Anterior cerebral artery territory US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Anterior cerebral artery territory. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Anterior cerebral artery territory US Medical PG Question 1: A 65-year-old male presents to the emergency room complaining of a severe headache. He developed a sudden-onset severe throbbing headache while watching a football game on television. His past medical history is significant for migraines and hypertension; however, he states that this headache is different from his normal migraine headaches. He has a 30 pack-year smoking history. His family history is notable for stroke in his mother and father. His temperature is 98.9°F (37.2°C), blood pressure is 150/90 mmHg, pulse is 100/min, and respirations are 14/min. On examination, he is oriented to person, place, and time. Neck motion is limited due to pain. Strength is 5/5 bilaterally in both the upper and the lower extremities and sensation is grossly intact across all the dermatomal distributions. Patellar, brachioradialis, and Achilles reflexes are 2+ bilaterally. The vessel that is most commonly involved in this patient's likely condition directly branches off which of the following vessels?
- A. Middle cerebral artery
- B. Maxillary artery
- C. Anterior cerebral artery
- D. Posterior cerebral artery
- E. Internal carotid artery (Correct Answer)
Anterior cerebral artery territory Explanation: ***Internal carotid artery***
- The patient's presentation with a **sudden-onset, severe "thunderclap" headache**, cervical pain, and normal neurologic examination, particularly in the context of **hypertension and smoking history**, is highly suggestive of a **subarachnoid hemorrhage (SAH)**. SAH is most commonly caused by rupture of a **saccular (berry) aneurysm**.
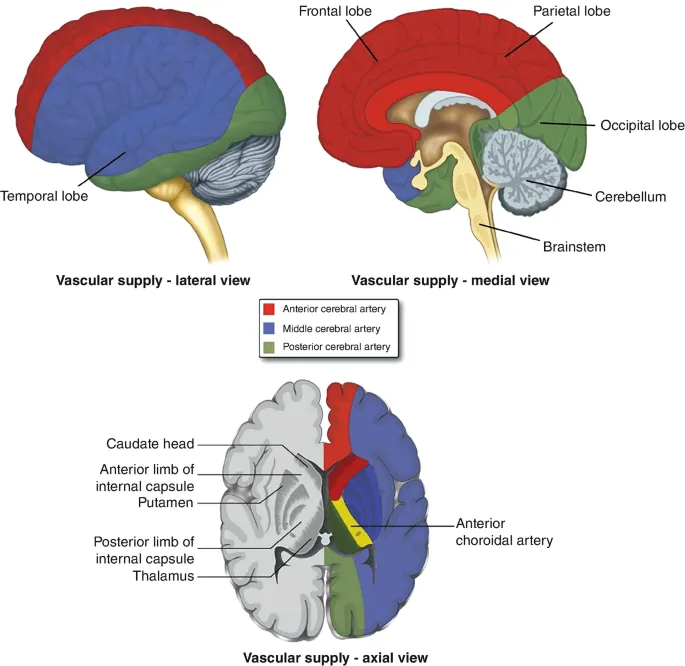
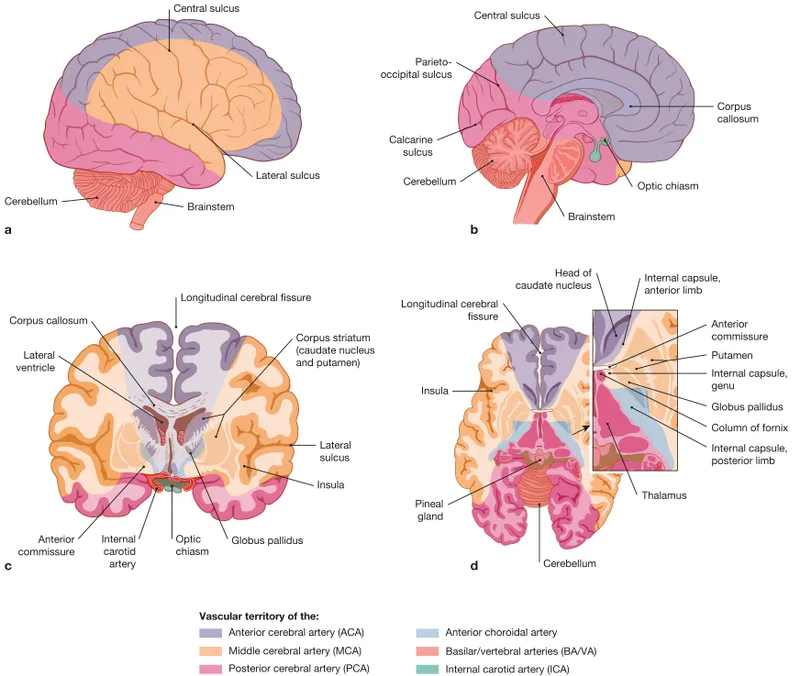
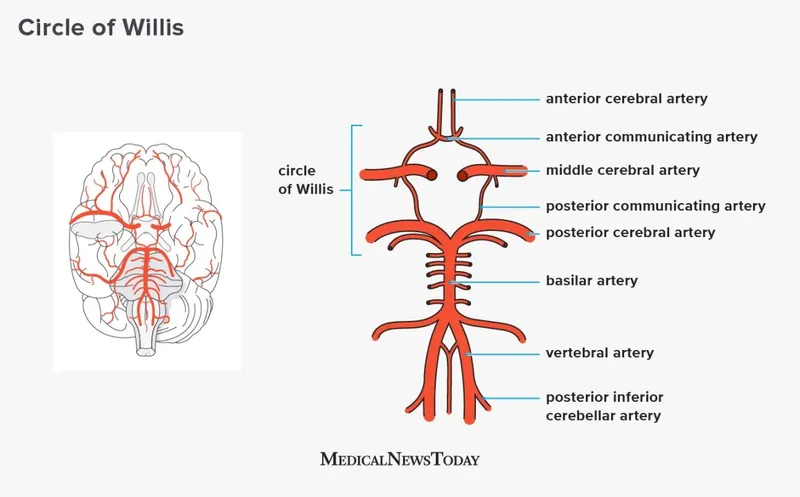
- Approximately 85% of SAHs result from the rupture of an aneurysm in the **anterior circulation**. The most common site for these aneurysms is the **anterior communicating artery**, which directly branches off the **anterior cerebral artery**. However, the **anterior cerebral artery (ACA)**, the **middle cerebral artery (MCA)**, and the **posterior communicating artery (PCoA)** (which is commonly involved in berry aneurysms) all originate directly or indirectly, through the ACA, from the **internal carotid artery (ICA)**. Therefore, the ICA is the most encompassing and correct option from which the most common aneurysm sites ultimately branch.
