Stroke syndromes by vascular territory US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Stroke syndromes by vascular territory. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Stroke syndromes by vascular territory US Medical PG Question 1: A 59-year-old man is brought to the emergency department by his wife for a 1-hour history of sudden behavior changes. They were having lunch together when, at 1:07 PM, he suddenly dropped his sandwich on the floor. Since then, he has been unable to use his right arm. She also reports that he is slurring his speech and dragging his right foot when he walks. Nothing like this has ever happened before. The vital signs include: pulse 95/min, blood pressure 160/90 mm Hg, and respiratory rate 14/min. The physical exam is notable for an irregularly irregular rhythm on cardiac auscultation. On neurological exam, he has a facial droop on the right half of his face but is able to elevate his eyebrows symmetrically. He has 0/5 strength in his right arm, 2/5 strength in his right leg, and reports numbness throughout the right side of his body. Angiography of the brain will most likely show a lesion in which of the following vessels?
- A. Posterior cerebral artery
- B. Internal carotid artery
- C. Middle cerebral artery (Correct Answer)
- D. Basilar artery
- E. Anterior cerebral artery
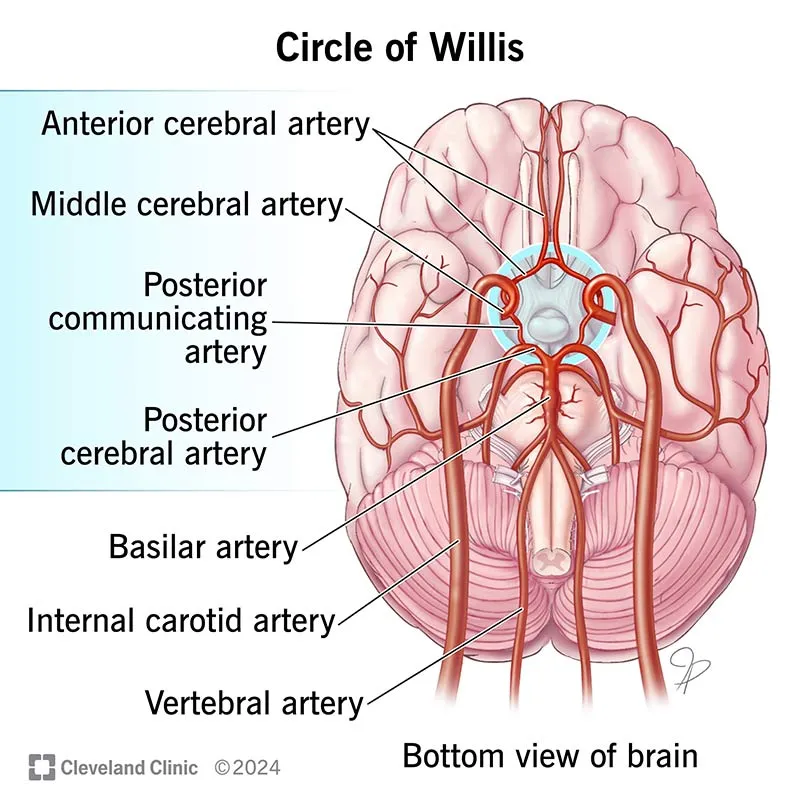
Stroke syndromes by vascular territory Explanation: ***Middle cerebral artery***
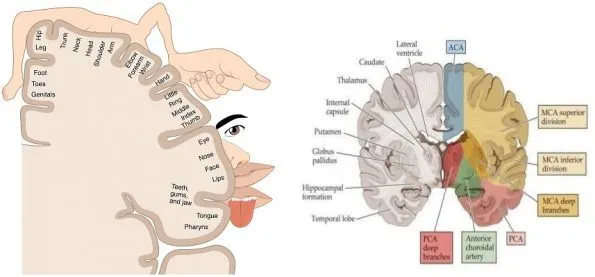
- The patient's symptoms, including **right-sided weakness with arm > leg involvement** (0/5 arm, 2/5 leg), **facial droop** (lower face sparing the forehead), and **slurred speech (dysarthria/aphasia)**, are classic signs of an **MCA stroke**.
- The **arm > leg pattern** is the key distinguishing feature of MCA territory infarction, as the MCA supplies the **lateral motor cortex** (which controls arm and face).
