG Question 2: A 76-year-old man is brought to the hospital after having a stroke. Head CT is done in the emergency department and shows intracranial hemorrhage. Upon arrival to the ED he is verbally non-responsive and withdraws only to pain. He does not open his eyes. He is transferred to the medical ICU for further management and intubated for airway protection. During his second day in the ICU, his blood pressure is measured as 91/54 mmHg and pulse is 120/min. He is given fluids and antibiotics, but he progresses to renal failure and his mental status deteriorates. The physicians in the ICU ask the patient’s family what his wishes are for end-of-life care. His wife tells the team that she is durable power of attorney for the patient and provides appropriate documentation. She mentions that he did not have a living will, but she believes that he would want care withdrawn in this situation, and therefore asks the team to withdraw care at this point. The patient’s daughter vehemently disagrees and believes it is in the best interest of her father, the patient, to continue all care. Based on this information, what is the best course of action for the physician team?
- A. Call other family members and consult them for their opinions
- B. Listen to the patient’s daughter’s wishes and continue all care
- C. Compromise between the wife and daughter and withdraw the fluids and antibiotics but keep the patient intubated
- D. Listen to the patient’s wife’s wishes and withdraw care (Correct Answer)
- E. Consult the hospital ethics committee and continue all care until a decision is reached
Principles of medical ethics Explanation: ***Listen to the patient’s wife’s wishes and withdraw care***
- The **durable power of attorney for healthcare** legally designates the wife as the patient's surrogate decision-maker when the patient lacks capacity, overriding other family opinions.
- In the absence of a living will, the **surrogate's interpretation of the patient's best interests** and previously expressed wishes is legally and ethically binding.
*Call other family members and consult them for their opinions*
- While involving family is good practice in general, the presence of a **legally appointed durable power of attorney** means that other family members' opinions do not supersede the designated surrogate's decisions.
- Consulting other family members could **create more conflict and delay** crucial decisions, as the wife holds the legal authority.
*Listen to the patient’s daughter’s wishes and continue all care*
- The daughter's wishes, while understandable, **do not hold legal authority** over the decisions of the legally appointed durable power of attorney.
- Disregarding the wife's authority would be a **breach of ethical and legal obligations** in patient care.
*Compromise between the wife and daughter and withdraw the fluids and antibiotics but keep the patient intubated*
- A compromise that goes against the legal surrogate's explicitly stated decision (to withdraw all care) is **ethically problematic and legally unsound**.
- Healthcare decisions should be based on the patient's best interest as interpreted by the **authorized surrogate**, not on attempting to please all family members.
*Consult the hospital ethics committee and continue all care until a decision is reached*
- While an ethics committee consult is appropriate if there's **disagreement over the interpretation of the patient's wishes** *among legally designated surrogates* or concerns about the surrogate's decision-making capacity, it's not the first step when a clear legal surrogate with documentation is present and makes a decision.
- Continuing all care against the wishes of the **legal proxy** would be contrary to patient autonomy and the principles of substituted judgment.
Principles of medical ethics US Medical PG Question 3: A 42-year-old woman presents to the physician with symptoms of vague abdominal pain and bloating for several months. Test results indicate that she has ovarian cancer. Her physician attempts to reach her by phone multiple times but cannot reach her. Next of kin numbers are in her chart. According to HIPAA regulations, who should be the primary person the doctor discusses this information with?