*Middle cerebral artery*
- While the **middle cerebral artery (MCA)** is a common location for aneurysms, particularly at its bifurcation, it is generally less common than the anterior communicating artery or the posterior communicating artery.
- Aneurysms of the MCA are also branches of the internal carotid artery.
*Maxillary artery*
- The **maxillary artery** is primarily involved in supplying blood to structures in the deep face, maxilla, and mandible.
- It is not a significant location for intracranial berry aneurysms that lead to subarachnoid hemorrhage.
*Anterior cerebral artery*
- While the **anterior cerebral artery (ACA)** itself can be a site for aneurysms, particularly the **anterior communicating artery** (AComA) which connects the two ACAs, it is a branch off the internal carotid artery.
- The AComA is the single most common site for berry aneurysms; however, the question asks for the vessel from which the commonly involved vessel *directly branches off*. The ACA itself directly branches off the ICA.
*Posterior cerebral artery*
- The **posterior cerebral artery (PCA)** is part of the posterior circulation, originating from the basilar artery.
- Aneurysms in the posterior circulation (vertebrobasilar system) are less common causes of SAH than those in the anterior circulation.
Anterior cerebral artery territory US Medical PG Question 2: A 72-year-old man with longstanding history of diabetes mellitus and hypertension presents to the emergency department with sudden-onset numbness. On your neurological exam, you note that he has loss of sensation on the left side of his face, arm, and leg. His motor strength exam is normal, as are his cranial nerves. Which of the following is the most likely explanation for his presentation?
- A. Middle cerebral artery stroke
- B. Thalamic stroke (Correct Answer)
- C. Conversion disorder
- D. Anterior cerebral artery stroke
- E. Basilar artery stroke
Anterior cerebral artery territory Explanation: ***Thalamic stroke***
- A **thalamic stroke** classically presents with pure sensory deficits, often affecting the **contralateral** side of the body without significant motor weakness or cranial nerve involvement.