- The finding of an **irregularly irregular rhythm** suggests **atrial fibrillation**, a common cause of **embolic stroke** to the MCA.
*Posterior cerebral artery*
- PCA strokes primarily affect the **occipital lobe** and **medial temporal lobe**, leading to **visual field defects** (e.g., homonymous hemianopsia) or memory deficits.
- While it can cause sensory loss, it typically does not present with the **prominent motor deficits** and **facial droop** seen in this patient.
*Internal carotid artery*
- ICA occlusion can cause symptoms similar to MCA stroke, especially if the **MCA is a direct branch of the ICA**, or it can cause both MCA and ACA symptoms simultaneously.
- However, the specific constellation of symptoms described (predominant motor and sensory deficits, speech issues) points more directly to the **MCA territory downstream**.
*Basilar artery*
- Basilar artery strokes affect the **brainstem** and often present with a combination of **cranial nerve palsies**, **ataxia**, bilateral weakness, **vertigo**, and sometimes **"locked-in" syndrome**.
- The patient's symptoms are more consistent with a **hemispheric lesion**, not a brainstem lesion.
*Anterior cerebral artery*
- ACA strokes typically cause **contralateral leg > arm weakness** (opposite pattern from MCA), as the ACA supplies the **medial motor cortex**.
- ACA strokes may also present with **behavioral changes** (e.g., abulia, apathy) due to involvement of the frontal lobe.
- The patient's prominent **right arm weakness** and **facial droop** are not characteristic of an ACA stroke.
Stroke syndromes by vascular territory US Medical PG Question 2: A 61-year-old man is brought to the emergency room with slurred speech. According to the patient's wife, they were watching a movie together when he developed a minor headache. He soon developed difficulty speaking in complete sentences, at which point she decided to take him to the emergency room. His past medical history is notable for hypertension and hyperlipidemia. He takes aspirin, lisinopril, rosuvastatin. The patient is a retired lawyer. He has a 25-pack-year smoking history and drinks 4-5 beers per day. His father died of a myocardial infarction, and his mother died of breast cancer. His temperature is 98.6°F (37°C), blood pressure is 143/81 mmHg, pulse is 88/min, and respirations are 21/min. On exam, he can understand everything that is being said to him and is able to repeat statements without difficulty. However, when asked to speak freely, he hesitates with every word and takes 30 seconds to finish a short sentence. This patient most likely has an infarct in which of the following vascular distributions?
- A. Proximal middle cerebral artery
- B. Inferior division of the middle cerebral artery
- C. Middle cerebral artery and posterior cerebral artery watershed area
- D. Superior division of the middle cerebral artery (Correct Answer)
- E. Anterior cerebral artery and middle cerebral artery watershed area
Stroke syndromes by vascular territory Explanation: ***Superior division of the middle cerebral artery***
- The patient's inability to speak spontaneously coupled with intact comprehension and repetition is characteristic of **Broca's aphasia**, which results from damage to **Broca's area** in the dominant frontal lobe.
- Broca's area is supplied by the **superior division of the middle cerebral artery (MCA)**.
*Proximal middle cerebral artery*
- An infarct in the proximal MCA, or the main stem, would typically lead to global aphasia if the dominant hemisphere is affected, characterized by **severe deficits in comprehension, repetition, and speech production**.
- This presentation does not align with the patient's ability to understand and repeat statements.
*Inferior division of the middle cerebral artery*
- The inferior division of the MCA supplies Wernicke's area in the dominant hemisphere.
- Damage here causes **Wernicke's aphasia**, characterized by **fluent but nonsensical speech** with **impaired comprehension** and **repetition**, which is contrary to the patient's symptoms.
*Middle cerebral artery and posterior cerebral artery watershed area*
- Watershed infarcts, especially between the MCA and posterior cerebral artery (PCA), can cause **transcortical sensory aphasia** if in the dominant hemisphere.
- This type of aphasia involves impaired comprehension but **intact repetition**, which differs from Broca's aphasia where spontaneous speech is the main deficit.
*Anterior cerebral artery and middle cerebral artery watershed area*
- Infarcts in the watershed area between the anterior cerebral artery (ACA) and MCA can result in **transcortical motor aphasia** if in the dominant hemisphere.
- This condition presents with **non-fluent speech** and **intact repetition**, similar to Broca's aphasia, but Broca's area itself is located specifically within the MCA superior division territory.
