Clinical correlations of lower limb US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Clinical correlations of lower limb. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Clinical correlations of lower limb US Medical PG Question 1: A 36-year-old woman comes to the physician because of new onset limping. For the past 2 weeks, she has had a tendency to trip over her left foot unless she lifts her left leg higher while walking. She has not had any trauma to the leg. She works as a flight attendant and wears compression stockings to work. Her vital signs are within normal limits. Physical examination shows weakness of left foot dorsiflexion against minimal resistance. There is reduced sensation to light touch over the dorsum of the left foot, including the web space between the 1st and 2nd digit. Further evaluation is most likely to show which of the following?
- A. Decreased ankle jerk reflex
- B. Normal foot eversion
- C. Weak knee flexion
- D. Normal foot inversion (Correct Answer)
- E. Weak hip flexion
Clinical correlations of lower limb Explanation: ***Normal foot inversion***
- The patient's symptoms of **foot drop** and **sensory loss** on the dorsum of the foot, including the web space between the 1st and 2nd digits, point to an injury of the **common fibular (peroneal) nerve** or its deep branch.
- The **deep fibular nerve** innervates the muscles responsible for **dorsiflexion** (tibialis anterior, extensor digitorum longus, extensor hallucis longus) and provides sensation to the **first dorsal web space**. The **superficial fibular nerve** innervates muscles for **eversion** and provides sensation to the rest of the foot dorsum. The **tibial nerve** innervates muscles for **foot inversion** (tibialis posterior) and plantarflexion; because the fibular nerve is affected, **tibial nerve function**, including foot inversion, should remain intact.
*Decreased ankle jerk reflex*
- The **ankle jerk reflex** (achilles tendon reflex) primarily tests the S1 nerve root, mediated by the **tibial nerve**.
- A common fibular nerve lesion does not directly affect the tibial nerve, thus the **ankle jerk reflex** is expected to be normal.
*Normal foot eversion*
- **Foot eversion** is primarily mediated by the **peroneus longus** and **brevis muscles**, which are supplied by the **superficial fibular nerve**.
- A lesion of the common fibular nerve before its bifurcation would affect both the deep and superficial branches, leading to **weakness or absence of foot eversion**.
*Weak knee flexion*
- **Knee flexion** is primarily controlled by the **hamstring muscles** (semitendinosus, semimembranosus, biceps femoris), which are innervated by the **tibial nerve** and the **common fibular nerve's branch to the short head of the biceps femoris**.
- While the common fibular nerve does contribute to biceps femoris innervation, the primary muscles for knee flexion are supplied by the tibial nerve, and isolated common fibular nerve injury typically does not result in significant global knee flexion weakness.
*Weak hip flexion*
- **Hip flexion** is primarily performed by the **iliopsoas muscle**, which is innervated by the **femoral nerve** and direct branches from the lumbar plexus (L1-L3).
- Injury to the common fibular nerve, which is a branch of the sciatic nerve (L4-S2), does not affect the innervation of the **hip flexors**.
Clinical correlations of lower limb US Medical PG Question 2: Seven hours after undergoing left hip arthroplasty for chronic hip pain, a 67-year-old woman reports a prickling sensation in her left anteromedial thigh and lower leg. Neurologic examination shows left leg strength 3/5 on hip flexion and 2/5 on knee extension. Patellar reflex is decreased on the left. Sensation to pinprick and light touch are decreased on the anteromedial left thigh as well as medial lower leg. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Femoral nerve injury (Correct Answer)
- B. L5 radiculopathy
- C. Sural nerve injury
- D. S1 radiculopathy
- E. Fibular nerve injury
Clinical correlations of lower limb Explanation: ***Femoral nerve injury***
- The patient's symptoms—weakness in **hip flexion** (iliopsoas via femoral nerve) and **knee extension** (quadriceps via femoral nerve), decreased **patellar reflex** (femoral nerve), and sensory loss in the **anteromedial thigh** (femoral nerve) and **medial lower leg** (saphenous nerve, a branch of the femoral nerve)—are all consistent with femoral nerve dysfunction.