- A. The patient's brother
- B. The patient's husband
- C. The patient's daughter
- D. All of the options
- E. The patient (Correct Answer)
Principles of medical ethics Explanation: ***The patient***
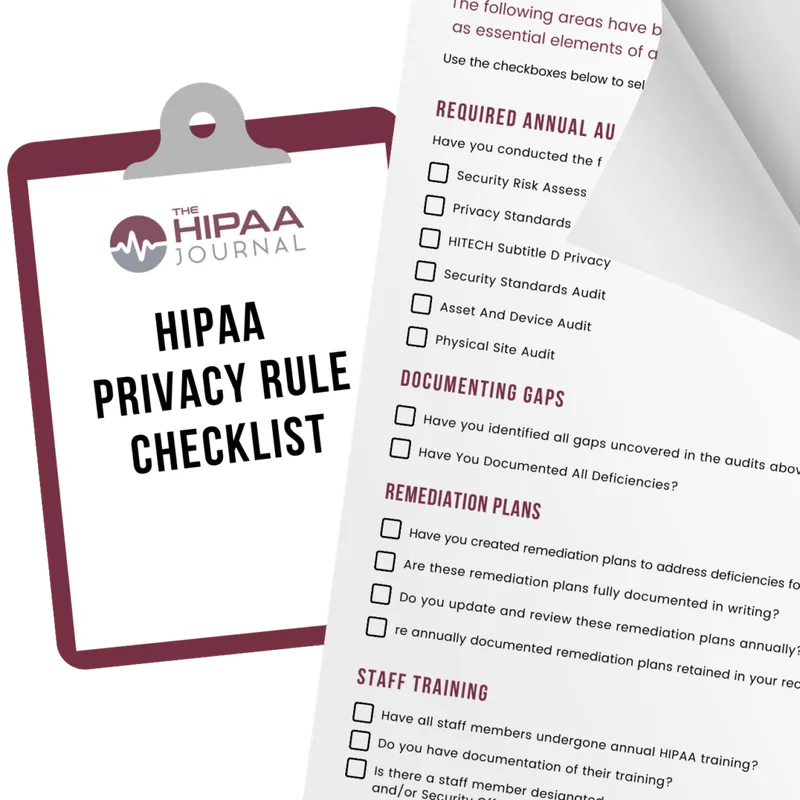
- Under **HIPAA**, the patient has the **right to privacy** regarding their protected health information (PHI). Therefore, the physician must make all reasonable attempts to contact the patient directly to convey their diagnosis.
- Sharing sensitive medical information like a cancer diagnosis with anyone other than the patient, without their explicit consent, would be a **violation of HIPAA regulations**.
*The patient's brother*
- The patient's brother is not automatically authorized to receive her medical information, even if listed as **next of kin**, without the patient's explicit consent or a documented **healthcare power of attorney**.
- Discussing the diagnosis with the brother without the patient's direct consent would be a **breach of patient confidentiality**.
*The patient's husband*
- Even a spouse does not automatically have the right to access a patient's **PHI** without the patient's express permission, according to **HIPAA**.
- While often a trusted contact, without explicit consent, revealing the diagnosis to the husband would still violate the patient's **privacy rights**.
*The patient's daughter*
- Similar to other family members, the patient's daughter is not legally entitled to receive her mother's confidential medical information without explicit authorization or a medical **power of attorney**.
- The physician's primary responsibility is to the patient herself, ensuring her **privacy** is maintained.
*All of the options*
- According to **HIPAA**, sharing the patient's diagnosis with any family member without her explicit consent would be a **breach of confidentiality**.
- This option incorrectly assumes that **next of kin** automatically have the right to receive sensitive medical information.
Principles of medical ethics US Medical PG Question 4: An 83-year-old man presents to the gastroenterologist to follow-up on results from a biopsy of a pancreatic head mass, which the clinician was concerned could be pancreatic cancer. After welcoming the patient and his wife to the clinic, the physician begins to discuss the testing and leads into delivering the results, which showed metastatic pancreatic adenocarcinoma. Before she is able to disclose these findings, the patient stops her and exclaims, "Whatever it is, I don't want to know. Please just make me comfortable in my last months alive. I have made up my mind about this." Which of the following is the most appropriate response on the part of the physician?
- A. "If that is your definite wish, then I must honor it" (Correct Answer)
- B. "The cancer has spread to your liver"
- C. "As a physician, I am obligated to disclose these results to you"
- D. "If you don't know what condition you have, I will be unable to be your physician going forward"
- E. "Please, sir, I strongly urge you to reconsider your decision"
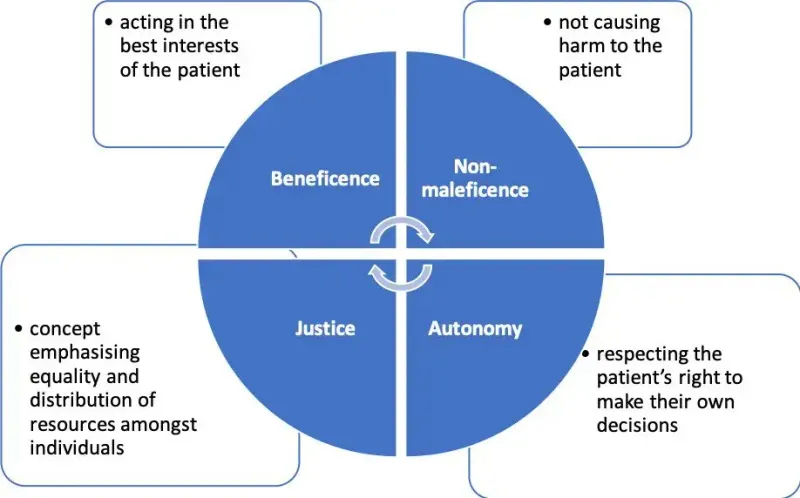
Principles of medical ethics Explanation: ***"If that is your definite wish, then I must honor it"***
- This response respects the patient's **autonomy** and right to refuse information, aligning with ethical principles of patient-centered care.