Stroke syndromes by vascular territory US Medical PG Question 3: A 72-year-old man with longstanding history of diabetes mellitus and hypertension presents to the emergency department with sudden-onset numbness. On your neurological exam, you note that he has loss of sensation on the left side of his face, arm, and leg. His motor strength exam is normal, as are his cranial nerves. Which of the following is the most likely explanation for his presentation?
- A. Middle cerebral artery stroke
- B. Thalamic stroke (Correct Answer)
- C. Conversion disorder
- D. Anterior cerebral artery stroke
- E. Basilar artery stroke
Stroke syndromes by vascular territory Explanation: ***Thalamic stroke***
- A **thalamic stroke** classically presents with pure sensory deficits, often affecting the **contralateral** side of the body without significant motor weakness or cranial nerve involvement.
- The patient's history of **diabetes mellitus** and **hypertension** are significant risk factors for this type of **lacunar stroke**.
*Middle cerebral artery stroke*
- An **MCA stroke** typically causes **contralateral hemiparesis/hemiplegia** (motor weakness), sensory loss, and possibly **aphasia** (if dominant hemisphere) or **hemineglect** (if non-dominant hemisphere).
- The patient's preserved motor strength and normal cranial nerves make a pure MCA stroke unlikely.
*Conversion disorder*
- **Conversion disorder** involves neurological symptoms that are inconsistent with known neurological conditions, often linked to psychological stress.
- While it can manifest as numbness, the specific pattern of **pure sensory loss** and the patient's strong vascular risk factors suggest a physiological rather than psychological cause.
*Anterior cerebral artery stroke*
- An **ACA stroke** primarily affects the **contralateral leg** more than the arm, often with **urinary incontinence** and **abulia** (lack of initiative).
- The patient's involvement of the face, arm, and leg equally, without leg predominance or behavioral changes, is atypical for an ACA stroke.
*Basilar artery stroke*
- A **basilar artery stroke** typically manifests with a wide range of severe neurological deficits, including **ataxia**, **dysarthria**, **diplopia**, **vertigo**, and often with **quadriparesis** or **locked-in syndrome**.
- The patient's isolated sensory loss without other brainstem signs makes a basilar artery stroke highly improbable.
Stroke syndromes by vascular territory US Medical PG Question 4: A 78-year-old left-handed woman with hypertension and hyperlipidemia is brought to the emergency room because of sudden-onset right leg weakness and urinary incontinence. Neurologic examination shows decreased sensation over the right thigh. Muscle strength is 2/5 in the right lower extremity and 4/5 in the right upper extremity. Strength and sensation in the face are normal but she has difficulty initiating sentences and she is unable to write her name. The most likely cause of this patient’s condition is an occlusion of which of the following vessels?
- A. Right vertebrobasilar artery
- B. Right middle cerebral artery
- C. Left posterior cerebral artery
- D. Left anterior cerebral artery (Correct Answer)
- E. Right anterior cerebral artery
Stroke syndromes by vascular territory Explanation: ***Left anterior cerebral artery***
- Stroke in the **left anterior cerebral artery (ACA)** territory typically causes **contralateral leg weakness** (right leg in this case) and **urinary incontinence** due to involvement of the paracentral lobule.
- The patient's difficulty writing her name (agraphia) and initiating sentences (transcortical motor aphasia, which can manifest as difficulty initiating speech) is consistent with damage to the supplemental motor area in the dominant (left) hemisphere, provided by the ACA.
*Right vertebrobasilar artery*
- Occlusion of the vertebrobasilar artery typically presents with a wide range of symptoms including **vertigo**, **ataxia**, **dysarthria**, and bilateral or alternating sensory/motor deficits.
- It would not selectively cause isolated right leg weakness, urinary incontinence, and dominant hemisphere language difficulties without other brainstem or cerebellar signs.
*Right middle cerebral artery*
- A stroke in the **right middle cerebral artery (MCA)** would cause **left-sided deficit**, not right-sided.
- Although it can cause motor and sensory deficits, it typically affects the arm and face more than the leg, and would not cause the specific language deficits of the dominant hemisphere seen here.
*Left posterior cerebral artery*
- Occlusion of the **left posterior cerebral artery (PCA)** typically leads to issues like **contralateral homonymous hemianopia**, visual field defects, and potentially memory impairment or alexia without agraphia if the splenium of the corpus callosum is involved.
