Communicating arteries US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Communicating arteries. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Communicating arteries US Medical PG Question 1: A 59-year-old man is brought to the emergency department by his wife for a 1-hour history of sudden behavior changes. They were having lunch together when, at 1:07 PM, he suddenly dropped his sandwich on the floor. Since then, he has been unable to use his right arm. She also reports that he is slurring his speech and dragging his right foot when he walks. Nothing like this has ever happened before. The vital signs include: pulse 95/min, blood pressure 160/90 mm Hg, and respiratory rate 14/min. The physical exam is notable for an irregularly irregular rhythm on cardiac auscultation. On neurological exam, he has a facial droop on the right half of his face but is able to elevate his eyebrows symmetrically. He has 0/5 strength in his right arm, 2/5 strength in his right leg, and reports numbness throughout the right side of his body. Angiography of the brain will most likely show a lesion in which of the following vessels?
- A. Posterior cerebral artery
- B. Internal carotid artery
- C. Middle cerebral artery (Correct Answer)
- D. Basilar artery
- E. Anterior cerebral artery
Communicating arteries Explanation: ***Middle cerebral artery***
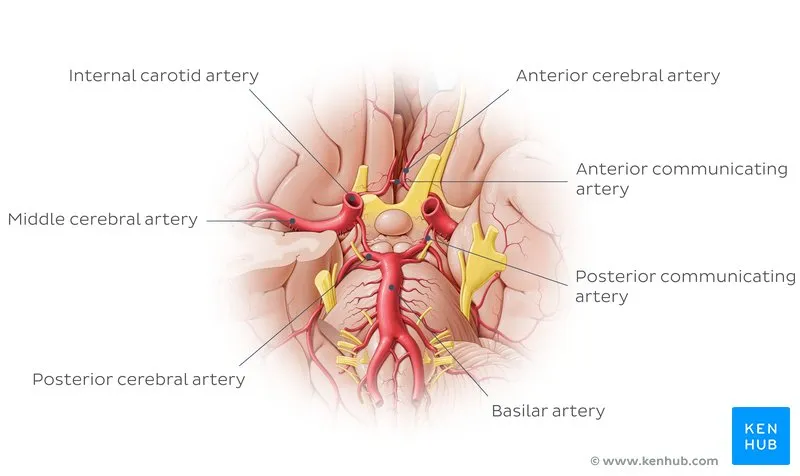
- The patient's symptoms, including **right-sided weakness with arm > leg involvement** (0/5 arm, 2/5 leg), **facial droop** (lower face sparing the forehead), and **slurred speech (dysarthria/aphasia)**, are classic signs of an **MCA stroke**.
- The **arm > leg pattern** is the key distinguishing feature of MCA territory infarction, as the MCA supplies the **lateral motor cortex** (which controls arm and face).
- The finding of an **irregularly irregular rhythm** suggests **atrial fibrillation**, a common cause of **embolic stroke** to the MCA.
*Posterior cerebral artery*
- PCA strokes primarily affect the **occipital lobe** and **medial temporal lobe**, leading to **visual field defects** (e.g., homonymous hemianopsia) or memory deficits.
- While it can cause sensory loss, it typically does not present with the **prominent motor deficits** and **facial droop** seen in this patient.
*Internal carotid artery*
- ICA occlusion can cause symptoms similar to MCA stroke, especially if the **MCA is a direct branch of the ICA**, or it can cause both MCA and ACA symptoms simultaneously.
- However, the specific constellation of symptoms described (predominant motor and sensory deficits, speech issues) points more directly to the **MCA territory downstream**.
*Basilar artery*
- Basilar artery strokes affect the **brainstem** and often present with a combination of **cranial nerve palsies**, **ataxia**, bilateral weakness, **vertigo**, and sometimes **"locked-in" syndrome**.
- The patient's symptoms are more consistent with a **hemispheric lesion**, not a brainstem lesion.
*Anterior cerebral artery*
- ACA strokes typically cause **contralateral leg > arm weakness** (opposite pattern from MCA), as the ACA supplies the **medial motor cortex**.