- The patient has clearly and articulately stated his desire not to know and wishes for **palliative care**, which the physician should respect.
- The patient appears to have **decision-making capacity** based on his clear communication of wishes.
*"The cancer has spread to your liver"*
- This statement violates the patient's explicit request not to be informed of his diagnosis, potentially causing distress and undermining trust.
- Disclosure of information against a patient's wishes is unethical when the patient has **decision-making capacity** and has clearly refused information.
*"As a physician, I am obligated to disclose these results to you"*
- While physicians have a general duty to inform, this is superseded by a **competent patient's right to refuse information**.
- No absolute obligation exists to force information upon a patient who explicitly states a desire not to know, especially when it concerns their own health information.
*"If you don't know what condition you have, I will be unable to be your physician going forward"*
- This response is coercive and threatening, attempting to strong-arm the patient into accepting information he has refused.
- A physician's role includes managing symptoms and providing comfort, even if the patient chooses not to know the full diagnostic details of their condition, particularly in a **palliative care** context.
- This statement could constitute **patient abandonment**, which is unethical.
*"Please, sir, I strongly urge you to reconsider your decision"*
- While it's acceptable to ensure the patient fully understands the implications of their decision, a forceful "urge to reconsider" after a clear refusal can be seen as undermining their **autonomy**.
- The physician should confirm the patient's understanding and offer an opportunity to discuss it later if desired, rather than immediately pressuring them.
Principles of medical ethics US Medical PG Question 5: A 52-year-old man with stage IV melanoma comes to the physician with his wife for a routine follow-up examination. He was recently diagnosed with new bone and brain metastases despite receiving aggressive chemotherapy but has not disclosed this to his wife. He has given verbal consent to discuss his prognosis with his wife and asks the doctor to inform her of his condition because he does not wish to do so himself. She is tearful and has many questions about his condition. Which of the following would be the most appropriate statement by the physician to begin the interview with the patient's wife?
- A. Have you discussed a living will or goals of care together?
- B. We should talk about how we can manage his symptoms with additional chemotherapy.
- C. Why do you think your husband has not discussed his medical condition with you?
- D. What is your understanding of your husband's current condition? (Correct Answer)
- E. Your husband has end-stage cancer, and his prognosis is poor.
Principles of medical ethics Explanation: ***What is your understanding of your husband's current condition?***
- This statement initiates the conversation by **assessing the wife's current knowledge** and emotional state, which is crucial for delivering sensitive and appropriate information.
- It allows the physician to tailor the discussion to her specific understanding and concerns, ensuring that information is delivered compassionately and effectively.
*Have you discussed a living will or goals of care together?*
- This question is too abrupt and **premature** as an opening, as the wife is clearly distressed and unaware of the full severity of her husband's condition.
- Discussions about end-of-life planning should only occur after the patient's wife has a clear understanding of the diagnosis and prognosis, and has processed this information.
*Your husband has end-stage cancer, and his prognosis is poor.*
- While factual, this statement is **too blunt and lacks empathy** for an opening, especially given the wife's emotional state and lack of prior knowledge.
- Delivering such devastating news directly without first assessing her understanding or providing context can be traumatic and impede effective communication.
*We should talk about how we can manage his symptoms with additional chemotherapy.*
- This statement implies a focus on further aggressive treatment which may not be appropriate given the **new bone and brain metastases** and aggressive prior chemotherapy, suggesting a limited benefit of more chemotherapy.