- **Hip arthroplasty procedures** can sometimes lead to iatrogenic femoral nerve damage due to retraction, compression, or direct injury during surgery, especially when positioning or using surgical instruments.
*L5 radiculopathy*
- L5 radiculopathy typically causes weakness in **foot dorsiflexion**, **eversion**, and **toe extension**, along with sensory loss over the **dorsum of the foot** and lateral lower leg, which does not match the patient's presentation.
- While it can cause hip abductor weakness, it would not explain the prominent **quadriceps weakness** and **decreased patellar reflex**.
*Sural nerve injury*
- The sural nerve provides sensation to the **posterolateral aspect of the lower leg** and lateral malleolus, and has no motor function to the hip or knee.
- Injury to this nerve would not account for the patient's **proximal weakness** or sensory loss in the anteromedial thigh.
*S1 radiculopathy*
- S1 radiculopathy typically leads to weakness in **plantarflexion**, **hip extension**, and an absent **Achilles reflex**, along with sensory loss over the lateral foot and sole.
- It would not explain the significant **quadriceps weakness**, **decreased patellar reflex**, or sensory changes in the anteromedial thigh.
*Fibular nerve injury*
- Fibular (peroneal) nerve injury primarily results in **foot drop** (weakness in dorsiflexion and eversion of the foot) and sensory loss over the **dorsum of the foot** and anterolateral lower leg.
- It does not affect hip flexion, knee extension, or the patellar reflex, nor does it cause sensory loss in the anteromedial thigh.
Clinical correlations of lower limb US Medical PG Question 3: A 60-year-old man seeks evaluation at a medical office due to leg pain while walking. He says the pain starts in his buttocks and extends to his thighs and down to his calves. Previously, the pain resolved with rest, but the pain now persists in his feet, even during rest. His past medical history is significant for diabetes mellitus, hypertension, and cigarette smoking. The vital signs are within normal limits. The physical examination shows an atrophied leg with bilateral loss of hair. Which of the following is the most likely cause of this patient’s condition?
- A. Thrombus formation
- B. Weakening of vessel wall
- C. Narrowing and calcification of vessels (Correct Answer)
- D. Decreased permeability of endothelium
- E. Peripheral emboli formation
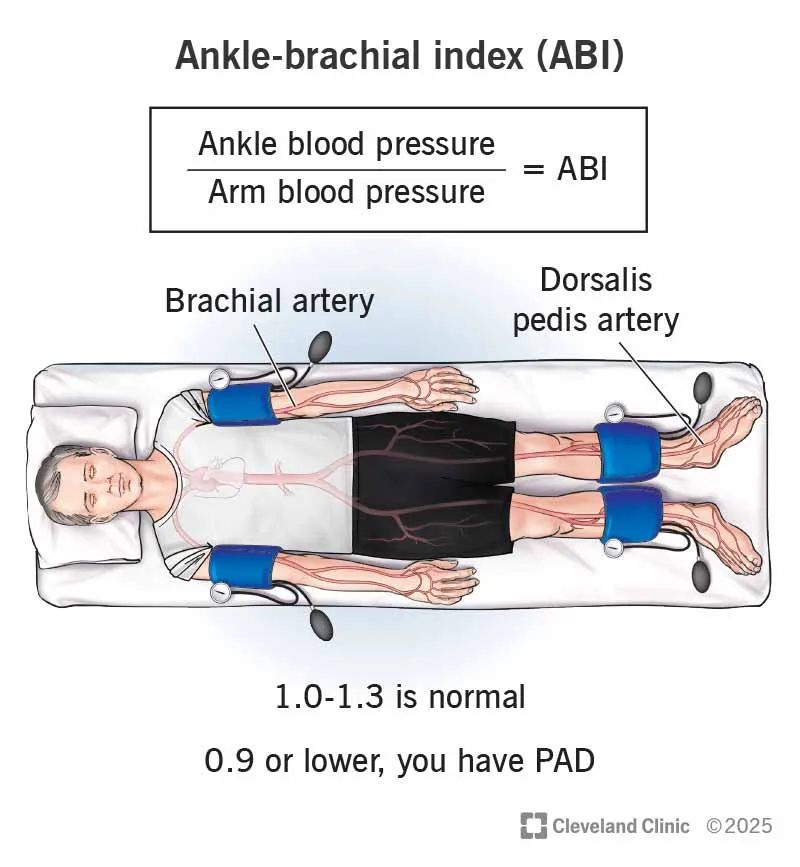
Clinical correlations of lower limb Explanation: ***Narrowing and calcification of vessels***
- This describes **atherosclerosis**, the most common cause of **peripheral artery disease (PAD)**, which presents with **intermittent claudication** (leg pain with walking, improving with rest) progressing to **rest pain**, especially in the feet.