- ACA strokes may also present with **behavioral changes** (e.g., abulia, apathy) due to involvement of the frontal lobe.
- The patient's prominent **right arm weakness** and **facial droop** are not characteristic of an ACA stroke.
Communicating arteries US Medical PG Question 2: A 76-year-old woman with hypertension and coronary artery disease is brought to the emergency department after the sudden onset of right-sided weakness. Her pulse is 83/min and blood pressure is 156/90 mm Hg. Neurological examination shows right-sided facial drooping and complete paralysis of the right upper and lower extremities. Tongue position is normal and she is able to swallow liquids without difficulty. Knee and ankle deep tendon reflexes are exaggerated on the right. Sensation to vibration, position, and light touch is normal bilaterally. She is oriented to person, place, and time, and is able to speak normally. Occlusion of which of the following vessels is the most likely cause of this patient's current symptoms?
- A. Ipsilateral anterior cerebral artery
- B. Contralateral middle cerebral artery
- C. Anterior spinal artery
- D. Contralateral lenticulostriate artery (Correct Answer)
- E. Ipsilateral posterior inferior cerebellar artery
Communicating arteries Explanation: ***Contralateral lenticulostriate artery***
- The patient presents with **pure motor hemiparesis** affecting the face, arm, and leg equally on the right side, with **no sensory deficits, aphasia, or cognitive impairment**.
- This clinical pattern is classic for a **lacunar stroke** affecting the **internal capsule**, which is supplied by the **lenticulostriate arteries** (branches of the middle cerebral artery).
- The internal capsule contains tightly packed corticospinal and corticobulbar fibers; a small infarct here causes complete contralateral motor deficits without cortical signs.
- The **absence of cortical findings** (normal speech, cognition, and sensation) distinguishes this from cortical MCA stroke.
*Contralateral middle cerebral artery*
- A **cortical MCA stroke** would typically present with **cortical signs** such as aphasia (if left hemisphere), neglect (if right hemisphere), sensory loss, and visual field defects.
- MCA strokes usually show **arm and face > leg** weakness (the leg area is supplied by ACA).
- This patient's **pure motor syndrome** without cortical signs points to a subcortical lesion, not cortical MCA occlusion.
*Ipsilateral anterior cerebral artery*
- First, the lateralization is incorrect - symptoms are right-sided, indicating left hemisphere pathology, so it would be **contralateral** ACA.
- ACA occlusion causes weakness predominantly in the **contralateral leg > arm**, with relative sparing of the face.
- This patient has equal involvement of face, arm, and leg, which is inconsistent with ACA territory.
*Anterior spinal artery*
- The **anterior spinal artery** supplies the anterior two-thirds of the spinal cord, including the corticospinal tracts and anterior horn cells.
- Occlusion causes **bilateral** motor weakness below the lesion level and bilateral loss of pain/temperature sensation.
- It does not cause **unilateral facial weakness** or the distribution of deficits seen in this patient.
*Ipsilateral posterior inferior cerebellar artery*
- Again, lateralization is incorrect - symptoms would be from **contralateral** PICA for motor findings, but PICA supplies the lateral medulla and inferior cerebellum.
- PICA occlusion causes **lateral medullary syndrome (Wallenberg syndrome)**: ataxia, vertigo, dysphagia, dysarthria, Horner syndrome, and contralateral pain/temperature loss.
- The patient's **pure motor hemiparesis** without cerebellar or brainstem signs is incompatible with PICA occlusion.
Communicating arteries US Medical PG Question 3: An 81-year-old woman comes to the emergency department due to a left-sided paralysis for the past 2 hours. Her husband says her symptoms began suddenly, and she is also unable to speak. Her pulse is 90/min, respirations are 18/min, temperature is 36.8°C (98.2°F), and blood pressure is 150/98 mm Hg. An ECG is obtained and is shown below. Which of the following is the most probable cause of the patient's paralysis?