- It directly affects posterior brain regions, so it would not cause the anterior cerebral artery specific symptoms such as prominent contralateral leg weakness, urinary incontinence, or the described language difficulties.
*Right anterior cerebral artery*
- Occlusion of the **right anterior cerebral artery (ACA)** would cause **left leg weakness** and **left-sided sensory deficits**, not the right-sided deficits observed in this patient.
- While it could cause urinary incontinence, the combination of right-sided weakness and dominant hemisphere language deficits points against a right ACA occlusion.
Stroke syndromes by vascular territory US Medical PG Question 5: A 52-year-old man is brought to the emergency department while on vacation with a history of sudden onset vertigo and difficulty walking. He was in normal health since starting his vacation a week ago, but today he is suffering from a loss of balance, mild headache, and has had 5–6 episodes of vomiting over the last few hours. He denies fever, neck pain, head trauma, weakness, and diplopia. Past medical history is significant for hypertension and dyslipidemia. His medications include valsartan and atorvastatin, but he missed several doses since leaving for this trip. Blood pressure is 198/112 mm Hg, the heart rate is 76/min, the respiratory rate is 16/min, and the temperature is 37.0°C (98.6°F). The patient is awake and oriented to time, place, and person. Extraocular movements are within normal limits. Muscle strength is normal in all 4 extremities. An urgent head CT is ordered and shown in the picture. What additional clinical features would be expected in this patient?
- A. Inability to speak fluently
- B. Right-sided visual field loss
- C. Right-sided neglect
- D. Inability to comprehend commands
- E. Inability to perform repetitive alternating movements (Correct Answer)
Stroke syndromes by vascular territory Explanation: ***Inability to perform repetitive alternating movements***
- The CT scan image shows a **hypodense lesion in the right cerebellar hemisphere**, which strongly suggests a **cerebellar infarct**.
- **Dysdiadochokinesia** (inability to perform rapid alternating movements) is a classic sign of cerebellar dysfunction, along with ataxia, vertigo, and nystagmus.
- This aligns perfectly with the patient's presentation of **sudden onset vertigo, difficulty walking, and loss of balance**.
- Other expected cerebellar signs include intention tremor, dysmetria, and scanning speech.
*Inability to speak fluently*
- **Broca's aphasia** (non-fluent speech) results from damage to the **dominant (usually left) frontal lobe**, specifically Broca's area.
- This does not align with the imaging findings of a **right cerebellar lesion**.
- The patient is awake and oriented, which is consistent with preserved language function.
*Right-sided visual field loss*
- **Homonymous hemianopsia** results from lesions in the **contralateral visual pathways** (optic tract, lateral geniculate nucleus, optic radiations, or occipital cortex).
- Right-sided visual field loss would require a **left cerebral hemisphere lesion**, not a right cerebellar lesion.
- The patient has normal extraocular movements and denies diplopia, further excluding visual pathway involvement.
*Right-sided neglect*
- **Hemispatial neglect** is most commonly associated with lesions in the **non-dominant (typically right) parietal lobe**.
- While the lesion is right-sided, cerebellar lesions cause **coordination and balance deficits**, not spatial awareness or attention problems.
*Inability to comprehend commands*
- **Wernicke's aphasia** (impaired comprehension) results from damage to the **dominant (usually left) superior temporal gyrus**.
- This is not consistent with a right cerebellar lesion.
- The patient is awake and oriented to time, place, and person, indicating intact comprehension.
Stroke syndromes by vascular territory US Medical PG Question 6: A 62-year-old man is brought to the emergency department by his wife because she thinks he has had a stroke. He has hypertension and type 2 diabetes mellitus. Current medications include enalapril and metformin. He has smoked 1 pack of cigarettes per day for the past 35 years. His blood pressure is 162/95 mm Hg. A CT scan of the brain shows a lacunar stroke involving the left subthalamic nucleus. The patient most likely presented with which of the following findings on physical examination?
- A. Cogwheel rigidity
- B. Dystonia
- C. Hemispatial agnosia
- D. Vertical gaze palsy
- E. Hemiballismus (Correct Answer)
Stroke syndromes by vascular territory Explanation: ***Hemiballismus***
- A lacunar stroke in the **subthalamic nucleus (STN)** typically causes **hemiballismus**, which is characterized by wild, involuntary, large-amplitude flinging movements on one side of the body.