- The patient's history of **diabetes mellitus** and **hypertension** are significant risk factors for this type of **lacunar stroke**.
*Middle cerebral artery stroke*
- An **MCA stroke** typically causes **contralateral hemiparesis/hemiplegia** (motor weakness), sensory loss, and possibly **aphasia** (if dominant hemisphere) or **hemineglect** (if non-dominant hemisphere).
- The patient's preserved motor strength and normal cranial nerves make a pure MCA stroke unlikely.
*Conversion disorder*
- **Conversion disorder** involves neurological symptoms that are inconsistent with known neurological conditions, often linked to psychological stress.
- While it can manifest as numbness, the specific pattern of **pure sensory loss** and the patient's strong vascular risk factors suggest a physiological rather than psychological cause.
*Anterior cerebral artery stroke*
- An **ACA stroke** primarily affects the **contralateral leg** more than the arm, often with **urinary incontinence** and **abulia** (lack of initiative).
- The patient's involvement of the face, arm, and leg equally, without leg predominance or behavioral changes, is atypical for an ACA stroke.
*Basilar artery stroke*
- A **basilar artery stroke** typically manifests with a wide range of severe neurological deficits, including **ataxia**, **dysarthria**, **diplopia**, **vertigo**, and often with **quadriparesis** or **locked-in syndrome**.
- The patient's isolated sensory loss without other brainstem signs makes a basilar artery stroke highly improbable.
Anterior cerebral artery territory US Medical PG Question 3: A 35-year-old man who suffered a motor vehicle accident 3 months ago presents to the office for a neurological evaluation. He has no significant past medical history and takes no current medications. He has a family history of coronary artery disease in his father and Alzheimer’s disease in his mother. On physical examination, his blood pressure is 110/60 mm Hg, the pulse is 85/min, the temperature is 37.0°C (98.6°F), and the respiratory rate is 20/min. Neurological examination is suggestive of a lesion in the anterior spinal artery that affects the anterior two-thirds of the spinal cord, which is later confirmed with angiography. Which of the following exam findings would have suggested this diagnosis?
- A. Loss of vibratory sense below the level of the lesion
- B. Loss of pain and temperature sensation above the level of the lesion
- C. Negative plantar extensor response in his lower limbs
- D. Flaccid paralysis on the right side
- E. Preserved pressure sensation (Correct Answer)
Anterior cerebral artery territory Explanation: ***Preserved pressure sensation***
- **Anterior spinal artery** occlusion affects the **spinothalamic tracts** (pain and temperature) and **corticospinal tracts** (motor function), but spares the **dorsal columns**.
- The **dorsal columns** carry **vibration, proprioception, and discriminative (fine) touch and pressure sensation**, which would therefore be preserved.
- While crude touch/pressure via the anterior spinothalamic tract may be impaired, the preservation of dorsal column function allows for intact discriminative pressure sensation, distinguishing this from other cord syndromes.
*Loss of vibratory sense below the level of the lesion*
- **Vibratory sense** is carried by the **dorsal columns**, which are typically spared in **anterior spinal artery syndromes** as they are supplied by the posterior spinal arteries.
- Loss of vibratory sense would suggest involvement of the posterior part of the spinal cord, inconsistent with an anterior spinal artery lesion.
*Loss of pain and temperature sensation above the level of the lesion*
- **Anterior spinal artery syndrome** causes loss of **pain and temperature sensation** *below* the level of the lesion, as the spinothalamic tracts are affected in the anterior cord.
- Sensation *above* the lesion level should be intact, as those pathways have already ascended past the lesion.
*Negative plantar extensor response in his lower limbs*
- A **negative plantar extensor response** (normal plantar reflex) indicates the toes curl downwards, which is the normal response.
- Lesions of the **corticospinal tract**, such as in anterior spinal artery syndrome, typically cause a **positive Babinski sign** (extensor plantar response), where the big toe extends upwards, indicating upper motor neuron damage.
*Flaccid paralysis on the right side*
- **Anterior spinal artery syndrome** causes **bilateral motor deficits** due to involvement of both **corticospinal tracts** in the anterior cord.
- While initial presentation can be **flaccid paralysis** due to spinal shock below the level of the lesion, it is typically **bilateral**, not unilateral, and evolves to **spastic paralysis** over time.