- The patient's risk factors (**diabetes, hypertension, smoking**) and physical findings (**atrophied leg, hair loss**) are highly consistent with chronic ischemia due to atherosclerosis.
*Thrombus formation*
- While thrombus formation can cause acute limb ischemia, the patient's symptoms are chronic and progressive, evolving over time from claudication to rest pain, which is more characteristic of gradual **atherosclerotic narrowing**.
- Acute thrombosis typically leads to a sudden onset of severe pain, pallor, pulselessness, paresthesias, and paralysis, which are not described here.
*Weakening of vessel wall*
- Weakening of the vessel wall is associated with conditions like **aneurysms** or dissections, which typically present with different symptoms (e.g., pulsatile masses, sudden severe chest/back pain).
- It does not directly explain the progressive ischemic symptoms described, such as claudication and rest pain from inadequate blood flow.
*Decreased permeability of endothelium*
- Decreased permeability of the endothelium generally implies difficulty in substances passing through the vessel wall, which is not directly linked to the pathophysiology of ischemic pain and tissue atrophy observed in this patient.
- Conditions affecting endothelial permeability often relate to inflammation, edema, or microvascular dysfunction, but not the macrovascular obstruction causing PAD.
*Peripheral emboli formation*
- Emboli can cause acute peripheral artery occlusion, leading to sudden onset severe limb pain and signs of ischemia.
- However, the patient's symptoms have progressed chronically over time, starting with intermittent claudication and worsening to rest pain, which is more indicative of a gradual atherosclerotic process rather than an acute embolic event.
Clinical correlations of lower limb US Medical PG Question 4: A 38-year-old man is brought to the emergency department after suffering a motor vehicle accident as the passenger. He had no obvious injuries, but he complains of excruciating right hip pain. His right leg is externally rotated, abducted, and extended at the hip and the femoral head can be palpated anterior to the pelvis. Plain radiographs of the pelvis reveal a right anterior hip dislocation and femoral head fracture. Which sensory and motor deficits are most likely in this patient's right lower extremity?
- A. Loss of sensation laterally below the knee, weak thigh extension and knee flexion
- B. Numbness of the ipsilateral scrotum and upper medial thigh
- C. Sensory loss to the dorsal surface of the foot and part of the anterior lower and lateral leg and foot drop
- D. Paresis and numbness of the medial thigh and medial side of the calf, weak hip flexion and knee extension
- E. Numbness of the medial side of the thigh and inability to adduct the thigh (Correct Answer)
Clinical correlations of lower limb Explanation: ***Numbness of the medial side of the thigh and inability to adduct the thigh***
- An **anterior hip dislocation** is caused by forced **abduction** and **external rotation**, putting the **obturator nerve** at risk due to its anatomical course through the **obturator foramen** and proximity to the hip joint.