- A. Cocaine toxicity
- B. Rupture of berry aneurysm
- C. Hemorrhagic disorder
- D. Cardioembolic stroke (Correct Answer)
- E. Conversion disorder
Communicating arteries Explanation: ***Cardioembolic stroke***
- The patient presents with **acute neurological deficits** (left-sided paralysis, aphasia) suggesting a **stroke**. The ECG shows **atrial fibrillation** (irregularly irregular rhythm with no clear P waves), which is a significant risk factor for cardioembolic stroke due to thrombus formation in the left atrium.
- The **sudden onset of symptoms** is highly characteristic of an ischemic stroke, and the presence of atrial fibrillation makes a cardioembolic source very likely.
*Cocaine toxicity*
- While cocaine can cause stroke due to vasospasm or accelerated atherosclerosis, it is **less probable in an 81-year-old woman** without other indicators of drug abuse.
- The symptoms of cocaine toxicity usually include **agitation, tachycardia, hypertension, and dilated pupils**, which are not consistently described here.
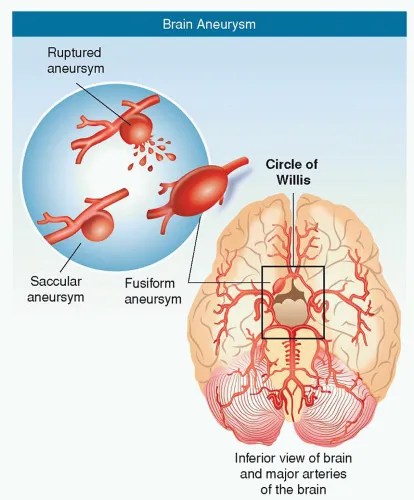
*Rupture of berry aneurysm*
- A ruptured berry aneurysm typically causes a **subarachnoid hemorrhage**, presenting with a **sudden, severe headache** ("thunderclap headache"), meningismus, and often altered consciousness.
- While it can cause focal neurological deficits, the primary presentation is usually different, and the ECG finding of atrial fibrillation does not directly support this diagnosis.
*Hemorrhagic disorder*
- While a hemorrhagic stroke could present with similar neurological deficits, a **primary hemorrhagic disorder** would typically involve a broader history of easy bruising or bleeding, which is not mentioned.
- The ECG finding of **atrial fibrillation** points more strongly towards an embolic rather than hemorrhagic etiology in this context.
*Conversion disorder*
- Conversion disorder is a **functional neurological symptom disorder** where psychological stressors manifest as neurological symptoms without an organic cause.
- The patient's age (81), acute onset of severe, distinct neurological deficits, and especially the **objective finding of atrial fibrillation** on ECG, make a psychological explanation highly unlikely when a clear organic cause is suggested.
Communicating arteries US Medical PG Question 4: A 28-year-old man is brought to the emergency department by ambulance after developing an altered mental state following blunt trauma to the head. The patient was competing at a local mixed martial arts competition when he was struck in the head and lost consciousness. A few minutes later, upon regaining consciousness, he had a progressive decline in mental status. Past medical history is noncontributory. Upon arrival at the hospital, the temperature is 37.0°C (98.6°F), the blood pressure is 145/89 mm Hg, the pulse is 66/min, the respiratory rate is 14/min, and the oxygen saturation is 99% on room air. He is alert now. A noncontrast CT scan is performed, and the result is provided in the image. Which of the following structures is most likely affected in this patient?
- A. Subarachnoid space
- B. Suprasellar cistern
- C. Middle Meningeal artery (Correct Answer)
- D. Ventricular system
- E. Bridging veins
Communicating arteries Explanation: ***Middle Meningeal artery***
- The CT scan shows a **lenticular** or **biconvex** shaped hemorrhage, characteristic of an **epidural hematoma**. This type of hematoma is typically caused by trauma leading to rupture of the middle meningeal artery.
- The history of blunt head trauma followed by a **lucid interval** and then progressive neurological decline strongly points to an epidural hematoma, which results from arterial bleeding.
*Subarachnoid space*
- Hemorrhage in the subarachnoid space (subarachnoid hemorrhage) typically appears as **blood filling the sulci and basal cisterns** on CT, not a localized collection like seen in the image.
