Muscles and movements of lower limb US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Muscles and movements of lower limb. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Muscles and movements of lower limb US Medical PG Question 1: A 53-year-old multiparous woman is scheduled to undergo elective sling surgery for treatment of stress incontinence. She has frequent loss of small amounts of urine when she coughs or laughs, despite attempts at conservative treatment. The physician inserts trocars in the obturator foramen bilaterally to make the incision and passes a mesh around the pubic bones and underneath the urethra to form a sling. During the procedure, the physician accidentally injures a nerve in the obturator foramen. The function of which of the following muscles is most likely to be affected following the procedure?
- A. Obturator internus
- B. Tensor fascia latae
- C. Adductor longus (Correct Answer)
- D. Semitendinosus
- E. Transversus abdominis
Muscles and movements of lower limb Explanation: ***Adductor longus***
- The **obturator nerve** passes through the obturator foramen and innervates the **adductor muscles** of the thigh, including the **adductor longus**.
- Injury to the obturator nerve would therefore directly affect the function of the adductor longus, leading to impaired thigh adduction.
*Obturator internus*
- The **obturator internus** muscle is innervated by the **nerve to obturator internus**, which arises from the sacral plexus (L5-S2).
- This nerve does not pass through the obturator foramen, making injury to this muscle unlikely in this specific scenario.
*Tensor fascia latae*
- The **tensor fascia latae** is innervated by the **superior gluteal nerve** (L4-S1).
- The superior gluteal nerve is located deeper in the gluteal region and does not traverse the obturator foramen.
*Semitendinosus*
- The **semitendinosus** is one of the hamstring muscles and is innervated by the **tibial division of the sciatic nerve** (L5-S2).
- The sciatic nerve is located posteriorly in the thigh and does not pass through the obturator foramen.
*Transversus abdominis*
- The **transversus abdominis** muscle is innervated by the **thoracoabdominal nerves** (T7-T11) and the **subcostal nerve** (T12).
- These nerves supply the abdominal wall and are anatomically distant from the obturator foramen, hence injury is not expected.
Muscles and movements of lower limb US Medical PG Question 2: A 65-year-old man is referred by his primary care provider to a neurologist for leg pain. He reports a 6-month history of progressive bilateral lower extremity pain that is worse in his left leg. The pain is 5/10 in severity at its worst and is described as a "burning" pain. He has noticed that the pain is acutely worse when he walks downhill. He has started riding his stationary bike more often as it relieves his pain. His past medical history is notable for hypertension, diabetes mellitus, and a prior myocardial infarction. He also sustained a distal radius fracture the previous year after falling on his outstretched hand. He takes aspirin, atorvastatin, metformin, glyburide, enalapril, and metoprolol. He has a 30-pack-year smoking history and drinks 2-3 glasses of wine with dinner every night. His temperature is 99°F (37.2°C), blood pressure is 145/85 mmHg, pulse is 91/min, and respirations are 18/min. On exam, he is well-appearing and in no acute distress. A straight leg raise is negative. A valsalva maneuver does not worsen his pain. Which of the following is the most appropriate test to confirm this patient's diagnosis?
- A. Electromyography
- B. Ankle-brachial index
- C. Computerized tomography myelography
- D. Magnetic resonance imaging (Correct Answer)
- E. Radiography
Muscles and movements of lower limb Explanation: **Magnetic resonance imaging**
- **Magnetic resonance imaging (MRI)** is the most appropriate test for diagnosing **lumbar spinal stenosis** because it provides detailed imaging of soft tissues, including the **spinal cord, nerve roots, and intervertebral discs**.
- The patient's symptoms of bilateral lower extremity pain, worse with downhill walking and relieved by stationary biking (which typically involves a flexed spine), are classic for **neurogenic claudication** caused by spinal stenosis.
*Electromyography*
- **Electromyography (EMG)** measures electrical activity of muscles and can identify **radiculopathy** or **neuropathy** but does not directly visualize the spinal canal or its contents to diagnose the cause of nerve compression.
- While it could show nerve root involvement, it wouldn't be the primary diagnostic test to confirm **spinal stenosis** itself.
*Ankle-brachial index*
- The **ankle-brachial index (ABI)** is used to diagnose **peripheral artery disease (PAD)**, which can also cause leg pain with activity (**vascular claudication**).
- However, the patient's pain being worse with downhill walking and relieved by spine flexion (like on a stationary bike) is more consistent with **neurogenic claudication** than vascular claudication.
*Computerized tomography myelography*
- **CT myelography** involves injecting contrast into the spinal canal and then performing a CT scan. While it can visualize the spinal canal, it is more invasive than MRI and exposes the patient to **ionizing radiation**.