- Damage to the **obturator nerve** (L2-L4) results in **sensory loss** over the **medial thigh** and paralysis of the **adductor muscles** (adductor longus, brevis, magnus, gracilis), leading to an inability to adduct the thigh.
*Loss of sensation laterally below the knee, weak thigh extension and knee flexion*
- **Sensory loss laterally below the knee** and **weak thigh extension/knee flexion** are characteristic of **sciatic nerve** or common **peroneal nerve injury**, which is more common in **posterior hip dislocations**.
- The presented case describes an **anterior dislocation**, making **obturator nerve** injury more likely than sciatic nerve injury.
*Numbness of the ipsilateral scrotum and upper medial thigh*
- **Numbness of the ipsilateral scrotum** and **upper medial thigh** is associated with injury to the **ilioinguinal nerve** or **genitofemoral nerve**.
- While these nerves supply portions of the **medial thigh** and **genitalia**, they are not typically injured in **anterior hip dislocations** which primarily affect deeper structures like the **obturator nerve**.
*Sensory loss to the dorsal surface of the foot and part of the anterior lower and lateral leg and foot drop*
- **Sensory loss to the dorsal surface of the foot**, **anterior lower and lateral leg**, and **foot drop** are classic signs of **common peroneal nerve** injury due to its superficial course around the fibular head.
- Although the common peroneal nerve is a branch of the **sciatic nerve**, direct injury specifically to the **common peroneal nerve** in an anterior hip dislocation is less probable than obturator nerve injury, and foot drop is characteristic of more severe neural compromise, typically seen in **posterior dislocations or direct trauma**.
*Paresis and numbness of the medial thigh and medial side of the calf, weak hip flexion and knee extension*
- **Paresis and numbness of the medial thigh** are consistent with **obturator nerve** injury. However, **numbness of the medial side of the calf** and **weak hip flexion/knee extension** point towards **femoral nerve** injury.
- While the **femoral nerve** can be injured, the prominent clinical picture of **anterior hip dislocation** points more directly to the **obturator nerve** findings of medial thigh numbness and adduction weakness, rather than primarily femoral nerve symptoms.
Clinical correlations of lower limb US Medical PG Question 5: A 25-year-old man presents to the emergency department after a car accident. He was the front seat restrained driver in a head-on collision. He has no significant past medical history. The patient’s vitals are stabilized and he is ultimately discharged with his injuries appropriately treated. At the patient’s follow up primary care appointment, he complains of being unable to lift his left foot. He otherwise states that he feels well and is not in pain. His vitals are within normal limits. Physical exam is notable for 1/5 strength upon dorsiflexion of the patient’s left foot, and 5/5 plantarflexion of the same foot. Which of the following initial injuries most likely occurred in this patient?
- A. Lisfranc fracture
- B. Calcaneal fracture
- C. Tibial plateau fracture
- D. Distal femur fracture
- E. Fibular neck fracture (Correct Answer)
Clinical correlations of lower limb Explanation: ***Fibular neck fracture***
- A fracture of the **fibular neck** can damage the **common peroneal nerve**, which wraps around this region.
- Injury to the common peroneal nerve typically causes **foot drop** (inability to dorsiflex the foot) and sensory loss on the dorsum of the foot, matching the patient's symptoms of 1/5 strength upon dorsiflexion.
*Lisfranc fracture*
- This is an injury to the **midfoot tarsometatarsal joints**, often causing severe pain, swelling, and inability to bear weight.
- While it can occur in high-impact trauma, it primarily affects the **structural integrity of the foot** and does not directly cause isolated foot drop through nerve damage.
*Calcaneal fracture*
- A fracture of the **heel bone** typically results from axial loading injuries (e.g., falls from height), causing severe heel pain, swelling, and gait disturbance.
- It does not directly affect the common peroneal nerve or lead to isolated **foot drop**.