- While subarachnoid hemorrhage can be traumatic, the classic presentation of an epidural hematoma (lucid interval, lenticular shape) is not consistent with primary subarachnoid bleeding.
*Suprasellar cistern*
- The suprasellar cistern is located at the base of the brain, superior to the sella turcica, and typically contains cerebrospinal fluid.
- While it can be affected by subarachnoid hemorrhage, the image clearly shows a hematoma in the temporal-parietal region, not specifically within the suprasellar cistern.
*Ventricular system*
- The ventricular system contains CSF and is an internal structure of the brain. Hemorrhage within the ventricles (intraventricular hemorrhage) would appear as blood filling the ventricular spaces.
- The image shows an extra-axial hematoma, meaning outside the brain parenchyma and ventricles.
*Bridging veins*
- Rupture of bridging veins typically causes a **subdural hematoma**, which appears as a **crescent-shaped** collection of blood along the surface of the brain, conforming to the contours of the cerebral hemisphere.
- The hematoma in the image has a **lenticular (biconvex)** shape, which is characteristic of an epidural hematoma, not a subdural hematoma.
Communicating arteries US Medical PG Question 5: A 72-year-old woman presents to the emergency department for vision loss. She was reading a magazine this afternoon when she started having trouble seeing out of her left eye. Her vision in that eye got progressively darker, eventually becoming completely black over the course of a few minutes. It then returned to normal after about 10 minutes; she reports she can see normally now. She had no pain and no other symptoms then or now. Past medical history is notable for hypertension and hyperlipidemia. A high-pitched sound is heard when the diaphragm of the stethoscope is placed on her left neck, but her physical exam is otherwise unremarkable; vision is currently 20/30 bilaterally. The etiology of her symptoms most likely localizes to which of the following anatomic locations?
- A. Left atrium
- B. Subclavian artery
- C. Temporal artery
- D. Carotid artery (Correct Answer)
- E. Vertebral artery
Communicating arteries Explanation: ***Carotid artery***
- The sudden, temporary vision loss (amaurosis fugax) in one eye, described as a "curtain coming down," is a classic symptom of an **embolus originating from the ipsilateral carotid artery**.
- The **bruit** heard in the left neck further points to significant **carotid artery stenosis**, which can be a source of these emboli to the **ophthalmic artery**.
*Left atrium*
- An embolus from the left atrium (e.g., in atrial fibrillation) would typically cause symptoms of a **cerebral stroke** or vision loss in **both eyes** if it affects a major supplying vessel before the intracranial branches, or could affect the carotid artery system, but the neck bruit directly implicates the carotid.
- While a source of emboli, the direct finding of a neck bruit makes the carotid the more immediate and specific localization.
*Subclavian artery*
- **Subclavian artery** stenosis can cause **subclavian steal syndrome**, leading to vertebrobasilar insufficiency and symptoms like **dizziness** or **syncope**, but generally does not cause unilateral amaurosis fugax.
- Its territory primarily supplies the arm and posterior circulation, not the anterior cerebral circulation or ophthalmic artery directly as suggested by amaurosis fugax.
*Temporal artery*
- **Temporal arteritis** (Giant Cell Arteritis) can cause sudden vision loss, often irreversible, and is usually associated with **headaches**, **jaw claudication**, and a very high **ESR**, none of which are reported here.
- While it affects the ophthalmic artery, the absence of pain and the transient nature of the vision loss (amaurosis fugax) make it less likely than an embolic event.
*Vertebral artery*
- The **vertebral arteries** supply the **posterior circulation** of the brain, leading to symptoms such as **diplopia**, **vertigo**, **ataxia**, or **hemiparesis**, but not isolated unilateral amaurosis fugax.
- Problems in this artery typically manifest as **vertebrobasilar insufficiency**, which affects both eyes or causes other brainstem symptoms, not transient unilateral blindness.
Communicating arteries US Medical PG Question 6: A 75-year-old man is brought to the emergency room after being found unresponsive in his home. His medical history is unknown. On physical examination he does not demonstrate any spontaneous movement of his extremities and is unable to respond to voice or painful stimuli. You notice that he is able blink and move his eyes in the vertical plane. Based on these physical exam findings, you expect that magnetic resonance angiogram will most likely reveal an occlusion in which of the following vessels?