- The STN is part of the **basal ganglia circuit** and its damage leads to disinhibition of the thalamus, resulting in hyperkinetic movements.
*Cogwheel rigidity*
- This is a feature of **Parkinson's disease**, resulting from damage to the **substantia nigra** affecting dopamine production, not typically a direct result of a lacunar stroke in the subthalamic nucleus.
- It is characterized by a jerky resistance to passive movement in a limb.
*Dystonia*
- Characterized by sustained or repetitive muscle contractions resulting in **twisting and repetitive movements** or abnormal fixed postures.
- While basal ganglia dysfunction can cause dystonia, it's a broader term, and **hemiballismus** is a more specific and classic presentation of STN lesions.
*Hemispatial agnosia*
- Refers to a deficit in attention to one side of space, most commonly associated with lesions in the **non-dominant (right) parietal lobe**.
- This is distinct from the motor symptoms expected from a subthalamic nucleus lesion.
*Vertical gaze palsy*
- Commonly associated with lesions in the **midbrain**, particularly the **dorsal midbrain syndrome (Parinaud syndrome)**.
- This is not a typical presentation of a lacunar stroke specifically involving the subthalamic nucleus.
Stroke syndromes by vascular territory US Medical PG Question 7: A 61-year-old man is brought to the emergency department by his son after collapsing to the ground while at home. His son immediately performed cardiopulmonary resuscitation and later the patient underwent successful defibrillation after being evaluated by the emergency medical technician. The patient has a medical history of hypertension, hyperlipidemia, and type II diabetes mellitus. He has smoked one-half pack of cigarettes for approximately 30 years. The patient was admitted to the cardiac intensive care unit, and after a few days developed acute onset right upper extremity weakness. His temperature is 99°F (37.2°C), blood pressure is 145/91 mmHg, pulse is 102/min and irregularly irregular, and respirations are 16/min. On physical examination, the patient is alert and orientated to person, place, and time. His language is fluent and he is able to name, repeat, and read. His strength is 5/5 throughout except in the right hand, wrist, and arm, which is 2/5. Based on this patient's clinical presentation, the affected neuronal fibers decussate at which level of the central nervous system?
- A. Caudal medulla (Correct Answer)
- B. Pons
- C. Spinal cord
- D. Primary motor cortex
- E. Thalamus
Stroke syndromes by vascular territory Explanation: ***Caudal medulla***
- The patient's **acute right upper extremity weakness** following a cardiac event suggests a **stroke** affecting the left motor pathways.
- The **pyramidal decussation**, where the vast majority of the **corticospinal tracts** cross to the contralateral side, occurs in the **caudal medulla**.
*Pons*
- While the corticospinal tracts pass through the pons, they generally do not decussate at this level.
- Lesions in the pons often present with **ipsilateral cranial nerve** deficits and **contralateral body weakness**.
*Spinal cord*
- Only a small percentage (about 10-15%) of the corticospinal fibers decussate in the spinal cord, and these form the **anterior corticospinal tract**, mainly supplying axial muscles.
- Significant contralateral upper extremity weakness implies a lesion higher up, before the spinal cord.
*Primary motor cortex*
- Lesions in the primary motor cortex would cause contralateral weakness, but the decussation itself occurs in the brainstem, not the cortex.
- The motor cortex is where the motor commands originate, not where they cross over.
*Thalamus*
- The thalamus is a major **sensory relay station** and also plays a role in motor control, but it is not the site of decussation for the corticospinal tracts.
- Thalamic lesions typically cause **sensory deficits** (e.g., contralateral hemianesthesia) and sometimes ataxia or dyskinesias.
Stroke syndromes by vascular territory US Medical PG Question 8: A 10-year-old boy is brought to a family physician by his mother with a history of recurrent headaches. The headaches are moderate-to-severe in intensity, unilateral, mostly affecting the left side, and pulsatile in nature. Past medical history is significant for mild intellectual disability and complex partial seizures that sometimes progress to secondary generalized seizures. He was adopted at the age of 7 days. His birth history and family history are not available. His developmental milestones were slightly delayed. There is no history of fever or head trauma. His vital signs are within normal limits. His height and weight are at the 67th and 54th percentile for his age. Physical examination reveals an area of bluish discoloration on his left eyelid and cheek. The rest of the examination is within normal limits. A computed tomography (CT) scan of his head is shown in the exhibit. Which of the following additional clinical findings is most likely to be present?