- It is typically reserved for cases where MRI is contraindicated (e.g., pacemakers) or when MRI findings are inconclusive.
*Radiography*
- **Radiography (X-rays)** can show bony changes such as **spondylosis** and **degenerative disc disease**, which are often associated with spinal stenosis.
- However, X-rays do not directly visualize the **spinal cord, nerve roots, or soft tissue compression**, making them inadequate for confirming spinal stenosis as the cause of neurogenic claudication.
Muscles and movements of lower limb US Medical PG Question 3: A 48-year-old male presents to his primary care provider with a two-week history of low back pain and left leg pain. He reports that his symptoms started while he was working at his job as a construction worker. He has since experienced intermittent achy pain over his lumbar spine. He has also noticed pain radiating into his left leg and weakness in left ankle dorsiflexion. On exam, he demonstrates the following findings on strength testing of the left leg: 5/5 in knee extension, 4/5 in ankle dorsiflexion, 4/5 in great toe extension, 5/5 in ankle plantarflexion, and 5/5 in great toe flexion. The patellar reflexes are 5/5 bilaterally. He is able to toe walk but has difficulty with heel walking. Weakness in which of the following compartments of the leg is most likely causing this patient’s foot drop?
- A. Lateral compartment
- B. Superficial posterior compartment
- C. Deep posterior compartment
- D. Anterior compartment (Correct Answer)
- E. Medial compartment
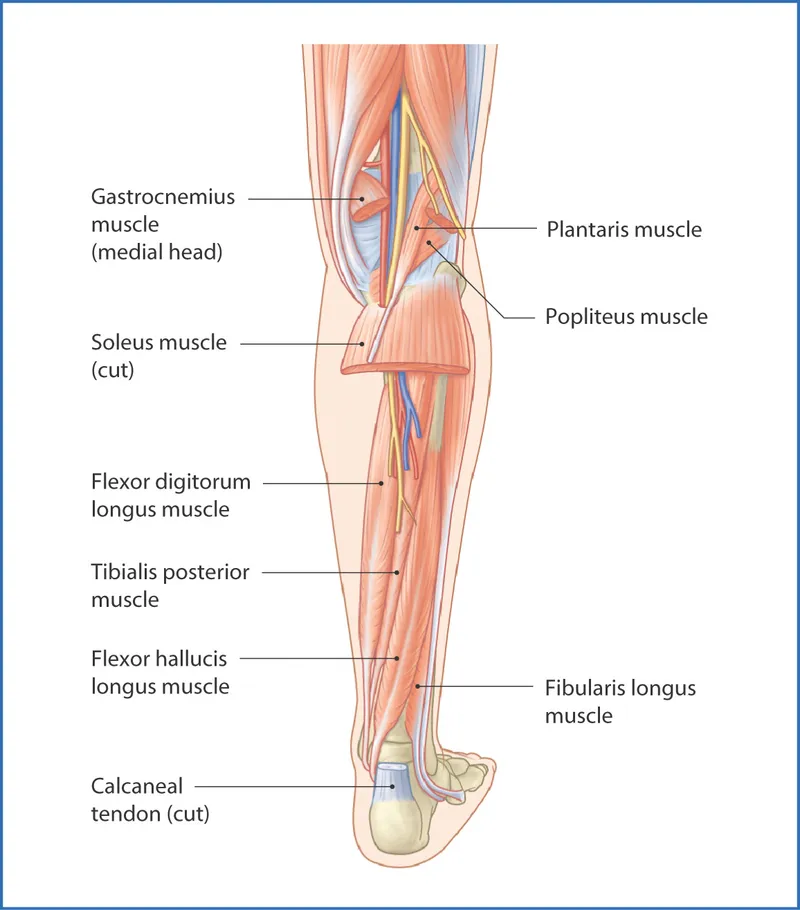
Muscles and movements of lower limb Explanation: ***Anterior compartment***
- Weakness in **ankle dorsiflexion** and **great toe extension**, coupled with difficulty **heel walking**, indicates a foot drop due to dysfunction of muscles in the anterior compartment, such as the **tibialis anterior**, **extensor hallucis longus**, and **extensor digitorum longus**.
- These muscles are primarily innervated by the **deep fibular nerve**, which is susceptible to compression from conditions like **lumbar radiculopathy** (L4-L5 nerve root involvement).
*Lateral compartment*
- Muscles in the lateral compartment (**fibularis longus** and **brevis**) are responsible for **eversion** of the foot.