Anterior cerebral artery territory US Medical PG Question 4: A 28-year-old man is brought to the emergency department by ambulance after developing an altered mental state following blunt trauma to the head. The patient was competing at a local mixed martial arts competition when he was struck in the head and lost consciousness. A few minutes later, upon regaining consciousness, he had a progressive decline in mental status. Past medical history is noncontributory. Upon arrival at the hospital, the temperature is 37.0°C (98.6°F), the blood pressure is 145/89 mm Hg, the pulse is 66/min, the respiratory rate is 14/min, and the oxygen saturation is 99% on room air. He is alert now. A noncontrast CT scan is performed, and the result is provided in the image. Which of the following structures is most likely affected in this patient?
- A. Subarachnoid space
- B. Suprasellar cistern
- C. Middle Meningeal artery (Correct Answer)
- D. Ventricular system
- E. Bridging veins
Anterior cerebral artery territory Explanation: ***Middle Meningeal artery***
- The CT scan shows a **lenticular** or **biconvex** shaped hemorrhage, characteristic of an **epidural hematoma**. This type of hematoma is typically caused by trauma leading to rupture of the middle meningeal artery.
- The history of blunt head trauma followed by a **lucid interval** and then progressive neurological decline strongly points to an epidural hematoma, which results from arterial bleeding.
*Subarachnoid space*
- Hemorrhage in the subarachnoid space (subarachnoid hemorrhage) typically appears as **blood filling the sulci and basal cisterns** on CT, not a localized collection like seen in the image.
- While subarachnoid hemorrhage can be traumatic, the classic presentation of an epidural hematoma (lucid interval, lenticular shape) is not consistent with primary subarachnoid bleeding.
*Suprasellar cistern*
- The suprasellar cistern is located at the base of the brain, superior to the sella turcica, and typically contains cerebrospinal fluid.
- While it can be affected by subarachnoid hemorrhage, the image clearly shows a hematoma in the temporal-parietal region, not specifically within the suprasellar cistern.
*Ventricular system*
- The ventricular system contains CSF and is an internal structure of the brain. Hemorrhage within the ventricles (intraventricular hemorrhage) would appear as blood filling the ventricular spaces.
- The image shows an extra-axial hematoma, meaning outside the brain parenchyma and ventricles.
*Bridging veins*
- Rupture of bridging veins typically causes a **subdural hematoma**, which appears as a **crescent-shaped** collection of blood along the surface of the brain, conforming to the contours of the cerebral hemisphere.
- The hematoma in the image has a **lenticular (biconvex)** shape, which is characteristic of an epidural hematoma, not a subdural hematoma.
Anterior cerebral artery territory US Medical PG Question 5: A 78-year-old left-handed woman with hypertension and hyperlipidemia is brought to the emergency room because of sudden-onset right leg weakness and urinary incontinence. Neurologic examination shows decreased sensation over the right thigh. Muscle strength is 2/5 in the right lower extremity and 4/5 in the right upper extremity. Strength and sensation in the face are normal but she has difficulty initiating sentences and she is unable to write her name. The most likely cause of this patient’s condition is an occlusion of which of the following vessels?
- A. Right vertebrobasilar artery
- B. Right middle cerebral artery
- C. Left posterior cerebral artery
- D. Left anterior cerebral artery (Correct Answer)
- E. Right anterior cerebral artery
Anterior cerebral artery territory Explanation: ***Left anterior cerebral artery***
- Stroke in the **left anterior cerebral artery (ACA)** territory typically causes **contralateral leg weakness** (right leg in this case) and **urinary incontinence** due to involvement of the paracentral lobule.
- The patient's difficulty writing her name (agraphia) and initiating sentences (transcortical motor aphasia, which can manifest as difficulty initiating speech) is consistent with damage to the supplemental motor area in the dominant (left) hemisphere, provided by the ACA.
*Right vertebrobasilar artery*
- Occlusion of the vertebrobasilar artery typically presents with a wide range of symptoms including **vertigo**, **ataxia**, **dysarthria**, and bilateral or alternating sensory/motor deficits.
- It would not selectively cause isolated right leg weakness, urinary incontinence, and dominant hemisphere language difficulties without other brainstem or cerebellar signs.
*Right middle cerebral artery*
- A stroke in the **right middle cerebral artery (MCA)** would cause **left-sided deficit**, not right-sided.
- Although it can cause motor and sensory deficits, it typically affects the arm and face more than the leg, and would not cause the specific language deficits of the dominant hemisphere seen here.