*Tibial plateau fracture*
- A fracture of the **proximal tibia** involves the knee joint and often results from significant valgus or varus force, presenting with knee pain, swelling, and instability.
- While it can be associated with soft tissue injuries, isolated **foot drop** via common peroneal nerve injury is less directly linked than with a fibular neck fracture.
*Distal femur fracture*
- A fracture of the **lower part of the thigh bone** typically presents with severe pain, swelling, and deformity of the thigh and knee, often due to significant trauma.
- This type of fracture is not directly associated with damage to the common peroneal nerve or isolated **foot drop**.
Clinical correlations of lower limb US Medical PG Question 6: A 56-year-old man presents to the emergency room after being in a motor vehicle accident. He was driving on an icy road when his car swerved off the road and ran head on into a tree. He complains of severe pain in his right lower extremity. He denies loss of consciousness during the accident. His past medical history is notable for poorly controlled hypertension, hyperlipidemia, and major depressive disorder. He takes enalapril, atorvastatin, and sertraline. His temperature is 99.1°F (37.3°C), blood pressure is 155/85 mmHg, pulse is 110/min, and respirations are 20/min. On exam, he is alert and fully oriented. He is unable to move his right leg due to pain. Sensation is intact to light touch in the sural, saphenous, tibial, deep peroneal, and superficial peroneal distributions. His leg appears adducted, flexed, and internally rotated. An anteroposterior radiograph of his pelvis would most likely demonstrate which of the following findings?
- A. Fracture line extending between the greater and lesser trochanters
- B. Femoral head larger than contralateral side and inferior to acetabulum
- C. Fracture line extending through the femoral neck
- D. Fracture line extending through the subtrochanteric region of the femur
- E. Femoral head smaller than contralateral side and posterior to acetabulum (Correct Answer)
Clinical correlations of lower limb Explanation: ***Femoral head smaller than contralateral side and posterior to acetabulum***
- This presentation is consistent with a **posterior hip dislocation**, which typically occurs with an **axial load** on a flexed hip, common in head-on collisions.
- On radiographs, the femoral head appears **smaller** due to magnification differences and is displaced **posteriorly** relative to the acetabulum. The affected leg is classically **shortened, adducted, and internally rotated**.
*Fracture line extending between the greater and lesser trochanters*
- This describes an **intertrochanteric hip fracture**, which typically presents with the leg **externally rotated** and **abducted**, not internally rotated and adducted.
- While caused by trauma, the clinical presentation does not align with the patient's physical exam findings.
*Femoral head larger than contralateral side and inferior to acetabulum*
- This describes an **anterior hip dislocation**, which is far less common and would present with the leg typically held in **abduction** and **external rotation**. The femoral head would also appear **larger** due to magnification from being anteriorly displaced.
- The patient's presentation of adduction and internal rotation is inconsistent with an anterior dislocation.
*Fracture line extending through the femoral neck*
- A **femoral neck fracture** usually presents with the leg in **external rotation** and **shortening**, and often involves older patients with osteoporosis after falls.
- While a severe impact could cause this, the characteristic adduction and internal rotation point more strongly to a dislocation.
*Fracture line extending through the subtrochanteric region of the femur*
- A **subtrochanteric fracture** involves the shaft of the femur just below the trochanters and commonly presents with significant pain and inability to bear weight.
- This type of fracture does not typically result in the specific adducted and internally rotated leg position seen with hip dislocations.
Clinical correlations of lower limb US Medical PG Question 7: A 24-year-old professional soccer player presents to the clinic with discomfort and pain while walking. He says that he has an unstable knee joint that started after an injury during a match last week. He adds that he heard a popping sound at the time of the injury. Physical examination of the knee reveals swelling of the knee joint with a positive anterior drawer test. Which of the following structures is most likely damaged in this patient?
