Vertebrobasilar system US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Vertebrobasilar system. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Vertebrobasilar system US Medical PG Question 1: A patient undergoes spinal surgery at the L4-L5 level. During the procedure, which of the following ligaments must be divided first to access the spinal canal?
- A. Nuchal ligament
- B. Anterior longitudinal ligament
- C. Supraspinous ligament
- D. Ligamentum flavum (Correct Answer)
Vertebrobasilar system Explanation: ***Ligamentum flavum***
- The **ligamentum flavum** connects the laminae of adjacent vertebrae and forms the posterior boundary of the spinal canal, making it the first ligament encountered anteriorly after removing the lamina.
- While performing a posterior approach **laminectomy**, the ligamentum flavum is typically divided or removed to gain access to the neural structures within the spinal canal.
*Nuchal ligament*
- The **nuchal ligament** is located in the cervical spine and provides attachment for muscles, extending from the external occipital protuberance to the spinous process of C7.
- It is not present at the **L4-L5 level** and therefore plays no role in lumbar spinal surgery.
*Anterior longitudinal ligament*
- The **anterior longitudinal ligament** runs along the anterior surfaces of the vertebral bodies and intervertebral discs.
- It would be encountered during an **anterior surgical approach** to the spine, not a posterior approach to access the spinal canal.
*Supraspinous ligament*
- The **supraspinous ligament** connects the tips of the spinous processes and is the most superficial ligament posteriorly.
- While it is incised during a posterior approach, it is **superficial to the lamina** and ligamentum flavum; therefore, the lamina and ligamentum flavum must be removed or divided first to access the canal.
Vertebrobasilar system US Medical PG Question 2: A 62-year-old woman comes to the physician for decreased vision and worsening headaches since this morning. She has hypertension and hypercholesterolemia. Pulse is 119/min and irregular. Current medications include ramipril and atorvastatin. Ocular and funduscopic examination shows no abnormalities. The findings of visual field testing are shown. Which of the following is the most likely cause of this patient's symptoms?
- A. Occlusion of the posterior cerebral artery (Correct Answer)
- B. Occlusion of anterior cerebral artery
- C. Degeneration of the macula
- D. Occlusion of the anterior inferior cerebellar artery
- E. Impaired perfusion of the retina
Vertebrobasilar system Explanation: ***Occlusion of the posterior cerebral artery***
- The patient presents with **acute visual field defect** and **headache** in the context of an **irregular pulse** (atrial fibrillation).
- **Atrial fibrillation** is a major risk factor for **cardioembolic stroke**, particularly affecting the posterior circulation.
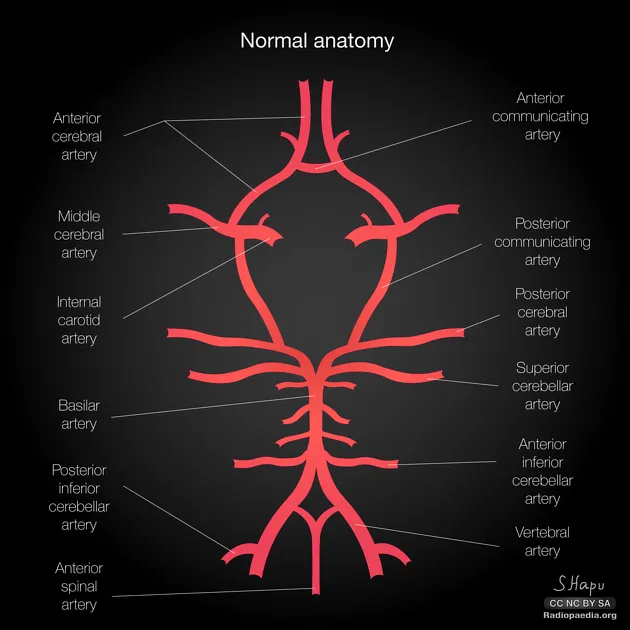
- The **posterior cerebral artery (PCA) supplies the occipital lobe**, which contains the primary visual cortex. PCA occlusion causes **contralateral homonymous hemianopia**, often with **macular sparing** due to collateral blood supply from the middle cerebral artery.
- The visual field defect pattern shown, combined with normal funduscopic examination (ruling out retinal pathology), is characteristic of **occipital cortex ischemia**.
- **Acute onset** with headache further supports an embolic stroke mechanism.
*Occlusion of anterior cerebral artery*
- Anterior cerebral artery (ACA) occlusion primarily affects the **frontal and medial parietal lobes**.