- It also **diverts from the primary need to discuss the overall prognosis** and the patient's rapidly declining condition, which the doctor has been asked to convey.
*Why do you think your husband has not discussed his medical condition with you?*
- This question is **accusatory** and places blame on either the patient or the wife, which is inappropriate and unhelpful in a sensitive medical discussion.
- It shifts the focus away from providing medical information and empathy towards a speculative and potentially confrontational topic.
Principles of medical ethics US Medical PG Question 6: A 32-year-old man visits his primary care physician for a routine health maintenance examination. During the examination, he expresses concerns about not wanting to become a father. He has been sexually active and monogamous with his wife for the past 5 years, and they inconsistently use condoms for contraception. He tells the physician that he would like to undergo vasectomy. His wife is also a patient under the care of the physician and during her last appointment, she expressed concerns over being prescribed any drugs that could affect her fertility because she would like to conceive soon. Which of the following is the most appropriate action by the physician regarding this patient's wish to undergo vasectomy?
- A. Explain the procedure's benefits, alternatives, and potential complications (Correct Answer)
- B. Refer the patient to a psychotherapist to discuss his reluctance to have children
- C. Discourage the patient from undergoing the procedure because his wife wants children
- D. Insist that the patient returns with his wife to discuss the risks and benefits of the procedure together
- E. Call the patient's wife to obtain her consent for the procedure
Principles of medical ethics Explanation: ***Explain the procedure's benefits, alternatives, and potential complications***
- The physician's primary ethical obligation is to the individual patient, ensuring informed consent for any medical procedure. Providing comprehensive information about **vasectomy benefits, alternatives, and risks** allows the patient to make an autonomous decision.
- While patient-physician confidentiality generally prohibits disclosing specific details of one spouse's medical history to the other, the general knowledge that his wife desires children creates an important backdrop for the discussion. It is the patient's responsibility to consider this and convey this information to his wife.
*Refer the patient to a psychotherapist to discuss his reluctance to have children*
- It is **not appropriate** to assume the patient has a psychological issue solely based on his desire for a vasectomy, even with his wife's conflicting wishes. This action could be seen as judgmental and dismissive of the patient's autonomy.
- A patient's preference for sterilization, even if contrary to a partner's desires, does not inherently indicate a need for psychiatric evaluation unless there are other concerning psychological symptoms.
*Discourage the patient from undergoing the procedure because his wife wants children*
- **Discouraging** the patient based on his wife's wishes infringes upon the patient's **autonomy and reproductive rights**. The physician's role is to provide information and support the patient's informed decisions, not to act as a relationship counselor or impose personal values.
- Medical decisions, especially concerning fertility, are deeply personal, and a physician should not pressure a patient into a decision they do not want based on a partner's separate, yet relevant, wishes.
*Insist that the patient returns with his wife to discuss the risks and benefits of the procedure together*
- While open communication between spouses about reproductive decisions is beneficial, **insisting** on the wife's presence for the consultation undermines the patient's **confidentiality and individual autonomy**. The patient has the right to make medical decisions independently.
- The physician should encourage the patient to discuss this with his wife, but it is ultimately the patient's decision whether to involve her in the consultation for his procedure.
*Call the patient's wife to obtain her consent for the procedure*
- This action would be a **breach of patient confidentiality**. The physician cannot disclose information about the patient's decision or medical discussions with a third party, even a spouse, without the patient's explicit consent.
- A spouse's consent is **not legally or ethically required** for an individual to undergo a vasectomy in most jurisdictions, as it is a decision pertaining to the individual's body and reproductive rights.
Principles of medical ethics US Medical PG Question 7: A psychiatrist receives a call from a patient who expresses thoughts of harming his ex-girlfriend. The patient describes a detailed plan to attack her at her workplace. Which of the following represents the psychiatrist's most appropriate legal obligation?
- A. Warn the ex-girlfriend and notify law enforcement (Correct Answer)
- B. Only notify the patient's family
- C. Warn only law enforcement
- D. Maintain patient confidentiality
Principles of medical ethics Explanation: ***Warn the ex-girlfriend and notify law enforcement***
- This scenario directly triggers the **"duty to warn"** and **"duty to protect"** principles, primarily stemming from the **Tarasoff v. Regents of the University of California** case.