- A. Basilar artery (Correct Answer)
- B. Anterior cerebral artery
- C. Anterior spinal artery
- D. Posterior cerebral artery
- E. Anterior inferior cerebellar artery
Communicating arteries Explanation: ***Basilar artery***
- The patient's presentation with **quadriplegia**, inability to respond to stimuli, and preserved **vertical eye movements** and blinking is characteristic of **locked-in syndrome**.
- **Locked-in syndrome** is most commonly caused by an **occlusion of the basilar artery**, leading to infarction of the ventral pons while sparing the tegmentum.
*Anterior cerebral artery*
- Occlusion of the **anterior cerebral artery** typically causes **contralateral leg weakness** and sensory loss, and sometimes **abulia** or urinary incontinence.
- It does not explain the widespread motor paralysis affecting all four limbs or the preservation of vertical eye movements in an otherwise unresponsive patient.
*Anterior spinal artery*
- Occlusion of the **anterior spinal artery** causes an **anterior spinal cord syndrome**, characterized by bilateral weakness and loss of pain/temperature sensation below the lesion, with preserved proprioception and vibration sense.
- This presentation does not include the characteristic signs of **brainstem dysfunction** seen in locked-in syndrome.
*Posterior cerebral artery*
- An occlusion in the **posterior cerebral artery** typically leads to **contralateral homonymous hemianopia**, and depending on the branch occluded, can also cause memory deficits or thalamic pain.
- It does not account for the extensive motor paralysis or the pattern of preserved vertical eye movements seen in locked-in syndrome.
*Anterior inferior cerebellar artery*
- Occlusion of the **anterior inferior cerebellar artery (AICA)** typically results in **lateral pontine syndrome**, which includes ipsilateral facial weakness, hearing loss, cerebellar ataxia, and contralateral loss of pain and temperature sensation.
- While it affects the pons, AICA occlusion does not typically cause the complete quadriplegia and preservation of vertical eye movements characteristic of locked-in syndrome.
Communicating arteries US Medical PG Question 7: A 45-year-old woman presents with headaches. She says the headaches started about a month ago, and although initially, they were intermittent, over the past 2 weeks, they have progressively worsened. She describes the pain as severe, worse on the left than the right, and relieved somewhat by non-steroidal anti-inflammatory drugs (NSAIDs). The headaches are usually associated with nausea, vomiting, and photophobia. She denies any changes in vision, seizures, similar past symptoms, or focal neurologic deficits. Past medical history is significant for a posterior communicating artery aneurysm, status post-clipping 10 years ago. Her vital signs include: blood pressure 135/90 mm Hg, temperature 36.7°C (98.0°F), pulse 80/min, and respiratory rate 14/min. Her body mass index (BMI) is 36 kg/m2. On physical examination, the patient is alert and oriented. Her pupils are 3 mm on the right and mid-dilated on the left with subtle left-sided ptosis. Ophthalmic examination reveals a cup-to-disc ratio of 0.4 on the right and 0.5 on the left. The remainder of her cranial nerves are intact. She has 5/5 strength and 2+ reflexes in her upper extremities bilaterally and her left leg; her right leg has 3/5 strength with 1+ reflexes at the knee and ankle. The remainder of the physical examination is unremarkable. Which of the following findings in this patient most strongly suggests a further diagnostic workup?
- A. Photophobia
- B. Age of onset
- C. Obesity
- D. Left eye findings (Correct Answer)
- E. Right-sided weakness
Communicating arteries Explanation: ***Left eye findings***
- The combination of **left-sided mid-dilated pupil** and **subtle left-sided ptosis** points towards a **left oculomotor nerve (CN III) palsy**. This, in a patient with a history of a **posterior communicating artery aneurysm**, is a critical red flag for aneurysm re-rupture or expansion.
- CN III palsy can cause progressive headaches and is a neurological emergency requiring urgent imaging to rule out pathologies like aneurysm expansion or hemorrhage.