- Classic presentation includes **contralateral leg weakness** > arm weakness, sensory loss in the leg, and behavioral/personality changes.
- ACA strokes do **not cause visual field defects** or homonymous hemianopia.
*Degeneration of the macula*
- Macular degeneration causes **gradual central vision loss**, presenting with difficulty reading and central scotomas.
- This is a **chronic progressive condition**, not acute onset "since this morning."
- Would not cause **headache**, irregular pulse correlation, or the specific visual field pattern shown.
- Funduscopy would typically show **drusen** or retinal pigmentary changes.
*Occlusion of the anterior inferior cerebellar artery*
- AICA occlusion affects the **lateral pons and cerebellum**.
- Presents with **vertigo, nystagmus, ataxia, ipsilateral facial paralysis**, and hearing loss.
- Does **not affect the visual cortex** and would not cause homonymous visual field defects.
*Impaired perfusion of the retina*
- Central retinal artery occlusion causes **sudden monocular painless vision loss** (not bilateral field defects).
- Funduscopy would reveal **"cherry-red spot"** at the macula and retinal whitening.
- The question states funduscopic examination shows **no abnormalities**, excluding this diagnosis.
- Would not explain the bilateral homonymous field defect pattern.
Vertebrobasilar system US Medical PG Question 3: A researcher is studying the brains of patients who recently died from stroke-related causes. One specimen has a large thrombus in an area of the brain that is important in relaying many modalities of sensory information from the periphery to the sensory cortex. Which of the following embryologic structures gave rise to the part of the brain in question?
- A. Metencephalon
- B. Diencephalon (Correct Answer)
- C. Mesencephalon
- D. Telencephalon
- E. Myelencephalon
Vertebrobasilar system Explanation: ***Diencephalon***
- The **thalamus**, a key relay center for sensory information to the cerebral cortex, develops from the diencephalon.
- A thrombus in this area would severely impair the transmission of **sensory modalities** from the periphery.
*Metencephalon*
- The metencephalon gives rise to the **pons** and the **cerebellum**.
- These structures are primarily involved in motor control, coordination, and respiratory regulation, not direct sensory relay to the cortex.
*Mesencephalon*
- The mesencephalon develops into the **midbrain**.
- The midbrain contains structures involved in visual and auditory reflexes, and motor control, but not the primary sensory relay described.
*Myelencephalon*
- The myelencephalon gives rise to the **medulla oblongata**.
- The medulla is crucial for vital autonomic functions (e.g., breathing, heart rate) and connects the brain to the spinal cord.
*Telencephalon*
- The telencephalon develops into the **cerebral hemispheres** (cerebral cortex, basal ganglia, hippocampus).
- While it processes sensory information, it is not the primary relay center from the periphery; that role belongs to the thalamus.
Vertebrobasilar system US Medical PG Question 4: A 28-year-old man is brought to the emergency department by ambulance after developing an altered mental state following blunt trauma to the head. The patient was competing at a local mixed martial arts competition when he was struck in the head and lost consciousness. A few minutes later, upon regaining consciousness, he had a progressive decline in mental status. Past medical history is noncontributory. Upon arrival at the hospital, the temperature is 37.0°C (98.6°F), the blood pressure is 145/89 mm Hg, the pulse is 66/min, the respiratory rate is 14/min, and the oxygen saturation is 99% on room air. He is alert now. A noncontrast CT scan is performed, and the result is provided in the image. Which of the following structures is most likely affected in this patient?
- A. Subarachnoid space
- B. Suprasellar cistern
- C. Middle Meningeal artery (Correct Answer)
- D. Ventricular system
- E. Bridging veins
Vertebrobasilar system Explanation: ***Middle Meningeal artery***
- The CT scan shows a **lenticular** or **biconvex** shaped hemorrhage, characteristic of an **epidural hematoma**. This type of hematoma is typically caused by trauma leading to rupture of the middle meningeal artery.
- The history of blunt head trauma followed by a **lucid interval** and then progressive neurological decline strongly points to an epidural hematoma, which results from arterial bleeding.
*Subarachnoid space*
- Hemorrhage in the subarachnoid space (subarachnoid hemorrhage) typically appears as **blood filling the sulci and basal cisterns** on CT, not a localized collection like seen in the image.
- While subarachnoid hemorrhage can be traumatic, the classic presentation of an epidural hematoma (lucid interval, lenticular shape) is not consistent with primary subarachnoid bleeding.