- A. Lateral collateral ligament
- B. Ligamentum patellae
- C. Anterior cruciate ligament (Correct Answer)
- D. Medial collateral ligament
- E. Posterior cruciate ligament
Clinical correlations of lower limb Explanation: ***Anterior cruciate ligament***
- The **"popping sound"** at the time of injury, associated with knee **instability** and a **positive anterior drawer test**, are classic signs of an **ACL tear**.
- The **anterior drawer test** specifically assesses the integrity of the ACL by checking for excessive anterior translation of the tibia relative to the femur.
*Lateral collateral ligament*
- Injury to the LCL typically results from a **varus stress** to the knee and is less commonly associated with a distinct "popping" sound or significant instability.
- While it causes pain and instability, the **anterior drawer test** would likely be negative, and a **varus stress test** would be more indicative.
*Ligamentum patellae*
- Damage to the patellar ligament usually presents as pain and difficulty with knee extension, often following a forceful quadriceps contraction.
- It does not typically cause the described popping sensation or knee instability assessed by the anterior drawer test.
*Medial collateral ligament*
- MCL injuries commonly result from a **valgus stress** (force to the outside of the knee) and are diagnosed with a **valgus stress test**, not the anterior drawer test.
- While it can cause instability, the "popping" sound and specific findings of the anterior drawer test point away from an isolated MCL injury.
*Posterior cruciate ligament*
- A PCL injury is often associated with a **posteriorly directed force** to the tibia, such as a dashboard injury, and would present with a **positive posterior drawer test**.
- The clinical presentation of a **positive anterior drawer test** and significant anterior instability rules out isolated PCL damage.
Clinical correlations of lower limb US Medical PG Question 8: Three days after undergoing laparoscopic colectomy, a 67-year-old man reports swelling and pain in his right leg. He was diagnosed with colon cancer 1 month ago. His temperature is 38.5°C (101.3°F). Physical examination shows swelling of the right leg from the ankle to the thigh. There is no erythema or rash. Which of the following is likely to be most helpful in establishing the diagnosis?
- A. D-dimer level
- B. Compression ultrasonography (Correct Answer)
- C. CT pulmonary angiography
- D. Transthoracic echocardiography
- E. Blood cultures
Clinical correlations of lower limb Explanation: ***Compression ultrasonography***
- This patient's presentation with **unilateral leg swelling and pain** after surgery, especially given his recent **colon cancer diagnosis** (a hypercoagulable state), is highly suspicious for a **deep vein thrombosis (DVT)**.
- **Compression ultrasonography** is the gold standard, non-invasive imaging modality for diagnosing DVT, allowing direct visualization of thrombi and assessing venous compressibility.
*D-dimer level*
- While a **positive D-dimer** indicates recent or ongoing clot formation, it is **non-specific** and can be elevated in many conditions, including surgery, cancer, and infection.
- A normal D-dimer can rule out DVT in low-probability patients, but a high D-dimer in a high-probability patient (like this case) requires further imaging for confirmation, making it less definitive than ultrasound.
*CT pulmonary angiography*
- This imaging is used to diagnose a **pulmonary embolism (PE)**, which is a complication of DVT, but the primary symptoms here are localized to the leg.
- While PE is a concern, diagnosing the source (DVT) in the leg is the immediate priority for treatment and prevention of future complications.
*Transthoracic echocardiography*
- **Echocardiography** evaluates cardiac structure and function and can sometimes detect large clots in the right heart leading to PE, but it is not the primary diagnostic tool for DVT in the leg.
- It would be done if signs of cardiac strain or shunting associated with acute PE were prominent, which is not the case here.
*Blood cultures*
- **Blood cultures** are used to diagnose **bacteremia or sepsis**, which might explain a fever, but the prominent, unilateral leg swelling and pain are not typical for a primary infectious cause in the leg without local signs of cellulitis or abscess.
- While a low-grade fever is present, the absence of erythema or rash makes a primary infectious etiology less likely than DVT given the risk factors.