*Photophobia*
- **Photophobia** is a common symptom associated with many types of headaches, including migraines, and by itself, does not strongly suggest a specific serious underlying pathology requiring immediate further workup.
- While it contributes to the headache symptom complex, it lacks the specificity of the observed objective neurological signs.
*Age of onset*
- While the onset of new, severe headaches in a middle-aged adult warrants evaluation, the patient's age (45) for new-onset headaches is not as alarming as the objective neurological deficits present.
- Headaches can develop at any age, and other features in this presentation are more indicative of an acute problem.
*Obesity*
- **Obesity** (BMI 36 kg/m2) is a risk factor for several conditions, including **idiopathic intracranial hypertension (pseudotumor cerebri)**, which can cause headaches.
- However, obesity itself does not directly explain the acute and progressive nature of these headaches or the specific left eye findings.
*Right-sided weakness*
- The **right-sided weakness** (3/5 strength in the right leg with 1+ reflexes) is a lateralizing sign suggesting a central neurological lesion, likely in the contralateral brain.
- While this finding is significant and requires investigation, the **left eye findings** (ptosis and dilated pupil) are more acutely concerning given the patient's history of a posterior communicating artery aneurysm, which directly impacts the third cranial nerve.
Communicating arteries US Medical PG Question 8: An 80-year-old woman is brought to the emergency department for left hip pain 30 minutes after she fell while walking around in her room. Examination shows left groin tenderness. The range of motion of the left hip is limited because of pain. An x-ray of the hip shows a linear fracture of the left femoral neck with slight posterior displacement of the femur. Which of the following arteries was most likely damaged in the patient's fall?
- A. Superior gluteal artery
- B. Deep circumflex iliac
- C. Deep femoral artery
- D. Obturator
- E. Medial circumflex femoral (Correct Answer)
Communicating arteries Explanation: ***Medial circumflex femoral***
- This artery is the **primary blood supply** to the femoral head and neck, making it highly vulnerable to injury in cases of femoral neck fractures.
- Damage to the medial circumflex femoral artery significantly increases the risk of **avascular necrosis** of the femoral head.
*Superior gluteal artery*
- The superior gluteal artery primarily supplies the **gluteus medius** and **minimus muscles**.
- It is **not directly involved** in the primary blood supply to the femoral head and neck.
*Deep circumflex iliac*
- This artery mainly supplies the **iliac fossa** and the **abdominal wall muscles**.
- It does not contribute significantly to the blood supply of the femoral neck.
*Deep femoral artery*
- The deep femoral artery, also known as the **profunda femoris artery**, is the main supply to the **thigh muscles**.
- While it gives rise to the circumflex arteries, it is not the artery directly compromised in a femoral neck fracture.
*Obturator*
- The obturator artery primarily supplies the **adductor muscles** of the thigh and contributes a small branch to the femoral head via the **ligamentum teres**.
- This contribution is **insufficient** to maintain viability of the femoral head, especially in trauma to the femoral neck.
Communicating arteries US Medical PG Question 9: A 68-year-old man comes to the physician because of double vision and unilateral right eye pain that began this morning. His vision improves when he covers either eye. He has hypertension, mild cognitive impairment, and type 2 diabetes mellitus. The patient has smoked two packs of cigarettes daily for 40 years. His current medications include lisinopril, donepezil, metformin, and insulin with meals. His temperature is 37°C (98.6°F), pulse is 85/minute, respirations are 12/minute, and blood pressure is 132/75 mm Hg. His right eye is abducted and depressed with slight intorsion. He can only minimally adduct the right eye. Visual acuity is 20/20 in both eyes. Extraocular movements of the left eye are normal. An MRI of the head shows no abnormalities. His fingerstick blood glucose concentration is 325 mg/dL. Further evaluation is most likely to show which of the following?
- A. Ptosis (Correct Answer)
- B. Dilated and fixed pupil
- C. Bitemporal hemianopsia
- D. Miosis and anhidrosis
- E. Positive swinging-flashlight test
Communicating arteries Explanation: ***Ptosis***
- The patient's presentation of an **abducted and depressed right eye with minimal adduction** is highly suggestive of an **ischemic (diabetic) third nerve palsy**.