*Suprasellar cistern*
- The suprasellar cistern is located at the base of the brain, superior to the sella turcica, and typically contains cerebrospinal fluid.
- While it can be affected by subarachnoid hemorrhage, the image clearly shows a hematoma in the temporal-parietal region, not specifically within the suprasellar cistern.
*Ventricular system*
- The ventricular system contains CSF and is an internal structure of the brain. Hemorrhage within the ventricles (intraventricular hemorrhage) would appear as blood filling the ventricular spaces.
- The image shows an extra-axial hematoma, meaning outside the brain parenchyma and ventricles.
*Bridging veins*
- Rupture of bridging veins typically causes a **subdural hematoma**, which appears as a **crescent-shaped** collection of blood along the surface of the brain, conforming to the contours of the cerebral hemisphere.
- The hematoma in the image has a **lenticular (biconvex)** shape, which is characteristic of an epidural hematoma, not a subdural hematoma.
Vertebrobasilar system US Medical PG Question 5: A 78-year-old left-handed woman with hypertension and hyperlipidemia is brought to the emergency room because of sudden-onset right leg weakness and urinary incontinence. Neurologic examination shows decreased sensation over the right thigh. Muscle strength is 2/5 in the right lower extremity and 4/5 in the right upper extremity. Strength and sensation in the face are normal but she has difficulty initiating sentences and she is unable to write her name. The most likely cause of this patient’s condition is an occlusion of which of the following vessels?
- A. Right vertebrobasilar artery
- B. Right middle cerebral artery
- C. Left posterior cerebral artery
- D. Left anterior cerebral artery (Correct Answer)
- E. Right anterior cerebral artery
Vertebrobasilar system Explanation: ***Left anterior cerebral artery***
- Stroke in the **left anterior cerebral artery (ACA)** territory typically causes **contralateral leg weakness** (right leg in this case) and **urinary incontinence** due to involvement of the paracentral lobule.
- The patient's difficulty writing her name (agraphia) and initiating sentences (transcortical motor aphasia, which can manifest as difficulty initiating speech) is consistent with damage to the supplemental motor area in the dominant (left) hemisphere, provided by the ACA.
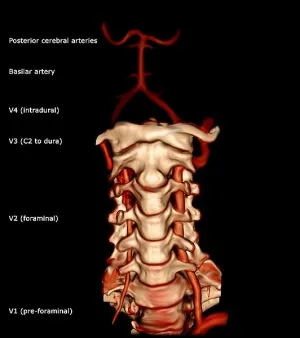
*Right vertebrobasilar artery*
- Occlusion of the vertebrobasilar artery typically presents with a wide range of symptoms including **vertigo**, **ataxia**, **dysarthria**, and bilateral or alternating sensory/motor deficits.
- It would not selectively cause isolated right leg weakness, urinary incontinence, and dominant hemisphere language difficulties without other brainstem or cerebellar signs.
*Right middle cerebral artery*
- A stroke in the **right middle cerebral artery (MCA)** would cause **left-sided deficit**, not right-sided.
- Although it can cause motor and sensory deficits, it typically affects the arm and face more than the leg, and would not cause the specific language deficits of the dominant hemisphere seen here.
*Left posterior cerebral artery*
- Occlusion of the **left posterior cerebral artery (PCA)** typically leads to issues like **contralateral homonymous hemianopia**, visual field defects, and potentially memory impairment or alexia without agraphia if the splenium of the corpus callosum is involved.
- It directly affects posterior brain regions, so it would not cause the anterior cerebral artery specific symptoms such as prominent contralateral leg weakness, urinary incontinence, or the described language difficulties.
*Right anterior cerebral artery*
- Occlusion of the **right anterior cerebral artery (ACA)** would cause **left leg weakness** and **left-sided sensory deficits**, not the right-sided deficits observed in this patient.
- While it could cause urinary incontinence, the combination of right-sided weakness and dominant hemisphere language deficits points against a right ACA occlusion.
Vertebrobasilar system US Medical PG Question 6: A 72-year-old woman is brought in to the emergency department after her husband noticed that she appeared to be choking on her dinner. He performed a Heimlich maneuver but was concerned that she may have aspirated something. The patient reports a lack of pain and temperature on the right half of her face, as well as the same lack of sensation on the left side of her body. She also states that she has been feeling "unsteady" on her feet. On physical exam you note a slight ptosis on the right side. She is sent for an emergent head CT. Where is the most likely location of the neurological lesion?