- The psychiatrist has a legal obligation to take reasonable steps to protect the identifiable victim, which includes directly warning the intended victim and informing law enforcement.
*Only notify the patient's family*
- Notifying the patient's family alone does not fulfill the **legal obligation to protect** an identifiable third party from a serious threat of harm.
- While family involvement might be part of a comprehensive safety plan, it is insufficient as the sole action in this critical situation.
*Warn only law enforcement*
- While notifying law enforcement is a crucial step, the **Tarasoff duty** specifically mandates warning the **intended victim** directly (or those who can reasonably be expected to notify the victim).
- Relying solely on law enforcement might not ensure the immediate safety of the ex-girlfriend, especially if there's a delay in their response or ability to locate her.
*Maintain patient confidentiality*
- Patient confidentiality is a cornerstone of psychiatric practice, but it is **not absolute** when there is a serious and imminent threat of harm to an identifiable individual.
- The **duty to protect** a potential victim *outweighs* the duty to maintain confidentiality in such extreme circumstances.
Principles of medical ethics US Medical PG Question 8: A 78-year-old woman comes to her family physician for an annual health maintenance examination. Her husband, who worked as an art collector and curator, recently passed away. To express her gratitude for the longstanding medical care of her husband, she offers the physician and his staff a framed painting from her husband's art collection. Which of the following is the most appropriate reaction by the physician?
- A. Politely decline and explain that he cannot accept gifts that belonged to her late husband.
- B. Politely decline and explain that he cannot accept valuable gifts from his patients. (Correct Answer)
- C. Accept the gift to maintain a positive patient-physician relationship but decline any further gifts.
- D. Accept the gift and assure the patient that he will take good care of her.
- E. Accept the gift and donate the painting to a local museum.
Principles of medical ethics Explanation: ***Politely decline and explain that he cannot accept valuable gifts from his patients.***
- Physicians should generally **decline valuable gifts** from patients to avoid the appearance of undue influence, conflicts of interest, or compromising the **professional patient-physician relationship**.
- Accepting valuable gifts can create a sense of obligation, potentially affecting medical judgment or leading to expectations of preferential treatment.
*Politely decline and explain that he cannot accept gifts that belonged to her late husband.*
- While refusing gifts from a deceased patient's estate might seem appropriate for some, the primary ethical concern here is the **value of the gift itself** and its potential impact on the physician-patient dynamic.
- The ownership history of the gift is secondary to the ethical principles guiding gift-giving in medicine.
*Accept the gift to maintain a positive patient-physician relationship but decline any further gifts.*
- Accepting a valuable gift, even with the intention of declining future ones, can still set a problematic precedent and create a **sense of obligation** which may undermine **professional boundaries**.
- A positive patient-physician relationship should be built on trust and excellent care, not on accepting valuable material offerings.
*Accept the gift and assure the patient that he will take good care of her.*
- Accepting a valuable gift and then assuring good care can be perceived as an **exchange of services for a gift**, which is ethically problematic and can lead to a significant **conflict of interest**.
- It blurs the lines between professional medical care and personal favors dependent on material offerings.
*Accept the gift and donate the painting to a local museum.*
- Even if the physician intends to donate the gift, the initial act of **accepting a valuable item** from a patient still carries the ethical risks of creating **perceived obligations** and blurring professional boundaries.
- The patient's intention is to give the gift to the physician, and how the physician then disposes of it does not mitigate the initial ethical concern.
Principles of medical ethics US Medical PG Question 9: A 32-year-old male asks his physician for information regarding a vasectomy. On further questioning, you learn that he and his wife have just had their second child and he asserts that they no longer wish to have additional pregnancies. You ask him if he has discussed a vasectomy with his wife to which he replies, "Well, not yet, but I'm sure she'll agree." What is the next appropriate step prior to scheduling the patient's vasectomy?
- A. Insist that the patient first discuss this procedure with his wife
- B. Telephone the patient's wife to inform her of the plan
- C. Refuse to perform the vasectomy
- D. Explain the risks and benefits of the procedure and request signed consent from the patient and his wife
- E. Explain the risks and benefits of the procedure and request signed consent from the patient (Correct Answer)
Principles of medical ethics Explanation: ***Explain the risks and benefits of the procedure and request signed consent from the patient***
- A patient has the **right to make autonomous decisions** about their own medical care, including reproductive choices, regardless of their marital status or spousal approval.