*Left posterior cerebral artery*
- Occlusion of the **left posterior cerebral artery (PCA)** typically leads to issues like **contralateral homonymous hemianopia**, visual field defects, and potentially memory impairment or alexia without agraphia if the splenium of the corpus callosum is involved.
- It directly affects posterior brain regions, so it would not cause the anterior cerebral artery specific symptoms such as prominent contralateral leg weakness, urinary incontinence, or the described language difficulties.
*Right anterior cerebral artery*
- Occlusion of the **right anterior cerebral artery (ACA)** would cause **left leg weakness** and **left-sided sensory deficits**, not the right-sided deficits observed in this patient.
- While it could cause urinary incontinence, the combination of right-sided weakness and dominant hemisphere language deficits points against a right ACA occlusion.
Anterior cerebral artery territory US Medical PG Question 6: A 50-year-old man undergoes parathyroidectomy for treatment-resistant hyperparathyroidism. The procedure is complicated by brisk bleeding from the superior thyroid artery near the external branch of the superior laryngeal nerve. To stop the bleeding, the artery is ligated at its origin. Which of the following is most likely the origin of the artery that was injured in this patient?
- A. Thyrocervical trunk
- B. Ascending pharyngeal artery
- C. Internal carotid artery
- D. Subclavian artery
- E. External carotid artery (Correct Answer)
Anterior cerebral artery territory Explanation: ***External carotid artery***
- The **superior thyroid artery** is the first branch to arise from the **external carotid artery** in the neck.
- Ligation of this artery at its origin is a common surgical maneuver to control bleeding during thyroid or parathyroid surgery.
*Thyrocervical trunk*
- The **thyrocervical trunk** is a branch of the **subclavian artery** and gives rise to the inferior thyroid artery, not the superior thyroid artery.
- Injury to the superior thyroid artery would not necessitate ligation of a vessel originating from the thyrocervical trunk.
*Ascending pharyngeal artery*
- The **ascending pharyngeal artery** is a small artery that branches from the **external carotid artery** but supplies the pharynx, not the thyroid gland.
- It is not typically implicated in bleeding during parathyroidectomy or in relation to the superior laryngeal nerve.
*Internal carotid artery*
- The **internal carotid artery** primarily supplies the brain and does not have branches in the neck that supply the thyroid or parathyroid glands.
- It arises from the common carotid artery but does not give off the superior thyroid artery.
*Subclavian artery*
- The **subclavian artery** gives rise to the **thyrocervical trunk**, which then supplies the inferior thyroid artery, but not directly the superior thyroid artery.
- The superior thyroid artery originates higher up from the external carotid artery.
Anterior cerebral artery territory US Medical PG Question 7: A 68-year-old man is brought to the emergency department by ambulance after he was found to be altered at home. Specifically, his wife says that he fell and was unable to get back up while walking to bed. When she approached him, she found that he was unable to move his left leg. His past medical history is significant for hypertension, atrial fibrillation, and diabetes. In addition, he has a 20-pack-year smoking history. On presentation, he is found to still have difficulty moving his left leg though motor function in his left arm is completely intact. The cause of this patient's symptoms most likely occurred in an artery supplying which of the following brain regions?
- A. Motor cortex (ACA) (Correct Answer)
- B. Cerebellum (PICA/SCA)
- C. Occipital cortex (PCA)
- D. Brainstem (Vertebrobasilar)
- E. Motor cortex (MCA)
Anterior cerebral artery territory Explanation: ***Motor cortex (ACA)***
- The patient's inability to move his **left leg** while his **left arm** remains intact points to an injury in the **right cerebral hemisphere** affecting the leg area of the motor cortex.
- The leg area of the **primary motor cortex** is primarily supplied by the **anterior cerebral artery (ACA)**, making an ACA stroke the most likely cause.
*Motor cortex (MCA)*
- The **middle cerebral artery (MCA)** primarily supplies the motor cortex areas responsible for the **face and arm**, not typically isolated leg weakness.
- If the MCA were affected, you would expect to see involvement of the face and/or arm on the contralateral side in addition to leg weakness.
*Brainstem (Vertebrobasilar)*
- A **brainstem stroke** would likely present with more widespread neurological deficits, including **cranial nerve palsies**, ataxia, or altered consciousness.
- Isolated contralateral leg weakness without arm involvement is not characteristic of a brainstem lesion.