- A. Pons
- B. Internal capsule
- C. Cervical spinal cord
- D. Medulla (Correct Answer)
- E. Midbrain
Vertebrobasilar system Explanation: ***Medulla***
- This presentation describes **Wallenberg syndrome** (lateral medullary syndrome), characterized by **ipsilateral facial sensory loss**, **contralateral body sensory loss**, and **ataxia** due to involvement of the spinothalamic tracts, trigeminal nucleus, and cerebellar pathways.
- **Dysphagia** (choking) and **Horner's syndrome** (ptosis, miosis, anhidrosis) are also classic signs, specifically the ptosis seen here, pointing to an infarct in the **lateral medulla**.
*Pons*
- Lesions in the pons typically present with varying degrees of **cranial nerve deficits** (e.g., trigeminal, abducens, facial) and **motor or sensory deficits** affecting both sides of the body due to the decussation of tracts.
- The specific combination of **crossed sensory loss** and other symptoms seen here is not characteristic of isolated pontine lesions.
*Internal capsule*
- A lesion in the internal capsule would primarily cause **contralateral motor weakness (hemiparesis)** and **sensory loss** affecting both the face and body on the same side, without the ipsilateral facial involvement.
- It would not explain the **ataxia** or specific cranial nerve signs like ptosis.
*Cervical spinal cord*
- Spinal cord lesions result in **sensory and motor deficits below the level of the lesion**, affecting both sides of the body symmetrically, or ipsilaterally depending on the tract involved.
- They do not cause **facial sensory disturbances**, **dysphagia**, or **ataxia** in the manner described.
*Midbrain*
- Midbrain lesions typically involve the **oculomotor nerve** (CN III), causing eye movement abnormalities, and can result in **contralateral hemiparesis**.
- They do not produce the **crossed sensory deficits** (ipsilateral face, contralateral body) or **ataxia** characteristic of this case.
Vertebrobasilar system US Medical PG Question 7: A 50-year-old man undergoes parathyroidectomy for treatment-resistant hyperparathyroidism. The procedure is complicated by brisk bleeding from the superior thyroid artery near the external branch of the superior laryngeal nerve. To stop the bleeding, the artery is ligated at its origin. Which of the following is most likely the origin of the artery that was injured in this patient?
- A. Thyrocervical trunk
- B. Ascending pharyngeal artery
- C. Internal carotid artery
- D. Subclavian artery
- E. External carotid artery (Correct Answer)
Vertebrobasilar system Explanation: ***External carotid artery***
- The **superior thyroid artery** is the first branch to arise from the **external carotid artery** in the neck.
- Ligation of this artery at its origin is a common surgical maneuver to control bleeding during thyroid or parathyroid surgery.
*Thyrocervical trunk*
- The **thyrocervical trunk** is a branch of the **subclavian artery** and gives rise to the inferior thyroid artery, not the superior thyroid artery.
- Injury to the superior thyroid artery would not necessitate ligation of a vessel originating from the thyrocervical trunk.
*Ascending pharyngeal artery*
- The **ascending pharyngeal artery** is a small artery that branches from the **external carotid artery** but supplies the pharynx, not the thyroid gland.
- It is not typically implicated in bleeding during parathyroidectomy or in relation to the superior laryngeal nerve.
*Internal carotid artery*
- The **internal carotid artery** primarily supplies the brain and does not have branches in the neck that supply the thyroid or parathyroid glands.
- It arises from the common carotid artery but does not give off the superior thyroid artery.
*Subclavian artery*
- The **subclavian artery** gives rise to the **thyrocervical trunk**, which then supplies the inferior thyroid artery, but not directly the superior thyroid artery.
- The superior thyroid artery originates higher up from the external carotid artery.
Vertebrobasilar system US Medical PG Question 8: A 75-year-old man is brought to the emergency room after being found unresponsive in his home. His medical history is unknown. On physical examination he does not demonstrate any spontaneous movement of his extremities and is unable to respond to voice or painful stimuli. You notice that he is able blink and move his eyes in the vertical plane. Based on these physical exam findings, you expect that magnetic resonance angiogram will most likely reveal an occlusion in which of the following vessels?
- A. Basilar artery (Correct Answer)
- B. Anterior cerebral artery
- C. Anterior spinal artery
- D. Posterior cerebral artery
- E. Anterior inferior cerebellar artery
Vertebrobasilar system Explanation: ***Basilar artery***
- The patient's presentation with **quadriplegia**, inability to respond to stimuli, and preserved **vertical eye movements** and blinking is characteristic of **locked-in syndrome**.