- Weakness in this compartment would manifest as difficulty everting the foot, not primarily ankle dorsiflexion or great toe extension deficits.
*Superficial posterior compartment*
- This compartment contains muscles like the **gastrocnemius** and **soleus**, which are primarily responsible for **ankle plantarflexion**.
- The patient exhibits 5/5 strength in ankle plantarflexion and is able to toe walk, indicating these muscles are functioning well.
*Deep posterior compartment*
- Muscles in the deep posterior compartment (**tibialis posterior**, **flexor digitorum longus**, **flexor hallucis longus**) are involved in **inversion** and **toe flexion**.
- The patient has 5/5 strength in great toe flexion, suggesting intact function of these muscles, and his primary deficit is in dorsiflexion.
*Medial compartment*
- There is no distinct "medial compartment" of the leg in the anatomical sense comparable to the other listed compartments; rather, various muscles contribute to medial actions.
- The symptoms described specifically point to weakness in dorsiflexion and toe extension, localizing the problem to the anterior compartment.
Muscles and movements of lower limb US Medical PG Question 4: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Muscles and movements of lower limb Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Muscles and movements of lower limb US Medical PG Question 5: During a physical examination, a physician tests the strength of hip adduction against resistance. Which of the following nerves innervates the primary muscles responsible for this action?
- A. Sciatic nerve
- B. Superior gluteal nerve
- C. Femoral nerve
- D. Obturator nerve (Correct Answer)
Muscles and movements of lower limb Explanation: ***Obturator nerve***
- The **obturator nerve** primarily innervates the **adductor muscles** of the thigh, including the adductor longus, adductor brevis, adductor magnus (adductor part), gracilis, and pectineus (variable innervation).
- These muscles are responsible for **adducting the hip**, which is the action tested when a physician checks hip adduction strength against resistance.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (semitendinosus, semimembranosus, biceps femoris) and all muscles below the knee.
- It does not significantly contribute to the innervation of the primary hip adductors.
*Superior gluteal nerve*
- The **superior gluteal nerve** mainly innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae** muscles.
- These muscles are primarily involved in **hip abduction** and medial rotation, not adduction.
*Femoral nerve*
- The **femoral nerve** innervates the **quadriceps femoris muscles** (rectus femoris, vastus lateralis, vastus medialis, vastus intermedius) and the sartorius.
- Its primary actions are **knee extension** and hip flexion, with no direct role in hip adduction.
Muscles and movements of lower limb US Medical PG Question 6: A 26-year-old woman comes to the physician because of painful paresthesias in her foot. Examination shows decreased sensation in the first interdigital space and a hallux valgus deformity. This patient's paresthesias are most likely caused by compression of which of the following nerves?
- A. Saphenous nerve
- B. Sural nerve
- C. Superficial peroneal nerve
- D. Medial plantar nerve
- E. Deep peroneal nerve (Correct Answer)
Muscles and movements of lower limb Explanation: ***Deep peroneal nerve***
- The **deep peroneal nerve** provides sensation to the **first interdigital space** of the foot, and its compression would explain the described paresthesias.
- A **hallux valgus deformity** can alter foot mechanics and contribute to compression of this nerve.
*Saphenous nerve*
- The **saphenous nerve** provides sensory innervation to the **medial aspect of the lower leg and foot**, not specifically the interdigital spaces.
- Its compression is typically associated with pain or paresthesias in the medial calf or ankle.
*Sural nerve*
- The **sural nerve** provides sensation to the **lateral aspect of the foot and ankle**.
- Compression of this nerve would cause symptoms in a different distribution than described.
*Superficial peroneal nerve*
- The **superficial peroneal nerve** innervates the **dorsum of the foot**, excluding the first interdigital space and the area between the first and second toes.
- Compression would typically result in sensory changes over the top of the foot.
*Medial plantar nerve*
- The **medial plantar nerve** provides sensation to the **medial two-thirds of the plantar foot** and the **first 3.5 toes** on the plantar surface, not the dorsal interdigital space.
- Compression is often associated with symptoms similar to tarsal tunnel syndrome.
Muscles and movements of lower limb US Medical PG Question 7: A 45-year-old man is brought to the emergency department following a motor vehicle collision. He reports right hip pain and numbness along the right thigh. Physical examination shows decreased sensation to light touch over a small area of the proximal medial thigh. X-rays of the pelvis show a displaced pelvic ring fracture. Further evaluation of this patient is most likely to show which of the following findings?