*Cerebellum (PICA/SCA)*
- The **cerebellum** is primarily involved in **coordination and balance**, not direct motor strength.
- A cerebellar stroke would present with symptoms like **ataxia**, dysarthria, or nystagmus, not isolated paralysis.
*Occipital cortex (PCA)*
- The **occipital cortex** is primarily responsible for **vision**.
- A posterior cerebral artery (PCA) stroke would typically cause **visual field defects** (e.g., contralateral homonymous hemianopia) rather than motor weakness.
Anterior cerebral artery territory US Medical PG Question 8: A 36-year-old woman, gravida 1, para 1, has back pain and numbness in her lower extremities after an emergency cesarean delivery of a healthy 3856-g (8-lb, 8-oz) newborn male. She had a placental abruption and lost approximately 2000 ml of blood. During the procedure, she received two units of packed red blood cells and intravenous fluids. She has no history of serious illness and takes no medications. She is sexually active with one male partner, and they use condoms inconsistently. She is alert and oriented to person, place, and time. Her temperature is 37.2°C (98.9°F), pulse is 90/min, respirations are 15/min, and blood pressure is 94/58 mm Hg. Examination shows decreased sensation to temperature and pinprick below her waist and 0/5 muscle strength in her lower extremities. She feels the vibrations of a tuning fork placed on both of her great toes. Deep tendon reflexes are absent in the lower extremities and 2+ in the upper extremities. Which of the following is the most likely diagnosis?
- A. Posterior spinal artery syndrome
- B. Brown-Séquard syndrome
- C. Anterior spinal artery syndrome (Correct Answer)
- D. Guillain-Barré Syndrome
- E. Tabes dorsalis
Anterior cerebral artery territory Explanation: ***Anterior spinal artery syndrome***
- This syndrome is characterized by the sudden onset of **bilateral motor paralysis** below the level of the lesion, accompanied by a dissociated sensory loss (**loss of pain and temperature sensation**) while **proprioception and vibratory sensation are preserved**.
- The patient's history of **significant blood loss** and hypotension during delivery makes her susceptible to spinal cord ischemia, particularly in the anterior spinal artery territory, which supplies the anterior two-thirds of the spinal cord.
*Posterior spinal artery syndrome*
- This syndrome primarily affects the **dorsal columns**, leading to a loss of **proprioception and vibratory sensation**, with preservation of motor function and pain/temperature sensation.
- The patient's preserved vibratory sensation and significant motor deficits rule out posterior spinal artery syndrome.
*Brown-Séquard syndrome*
- This syndrome results from **hemitransverse lesion of the spinal cord**, causing **ipsilateral motor paralysis** and loss of proprioception/vibration below the lesion, and **contralateral loss of pain and temperature sensation**.
- The patient's **bilateral motor and sensory deficits** are inconsistent with the unilateral presentation of Brown-Séquard syndrome.
*Guillain-Barré Syndrome*
- GBS typically presents as an **ascending paralysis** with **areflexia**, but sensory loss is usually stocking-glove distribution and often involves proprioception, and it is a **peripheral neuropathy** not a spinal cord infarction.
- The acute, localized nature of the sensory and motor loss below the waist, along with preserved vibratory sensation, differentiates it from the more diffuse presentation of GBS.
*Tabes dorsalis*
- This is a late manifestation of **syphilis** affecting the **dorsal columns** and dorsal roots, characterized by ataxia, lancinating pains, and loss of proprioception and vibration sense.
- The acute onset of symptoms following a hypotensive episode, along with motor paralysis and preserved vibratory sensation, does not fit the chronic, dorsal column pathology of tabes dorsalis.
Anterior cerebral artery territory US Medical PG Question 9: A 65-year-old man presents with facial weakness. He says he noticed that his face appeared twisted when he looked in the bathroom mirror this morning. He is otherwise well and does not have any other complaints. He denies any facial pain or paresthesia. No significant past medical history. The patient is afebrile and vital signs are within normal limits. Neurological examination reveals difficulty shutting the right eye tight and inability to bring up the right corner of his mouth when asked to smile. Remainder of the exam, including the left side of the face, is unremarkable. Which of the following is the most likely diagnosis in this patient?