- **Locked-in syndrome** is most commonly caused by an **occlusion of the basilar artery**, leading to infarction of the ventral pons while sparing the tegmentum.
*Anterior cerebral artery*
- Occlusion of the **anterior cerebral artery** typically causes **contralateral leg weakness** and sensory loss, and sometimes **abulia** or urinary incontinence.
- It does not explain the widespread motor paralysis affecting all four limbs or the preservation of vertical eye movements in an otherwise unresponsive patient.
*Anterior spinal artery*
- Occlusion of the **anterior spinal artery** causes an **anterior spinal cord syndrome**, characterized by bilateral weakness and loss of pain/temperature sensation below the lesion, with preserved proprioception and vibration sense.
- This presentation does not include the characteristic signs of **brainstem dysfunction** seen in locked-in syndrome.
*Posterior cerebral artery*
- An occlusion in the **posterior cerebral artery** typically leads to **contralateral homonymous hemianopia**, and depending on the branch occluded, can also cause memory deficits or thalamic pain.
- It does not account for the extensive motor paralysis or the pattern of preserved vertical eye movements seen in locked-in syndrome.
*Anterior inferior cerebellar artery*
- Occlusion of the **anterior inferior cerebellar artery (AICA)** typically results in **lateral pontine syndrome**, which includes ipsilateral facial weakness, hearing loss, cerebellar ataxia, and contralateral loss of pain and temperature sensation.
- While it affects the pons, AICA occlusion does not typically cause the complete quadriplegia and preservation of vertical eye movements characteristic of locked-in syndrome.
Vertebrobasilar system US Medical PG Question 9: A 38-year-old woman with moyamoya disease undergoes cerebral angiography showing bilateral progressive stenosis of distal internal carotid arteries with extensive collateral formation. She has had multiple TIAs despite medical management. CT perfusion shows reduced flow in bilateral MCA territories. The neurosurgery team debates between direct bypass (STA-MCA) versus indirect revascularization (EDAS). Evaluate the optimal approach considering Circle of Willis pathophysiology.
- A. Indirect revascularization allows gradual angiogenesis; better for incomplete Circle variants
- B. Combined direct and indirect approaches optimize collateral development regardless of Circle anatomy (Correct Answer)
- C. Circle of Willis anatomy is irrelevant; external to internal carotid bypass is contraindicated in moyamoya
- D. Observation only; intact Circle of Willis through ACoA and PCoA provides adequate collaterals
- E. Direct bypass provides immediate flow; superior for adults with completed Circle
Vertebrobasilar system Explanation: ***Combined direct and indirect approaches optimize collateral development regardless of Circle anatomy***
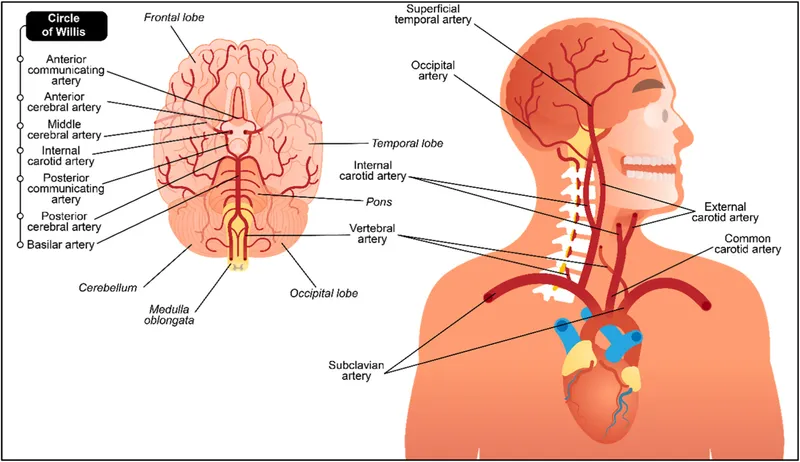
- In **Moyamoya disease**, the **Circle of Willis** loses its compensatory efficiency due to progressive **internal carotid artery (ICA) stenosis**, necessitating both immediate and long-term revascularization strategies.
- A **combined approach** (direct STA-MCA bypass plus indirect EDAS) provides **immediate hemodynamic augmentation** and facilitates **long-term angiogenesis** to counter chronic ischemia.