- A. Glaucoma (Correct Answer)
- B. Ash leaf spots
- C. Charcot-Bouchard aneurysm
- D. Café-au-lait spots
- E. Iris hamartoma
Stroke syndromes by vascular territory Explanation: ***Glaucoma***
- The clinical presentation, including recurrent headaches, complex partial seizures, developmental delay, and a **bluish discoloration on the left eyelid and cheek (facial port-wine stain)**, along with the CT scan showing **cortical calcifications**, is highly suggestive of **Sturge-Weber syndrome**.
- **Glaucoma** is a common ocular manifestation of Sturge-Weber syndrome, particularly on the ipsilateral side of the facial port-wine stain, due to abnormal episcleral vasculature.
*Ash leaf spots*
- **Ash leaf spots** are hypopigmented macules characteristic of **Tuberous Sclerosis Complex**, which also manifests with seizures and intellectual disability but not typically with a facial port-wine stain or cortical calcifications in this pattern.
- While both Sturge-Weber and Tuberous Sclerosis are **neurocutaneous syndromes**, their specific diagnostic features differ.
*Charcot-Bouchard aneurysm*
- **Charcot-Bouchard aneurysms** are small aneurysms that occur in the brain's small penetrating arteries, typically associated with **chronic hypertension**, and can cause **intracerebral hemorrhage**.
- They are not related to the clinical picture of a facial port-wine stain, seizures, or developmental delay seen in this patient.
*Café-au-lait spots*
- **Café-au-lait spots** are hyperpigmented macules and are a hallmark feature of **Neurofibromatosis Type 1 (NF1)**, which is also associated with seizures and developmental delays.
- However, NF1 does not typically present with the facial port-wine stain or the specific cortical calcifications seen in Sturge-Weber syndrome.
*Iris hamartoma*
- **Iris hamartomas**, also known as **Lisch nodules**, are characteristic ocular findings in **Neurofibromatosis Type 1 (NF1)**.
- While NF1 can involve seizures and developmental delays, it does not present with a facial port-wine stain or the typical brain calcifications of Sturge-Weber syndrome.
Stroke syndromes by vascular territory US Medical PG Question 9: A 32-year-old man visits his family physician for 10 months of persistent left flank pain, weight loss, and fatigue. Also, he has had hematuria a couple of times in the last month. His mother was diagnosed and treated for a pheochromocytoma when she was 36 years old, and his father died at 45 years due to myocardial infarction. His personal medical history is not relevant. He does not smoke and used to be a varsity athlete in high school and university. Physical examination shows temporal wasting, pale mucous membranes and palms, a palpable mass in the left flank, and a varicocele that does not reduce upon recumbency. His family physician sends the patient to the emergency department for an abdominal computed tomography (CT) scan, which shows a complex left renal mass and a hemangioblastoma in T10. A biopsy of the renal mass is ordered by the oncology team, which demonstrates compact cells with prominent nucleoli, eosinophilic cytoplasm within a network of a small and thin-walled vasculature. What is the most likely type of tumor in this patient?
- A. Collecting duct carcinoma
- B. Clear-cell carcinoma (Correct Answer)
- C. Oncocytic carcinoma
- D. Papillary carcinoma
- E. Chromophobe carcinoma
Stroke syndromes by vascular territory Explanation: ***Clear-cell carcinoma***
- This patient's presentation with a **renal mass**, hemangioblastoma, a family history of **pheochromocytoma** (his mother), and an early death of his father (likely from heart disease associated with pheochromocytoma) is highly suggestive of **Von Hippel-Lindau (VHL) syndrome**. **Clear cell renal cell carcinoma** is the most common renal tumor associated with VHL syndrome.
- The biopsy description of **compact cells with prominent nucleoli**, **eosinophilic cytoplasm**, and a **network of small and thin-walled vasculature** is characteristic of clear cell renal cell carcinoma.
*Collecting duct carcinoma*
- This is a rare and aggressive subtype of **renal cell carcinoma** that typically presents with a mass in the renal medulla, often with central necrosis.
- Its histological features involve atypical cells arranged in **tubules or ducts**, which does not match the description of compact cells with eosinophilic cytoplasm.