- A. Idiopathic facial paralysis (Correct Answer)
- B. Right hemisphere stroke
- C. Left middle cerebral artery stroke
- D. Facial nerve schwannoma
- E. Acoustic neuroma
Anterior cerebral artery territory Explanation: ***Idiopathic facial paralysis***
- The sudden onset of **unilateral facial weakness** affecting both the upper and lower face (inability to shut eye and inability to smile on the same side) without other neurological symptoms is characteristic of **Bell's palsy**.
- It is a diagnosis of exclusion, and the absence of other symptoms and normal vital signs support this benign, self-limiting condition.
*Right hemisphere stroke*
- A stroke typically causes **upper motor neuron facial weakness**, primarily affecting the **lower half of the contralateral face**, sparing the forehead.
- Would likely present with other neurological deficits such as **hemiparesis** or sensory changes, which are absent here.
*Left middle cerebral artery stroke*
- Similar to a right hemisphere stroke, a left MCA stroke would typically cause **contralateral facial weakness**, predominantly in the **lower face**.
- Would also likely present with additional symptoms such as **aphasia** (if the dominant hemisphere is affected) or right-sided motor/sensory deficits, which are not described.
*Facial nerve schwannoma*
- This condition tends to cause a **slowly progressive facial weakness**, not the acute onset described.
- Often associated with other symptoms such as **persistent facial pain** or paresthesia, which this patient denies.
*Acoustic neuroma*
- Primarily causes **hearing loss** and **tinnitus**, and later, **vestibular symptoms** like dizziness or imbalance.
- While it can eventually compress the facial nerve causing weakness, the onset would be gradual and accompanied by **auditory symptoms**, which are absent here.
Anterior cerebral artery territory US Medical PG Question 10: A 38-year-old man comes to the physician for a follow-up examination. He has quadriparesis as a result of a burst fracture of the cervical spine that occurred after a fall from his roof 1 month ago. He has urinary and bowel incontinence. He appears malnourished. His temperature is 37.1°C (98.8°F), pulse is 88/min, and blood pressure is 104/60 mm Hg. Examination shows spasticity in all extremities. Muscle strength is decreased in proximal and distal muscle groups bilaterally. Deep tendon reflexes are 4+ bilaterally. Plantar reflex shows extensor response bilaterally. Sensation to pinprick and temperature is absent below the neck. Sensation to vibration, position, and light touch is normal bilaterally. Rectal tone is decreased. There is a 1-cm area of erythema over the sacrum. Which of the following is the most likely cause of this patient's symptoms?
- A. Hemi-transection of the spinal cord
- B. Cavitation within the spinal cord
- C. Injury to gray matter of the spinal cord
- D. Occlusion of the posterior spinal artery
- E. Damage to the anterior spinal artery (Correct Answer)
Anterior cerebral artery territory Explanation: ***Damage to the anterior spinal artery***
- This typically results in **anterior cord syndrome**, characterized by bilateral loss of pain and temperature sensation, motor function (quadriparesis), and autonomic dysfunction (bowel/bladder incontinence below the level of injury).
- The **preservation of posterior column functions** (vibration, proprioception, light touch) is a hallmark of anterior spinal artery ischemia, as the posterior columns are supplied by the posterior spinal arteries.
*Hemi-transection of the spinal cord*
- This describes **Brown-Séquard syndrome**, which involves ipsilateral loss of motor function, vibration, and proprioception, and contralateral loss of pain and temperature sensation.
- The patient's symptoms are inconsistent with Brown-Séquard syndrome due to the **bilateral presentation of motor and sensory deficits**.
*Cavitation within the spinal cord*
- This condition, known as **syringomyelia**, typically presents with a **cape-like distribution of pain and temperature loss** (due to central cord involvement affecting the decussating spinothalamic fibers).
- It would usually spare motor function initially and would not explain the sudden, severe quadriparesis and complete sensory loss described.
*Injury to gray matter of the spinal cord*
- Isolated gray matter injury, often seen in conditions like **central cord syndrome**, primarily affects the pain and temperature pathways and may cause upper extremity weakness.
- It would not explain the **complete loss of motor function and pain/temperature sensation below the neck** while preserving posterior column function.
*Occlusion of the posterior spinal artery*
- Occlusion of the posterior spinal artery would primarily affect the **dorsal columns**, leading to loss of vibration, proprioception, and light touch.
- This patient, however, has **preserved sensation to vibration, position, and light touch**, making posterior spinal artery occlusion unlikely.
More Anterior cerebral artery territory US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.