- A. Sensory deficit of the dorsal foot
- B. Absent cremasteric reflex
- C. Impaired hip extension
- D. Impaired adduction of the hip (Correct Answer)
- E. Impaired extension of the knee
Muscles and movements of lower limb Explanation: ***Impaired adduction of the hip***
- The patient's **numbness along the right thigh** and **decreased sensation to light touch over the proximal medial thigh**, combined with a **pelvic ring fracture**, points to probable injury of the **obturator nerve**.
- The **obturator nerve** innervates the **adductor muscles** of the hip, and its injury would result in impaired hip adduction and sensory deficits in the medial thigh.
*Sensory deficit of the dorsal foot*
- A sensory deficit on the **dorsal foot** is typically associated with injury to the **peroneal nerve**, which is less likely to be affected by a pelvic ring fracture leading to medial thigh numbness.
- Peroneal nerve injury often results from trauma to the **lateral knee** or prolonged compression.
*Absent cremasteric reflex*
- An absent **cremasteric reflex** suggests injury to the **ilioinguinal** or **genitofemoral nerves**, or spinal cord injury at the L1-L2 level.
- While these nerves can be affected by pelvic trauma, the specific sensory deficit described (proximal medial thigh) aligns more with obturator nerve involvement.
*Impaired hip extension*
- **Hip extension** is primarily controlled by the **gluteus maximus** and **hamstrings**, which are innervated by the **inferior gluteal nerve** and **sciatic nerve**, respectively.
- Injury to these nerves or muscles would not typically cause numbness in the proximal medial thigh.
*Impaired extension of the knee*
- **Knee extension** is mediated by the **quadriceps femoris** muscle group, innervated by the **femoral nerve**.
- While the femoral nerve can be injured in severe pelvic trauma, the sensory distribution described does not match the typical sensory deficits of femoral nerve injury (anterior and medial thigh, medial leg).
Muscles and movements of lower limb US Medical PG Question 8: A 72-year-old male presents to a cardiac surgeon for evaluation of severe aortic stenosis. He has experienced worsening dyspnea with exertion over the past year. The patient also has a history of poorly controlled hypertension, diabetes mellitus, and hyperlipidemia. An echocardiogram revealed a thickened calcified aortic valve. The surgeon is worried that the patient will be a poor candidate for open heart surgery and decides to perform a less invasive transcatheter aortic valve replacement. In order to perform this procedure, the surgeon must first identify the femoral pulse just inferior to the inguinal ligament and insert a catheter into the vessel in order to gain access to the arterial system. Which of the following structures is immediately lateral to this structure?
- A. Lymphatic vessels
- B. Femoral vein
- C. Sartorius muscle
- D. Pectineus muscle
- E. Femoral nerve (Correct Answer)
Muscles and movements of lower limb Explanation: ***Femoral nerve***
- The **femoral nerve** lies lateral to the **femoral artery** within the **femoral triangle**.
- The order of structures from **lateral to medial** under the inguinal ligament is remembered by the mnemonic **NAVEL**: **N**erve, **A**rtery, **V**ein, **E**mpty space, **L**ymphatics.
*Lymphatic vessels*
- **Lymphatic vessels** and nodes are located most medially within the femoral triangle, medial to the femoral vein.
- This position is not immediately lateral to the femoral artery.
*Femoral vein*
- The **femoral vein** is located immediately medial to the **femoral artery**.
- It would not be found immediately lateral to the femoral artery.
*Sartorius muscle*
- The **sartorius muscle** forms the lateral boundary of the **femoral triangle** but is not immediately adjacent and lateral to the femoral artery within the triangle itself.
- The femoral nerve is enclosed within the iliopsoas fascial compartment, which runs deep to the sartorius.
*Pectineus muscle*
- The **pectineus muscle** forms part of the floor of the **femoral triangle**, but it is deep to the neurovascular structures.
- It is not immediately lateral to the femoral artery.
Muscles and movements of lower limb US Medical PG Question 9: A 32-year-old man comes to the physician because of a 1-month history of intermittent tingling of his hand. He is an avid cyclist and has recently started training for a cycle marathon. Physical examination shows decreased grip strength in the right hand and wasting of the hypothenar eminence. On asking the patient to grasp a piece of paper between his right thumb and right index finger in the first web space, there is hyperflexion of the right thumb interphalangeal joint. Which of the following additional findings is most likely in this patient?