- The physician's role is to ensure the patient is fully informed and provides **voluntary, uncoerced consent** after understanding the risks, benefits, and alternatives of the procedure.
*Insist that the patient first discuss this procedure with his wife*
- This option would be a **violation of patient autonomy** and confidentiality, as a married person has the right to make independent medical decisions.
- Requiring spousal consent for a procedure performed solely on one individual is not ethically or legally mandated and could be considered discriminatory.
*Telephone the patient's wife to inform her of the plan*
- This action would be a **breach of patient confidentiality**, as the patient's medical information, including his intent to have a vasectomy, cannot be shared with a third party, even a spouse, without explicit permission.
- Informing the wife without the husband's consent also undermines the patient's autonomy and right to privacy regarding his healthcare decisions.
*Refuse to perform the vasectomy*
- Refusing to perform the procedure simply because the patient has not discussed it with his wife would be **unethical and inconsistent with medical professionalism**, assuming the patient is competent and fully informed.
- A physician should not deny medically appropriate care based on a patient's marital dynamics or the presumed wishes of a spouse, as long as the patient's consent is valid.
*Explain the risks and benefits of the procedure and request signed consent from the patient and his wife*
- While it is advisable for a patient to discuss major life decisions with their spouse, requiring **spousal consent for a patient's own medical procedure** is not legally or ethically mandated for competent adults.
- Obtaining consent from both individuals is typically reserved for procedures affecting both parties directly or for those involving a surrogate decision-maker, not for an autonomous adult's personal medical choice.
Principles of medical ethics US Medical PG Question 10: An 86-year-old male is admitted to the hospital under your care for management of pneumonia. His hospital course has been relatively uneventful, and he is progressing well. While making morning rounds on your patients, the patient's cousin approaches you in the hallway and asks about the patient's prognosis and potential future discharge date. The patient does not have an advanced directive on file and does not have a medical power of attorney. Which of the following is the best course of action?
- A. Direct the cousin to the patient's room, telling him that you will be by within the hour to discuss the plan.
- B. Explain that you cannot discuss the patient's care without explicit permission from the patient themselves. (Correct Answer)
- C. Provide the cousin with the patient's most recent progress notes and a draft of his discharge summary.
- D. Explain that the patient is progressing well and should be discharged within the next few days.
- E. Refer the cousin to ask the patient's wife about these topics.
Principles of medical ethics Explanation: ***Explain that you cannot discuss the patient's care without explicit permission from the patient themselves.***
- This is the **correct ethical and legal action** in healthcare to maintain patient confidentiality, as the patient has not designated a medical power of attorney or filed an advance directive.
- The **Health Insurance Portability and Accountability Act (HIPAA)** protects patient health information, requiring explicit patient consent before disclosure to anyone, including family members, unless specific exceptions apply (e.g., immediate threat to safety, treatment purposes directly).
*Direct the cousin to the patient's room, telling him that you will be by within the hour to discuss the plan.*
- While ultimately the patient needs to be involved, directly discussing **private health information** with the cousin without the patient's consent first is a breach of **confidentiality**.
- This approach prematurely assumes the patient will grant permission or wishes for this specific family member to be involved, which might not be true.
*Provide the cousin with the patient's most recent progress notes and a draft of his discharge summary.*
- This action represents a clear and significant **breach of patient confidentiality** and **HIPAA regulations**.
- Without explicit patient consent, sharing detailed medical records with anyone, including family, is strictly prohibited.
*Explain that the patient is progressing well and should be discharged within the next few days.*
- Even a general statement about the patient's condition and discharge plans can be considered a **breach of confidentiality** under HIPAA.
- Such information, while seemingly innocuous, reveals that the individual is indeed a patient and implies details about their health status, which requires patient consent to disclose.
*Refer the cousin to ask the patient's wife about these topics.*
- There is no information provided that the **patient's wife** has legal authority (e.g., **medical power of attorney**) or explicit permission from the patient to discuss his medical information.
- Referring the cousin to the wife without verifying her authority could lead to further breaches of **confidentiality** if the wife is not authorized to share such details.
More Principles of medical ethics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.