- Ischemic third nerve palsies characteristically **spare the pupillary fibers** (pupil remains normal in size and reactive) but affect the **somatomotor fibers** that innervate the extraocular muscles and the **levator palpebrae superioris**, leading to **ptosis**.
- The key clinical feature distinguishing ischemic from compressive CN III palsy is **pupil-sparing**, which is present in this case.
*Dilated and fixed pupil*
- A dilated and fixed pupil would indicate **compression of the oculomotor nerve**, often by an aneurysm (e.g., posterior communicating artery aneurysm).
- Compressive lesions affect the superficial **pupillomotor fibers** first, while ischemic third nerve palsies, as seen in patients with **diabetes**, typically affect the inner somatomotor fibers while **sparing the pupil**.
*Bitemporal hemianopsia*
- This visual field defect is characteristic of **optic chiasm compression**, commonly caused by a **pituitary adenoma**.
- This patient's symptoms are localized to a single eye and involve extraocular muscle dysfunction, not visual field loss.
*Miosis and anhidrosis*
- **Miosis** (constricted pupil) and **anhidrosis** (decreased sweating) on one side of the face, accompanied by **ptosis**, are classic signs of **Horner syndrome**.
- Horner syndrome results from a lesion in the **sympathetic pathway**, which is inconsistent with the extraocular muscle deficits observed in this patient.
*Positive swinging-flashlight test*
- A positive swinging-flashlight test (Marcus Gunn pupil) indicates an **afferent pupillary defect**, often seen in conditions affecting the **optic nerve** (e.g., optic neuritis, severe retinal disease).
- This patient's symptoms point to a **cranial nerve III palsy**, which affects efferent ocular movements and typically does not cause an afferent pupillary defect.
Communicating arteries US Medical PG Question 10: A 26-year-old man is brought to the emergency department by ambulance after being involved in a motor vehicle collision. He does not open his eyes on command or respond to verbal cues. A CT scan of the head shows a hyperdense fluid collection in the right medial temporal lobe with medial displacement of the uncus and parahippocampal gyrus of the temporal lobe. Which of the following cranial nerves is most likely to be injured as a result of this patient's lesion?
- A. Vagus
- B. Facial
- C. Oculomotor (Correct Answer)
- D. Abducens
- E. Trigeminal
Communicating arteries Explanation: ***Oculomotor***
- The description of **medial displacement of the uncus and parahippocampal gyrus** (uncus herniation) compresses the **oculomotor nerve (CN III)** as it passes between the posterior cerebral and superior cerebellar arteries.
- Compression of the oculomotor nerve leads to a **dilated pupil** (due to parasympathetic fiber involvement) and **down-and-out deviation of the eye** (due to paralysis of extraocular muscles it innervates).
*Vagus*
- The vagus nerve (CN X) is deep within the skull and brainstem, far from the temporal lobe, and is not directly affected by uncal herniation.
- Injury to the vagus nerve typically presents with dysphagia, hoarseness, or cardiac arrhythmias, symptoms not indicated here.
*Facial*
- The facial nerve (CN VII) exits the brainstem at the pontomedullary junction and is located more superiorly and laterally than the structures involved in uncal herniation.
- Damage to the facial nerve causes facial muscle weakness or paralysis, which is not the primary concern with uncal herniation.
*Abducens*
- The abducens nerve (CN VI) is a long, slender nerve that can be affected by **generalized increases in intracranial pressure**, but is less commonly directly compressed by an uncal herniation itself.
- Injury to the abducens nerve causes **lateral rectus muscle paralysis**, leading to medial deviation of the eye, whereas uncal herniation typically affects the oculomotor nerve.
*Trigeminal*
- The trigeminal nerve (CN V) exits the pons and is located superior to the tentorial notch and medial temporal lobe, making it unlikely to be directly compressed by uncal herniation.
- Injury to the trigeminal nerve causes sensory loss in the face or weakness of the muscles of mastication, which are not consistent with the described lesion.
More Communicating arteries US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.