- A. Loss of sensation over the dorsum of the medial half of the hand
- B. Inability to extend the ring finger at the metacarpophalangeal joint
- C. Inability to flex the index finger at the interphalangeal joints
- D. Loss of sensation over the palmar aspect of the middle finger
- E. Inability to extend the little finger at the proximal interphalangeal joints (Correct Answer)
Muscles and movements of lower limb Explanation: ***Inability to extend the little finger at the proximal interphalangeal joints***
- The patient's symptoms (tingling, decreased grip strength, hypothenar eminence wasting, and **Froment's sign**) indicate **ulnar nerve compression at Guyon's canal** (handlebar palsy) from cycling.
- The ulnar nerve innervates the **3rd and 4th lumbricals** (medial two), which extend the PIP and DIP joints of the ring and little fingers.
- The ulnar nerve also innervates the **interossei muscles**, which assist in MCP flexion and IP extension.
- Loss of these intrinsic muscles results in **claw hand deformity** affecting the 4th and 5th digits, with hyperextension at MCP joints and flexion (inability to extend) at PIP and DIP joints.
- This is a classic finding in ulnar nerve palsy.
*Inability to extend the ring finger at the metacarpophalangeal joint*
- Extension at the MCP joint is primarily performed by the **extensor digitorum** (innervated by the **radial nerve**).
- The patient's findings indicate ulnar nerve compression, not radial nerve injury.
- In ulnar nerve palsy, the unopposed extensor digitorum actually causes MCP **hyperextension**, not inability to extend.
*Inability to flex the index finger at the interphalangeal joints*
- Flexion of the index finger IP joints is controlled by **flexor digitorum superficialis** (FDS) and **flexor digitorum profundus** (FDP).
- Both muscles to the index finger are innervated by the **median nerve**, not the ulnar nerve.
- This finding would indicate median nerve injury (e.g., carpal tunnel syndrome or anterior interosseous syndrome).
*Loss of sensation over the palmar aspect of the middle finger*
- Palmar sensation of the middle finger is supplied by the **median nerve**.
- The ulnar nerve supplies sensation to the medial 1.5 digits (little finger and medial half of ring finger).
- This finding would indicate median nerve pathology, not ulnar nerve compression.
*Loss of sensation over the dorsum of the medial half of the hand*
- The **dorsal cutaneous branch of the ulnar nerve** branches approximately 5-8 cm proximal to the wrist and passes **superficially**, NOT through Guyon's canal.
- In **Guyon's canal compression** (handlebar palsy), the dorsal cutaneous branch is **SPARED**, so dorsal sensation remains intact.
- The patient would have palmar sensory loss over the medial 1.5 digits but **preserved dorsal sensation**.
- Loss of dorsal sensation would suggest a more proximal ulnar nerve lesion (at the elbow or forearm), not at the wrist.
Muscles and movements of lower limb US Medical PG Question 10: A 31-year-old woman with multiple sclerosis comes to the physician because of a 4-day history of cramps in her left leg. Physical examination shows flexion of the left hip and increased tone in the thigh muscles. A local anesthetic block of which of the following nerves would most likely improve this patient's condition the most?
- A. Inferior gluteal nerve
- B. Superior gluteal nerve
- C. Femoral nerve (Correct Answer)
- D. Sciatic nerve
- E. Obturator nerve
Muscles and movements of lower limb Explanation: ***Femoral nerve***
- The **femoral nerve** innervates the **iliacus** (a primary hip flexor) and the **rectus femoris** (part of the quadriceps that assists in hip flexion), as well as the entire **quadriceps femoris group** (responsible for knee extension and contributing to increased thigh muscle tone).
- In this patient with spasticity, **hip flexion** is caused by hypertonicity of iliopsoas and rectus femoris, while **increased tone in thigh muscles** reflects quadriceps involvement.
- Blocking the femoral nerve would relax these muscles, thereby improving the **cramps, hip flexion, and increased thigh tone**.
*Inferior gluteal nerve*
- The **inferior gluteal nerve** primarily innervates the **gluteus maximus muscle**, which is involved in hip extension and external rotation, not hip flexion.
- Blocking this nerve would not directly address the symptoms of increased thigh muscle tone and hip flexion.
*Superior gluteal nerve*
- The **superior gluteal nerve** mainly innervates the **gluteus medius, gluteus minimus**, and **tensor fasciae latae muscles**, which are involved in hip abduction and internal rotation.
- Its blockade would not relieve hip flexion or thigh muscle cramps.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (hip extension, knee flexion) and all muscles below the knee.
- While it affects leg muscles, it does not directly control the muscles causing **hip flexion and increased thigh tone** in this context.
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles** of the thigh (adductor longus, brevis, magnus, gracilis), leading to hip adduction.
- Blocking this nerve would not address hip flexion or the increased tone in the quadriceps muscles described.
More Muscles and movements of lower limb US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.