*Indirect revascularization allows gradual angiogenesis; better for incomplete Circle variants*
- While **indirect revascularization (EDAS)** promotes gradual **angiogenesis**, it is usually less effective in adults when used alone due to reduced angiogenic potential compared to children.
- It does not address the need for **immediate flow restoration** in a patient experiencing recurrent **TIAs** despite medical management.
*Direct bypass provides immediate flow; superior for adults with completed Circle*
- **Direct bypass** (STA-MCA) does provide **immediate flow**, but relying solely on it ignores the benefit of **indirect synangiosis** in providing wider regional coverage over time.
- The status of a "completed" **Circle of Willis** is often irrelevant in advanced disease because the progressive **distal ICA stenosis** prevents effective cross-flow regardless of anatomical completeness.
*Circle of Willis anatomy is irrelevant; external to internal carotid bypass is contraindicated in moyamoya*
- External to internal carotid bypass is not contraindicated; it is actually a **standard of care** for preventing future **ischemic strokes** in symptomatic Moyamoya patients.
- While the disease originates at the **Circle of Willis**, understanding its anatomy is vital for surgical planning and predicting **collateral compensation** patterns.
*Observation only; intact Circle of Willis through ACoA and PCoA provides adequate collaterals*
- Observation is inappropriate for a patient with **recurrent TIAs** and **reduced CT perfusion**, as it carries a high risk of permanent **ischemic stroke**.
- In **Moyamoya disease**, the typical **distal ICA stenosis** frequently involves the origins of the **ACoA and PCoA**, rendering the **Circle of Willis** inadequate for maintaining cerebral perfusion.
Vertebrobasilar system US Medical PG Question 10: A 70-year-old man undergoes elective clipping of an unruptured basilar tip aneurysm. Preoperative angiography shows bilateral fetal-type posterior cerebral arteries (PCAs arising from internal carotid arteries) with hypoplastic P1 segments. The aneurysm involves both posterior communicating artery origins. Synthesize an approach to surgical planning that optimally preserves cerebral perfusion.
- A. Staged bilateral STA-PCA bypasses followed by aneurysm clipping with PCoA sacrifice
- B. Standard clip placement sacrificing one PCoA; contralateral PCoA provides adequate flow
- C. Bypass surgery from external carotid to PCA prior to aneurysm clipping
- D. Endovascular coiling instead of clipping to preserve both PCoA vessels
- E. Clip reconstruction technique preserving both PCoA origins with intraoperative flow assessment (Correct Answer)
Vertebrobasilar system Explanation: ***Clip reconstruction technique preserving both PCoA origins with intraoperative flow assessment***
- In patients with **fetal-type posterior cerebral arteries (PCAs)**, the **posterior communicating artery (PCoA)** is the primary supply to the PCA territory because the **P1 segment** of the basilar artery is hypoplastic.
- **Clip reconstruction** is the gold standard for maintaining the integrity of these vital vessels, and **intraoperative flow assessment** (like ICG angiography) ensures that perfusion to the occipital and temporal lobes is maintained.
*Staged bilateral STA-PCA bypasses followed by aneurysm clipping with PCoA sacrifice*
- While **bypass surgery** can provide additional flow, performing staged bilateral procedures is excessively invasive and carries a high risk for an **unruptured aneurysm**.
- The goal should be the **anatomic preservation** of the primary vessels rather than replacing them with complex extracranial-to-intracranial bypasses unless necessary.
*Standard clip placement sacrificing one PCoA; contralateral PCoA provides adequate flow*
- Sacrificing a **fetal-type PCoA** is contraindicated because the **hypoplastic P1** cannot provide compensatory flow, leading to a major **ischaemic stroke** in the PCA territory.
- Unlike a typical Circle of Willis, **contralateral flow** cannot cross over to support the deprived PCA territory in this specific anatomical configuration.
*Bypass surgery from external carotid to PCA prior to aneurysm clipping*
- External carotid-to-PCA bypass is a complex rescue operation and is typically reserved for cases where **direct clip reconstruction** is technically impossible.
- In elective surgery for a basilar tip aneurysm, the priority is **microsurgical technique** to save the native **internal carotid-driven** flow.
*Endovascular coiling instead of clipping to preserve both PCoA vessels*
- While **endovascular coiling** is an alternative, the question specifically asks for a **surgical planning approach** based on the decision to use clipping.
- Furthermore, coiling a wide-necked **basilar tip aneurysm** often requires stents or balloons that could still inadvertently compromise the **PCoA origins** if not performed meticulously.
More Vertebrobasilar system US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.