*Oncocytic carcinoma*
- **Oncocytic carcinoma** is a rare and generally benign tumor. It is characterized histologically by cells with abundant, granular eosinophilic cytoplasm.
- While it has eosinophilic cytoplasm, it lacks the prominent nucleoli and compact cell arrangement seen in the biopsy, and it is not typically associated with VHL syndrome.
*Papillary carcinoma*
- **Papillary carcinoma** is characterized by cells arranged in papillary formations or tubular structures. It is generally associated with different genetic syndromes (e.g., hereditary papillary renal carcinoma).
- The histological description provided, particularly the "compact cells" and vasculature, does not fit the typical papillary architecture.
*Chromophobe carcinoma*
- **Chromophobe carcinoma** is characterized by large cells with distinct cell borders and pale, flocculent cytoplasm. It typically has a good prognosis.
- This type of carcinoma is generally not associated with VHL syndrome and its histological features do not align with the biopsy description of compact cells with eosinophilic cytoplasm and prominent nucleoli.
Stroke syndromes by vascular territory US Medical PG Question 10: A 72-year-old woman is brought to the emergency department for right hip pain 1 hour after she fell while walking around in her house. She has been unable to stand or walk since the fall. She has hypertension and gout. Her sister died of multiple myeloma at the age of 55 years. Current medications include amlodipine and febuxostat. She does not smoke cigarettes. She drinks a glass of wine daily. Her temperature is 37.3°C (99.1°F), pulse is 101/min, and blood pressure is 128/86 mm Hg. Examination shows right groin tenderness. Range of motion of the right hip is limited by pain. The remainder of the examination shows no abnormalities. A complete blood count and serum creatinine concentration are within the reference range. An x-ray of the hip shows a linear fracture of the right femoral neck. She is scheduled for surgery. Which of the following is the most likely underlying cause of this patient's fracture?
- A. Defective osteoclast function
- B. Impaired bone mineralization
- C. Monoclonal antibody production
- D. Interrupted vascular supply
- E. Reduced osteoblastic activity (Correct Answer)
Stroke syndromes by vascular territory Explanation: ***Reduced osteoblastic activity***
- In a 72-year-old woman, a **femoral neck fracture** following a fall typically indicates underlying **osteoporosis**, which is characterized by reduced **osteoblastic activity** and overall bone density loss.
- As women age, particularly after menopause, **estrogen deficiency** leads to an imbalance in bone remodeling, with bone resorption outpacing bone formation, thus leading to weaker bones.
*Defective osteoclast function*
- **Defective osteoclast function** is primarily associated with conditions like **osteopetrosis**, where bones become dense and brittle due to impaired bone resorption, making them prone to fracture, which is not consistent with the typical presentation of a hip fracture in an elderly woman.
- This condition is rare and usually presents earlier in life, often with symptoms such as **anemia**, **hepatosplenomegaly**, and **cranial nerve compression**.
*Impaired bone mineralization*
- **Impaired bone mineralization** is characteristic of **osteomalacia** (in adults) or **rickets** (in children), usually due to **vitamin D deficiency** or phosphate imbalances.
- While it can lead to bone pain and increased fracture risk, osteoporosis due to aging is a much more common cause of hip fractures in this demographic, and there are no signs of osteomalacia such as **pseudofractures** or specific biochemical abnormalities like **hypophosphatemia** or **elevated alkaline phosphatase** without other causes.
*Monoclonal antibody production*
- **Monoclonal antibody production** is associated with **multiple myeloma**, a plasma cell malignancy that causes **lytic bone lesions** and diffuse osteopenia.
- While the patient's sister died of multiple myeloma, her normal complete blood count and creatinine, and the absence of specific myeloma-related symptoms (e.g., **hypercalcemia**, **renal failure**, **anemia**, or **CRAB criteria**) make this diagnosis less likely for her acute hip fracture.
*Interrupted vascular supply*
- **Interrupted vascular supply** can lead to **avascular necrosis (AVN)**, which weakens the bone and can cause collapse, eventually leading to a fracture.
- However, for an acute traumatic hip fracture, especially in the femoral neck, the primary underlying cause in an elderly person is generally **osteoporosis**, and AVN would typically present with chronic pain and characteristic imaging findings prior to an acute traumatic event.
More Stroke syndromes by vascular territory US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.