Clinical correlations of lower limb US Medical PG Question 9: A 45-year-old male presents to his primary care provider with an abnormal gait. He was hospitalized one week prior for acute cholecystitis and underwent a laparoscopic cholecystectomy. He received post-operative antibiotics via intramuscular injection. He recovered well and he was discharged on post-operative day #3. However, since he started walking after the operation, he noticed a limp that has not improved. On exam, his left hip drops every time he raises his left foot to take a step. In which of the following locations did this patient likely receive the intramuscular injection?
- A. Superomedial quadrant of the buttock (Correct Answer)
- B. Superolateral quadrant of the buttock
- C. Anteromedial thigh
- D. Inferomedial quadrant of the buttock
- E. Inferolateral quadrant of the buttock
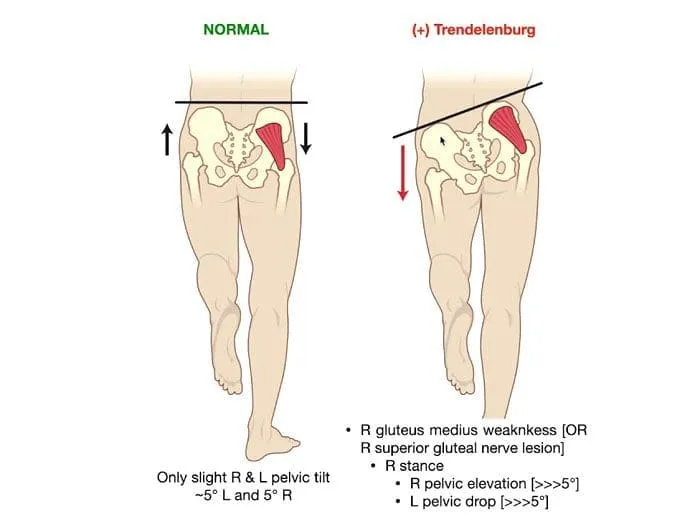
Clinical correlations of lower limb Explanation: ***Superomedial quadrant of the buttock***
- An injection in the **superomedial quadrant of the buttock** is the most common site for iatrogenic injury to the **superior gluteal nerve**.
- The superior gluteal nerve exits the pelvis through the greater sciatic foramen above the piriformis muscle and runs in the **superomedial** region of the buttock.
- Injury to the superior gluteal nerve results in weakness of the **gluteus medius and minimus muscles**, leading to a **Trendelenburg gait** (hip drops on the contralateral side when lifting that leg), which is consistent with the patient's symptoms.
- This is why the **superolateral quadrant** is recommended for safe IM injections.
*Superolateral quadrant of the buttock*
- The **superolateral quadrant** is the **safest site** for intramuscular gluteal injections precisely because it avoids the superior gluteal nerve.
- This is the recommended injection site to prevent the complication that this patient experienced.
- An injection here would not cause superior gluteal nerve injury or Trendelenburg gait.
*Inferomedial quadrant of the buttock*
- Injections in the **inferomedial quadrant** put the **sciatic nerve** at significant risk of injury.
- Sciatic nerve injury would lead to symptoms affecting the posterior thigh and lower leg, such as **foot drop, loss of ankle reflexes, or paresthesias in the posterior leg and foot**, not isolated hip abductor weakness.
*Inferolateral quadrant of the buttock*
- This area is close to the **sciatic nerve** and **inferior gluteal nerve**.
- Inferior gluteal nerve injury would affect the **gluteus maximus**, leading to difficulty with hip extension (trouble climbing stairs, rising from a chair), not a Trendelenburg gait.
- Sciatic nerve injury would present with foot drop and sensory deficits.
*Anteromedial thigh*
- Injections in the **anteromedial thigh** could injure the **femoral nerve** or its branches.
- This would cause **quadriceps weakness** with impaired knee extension and difficulty walking (buckling knee), not hip abductor weakness or Trendelenburg gait.
- The femoral nerve does not control hip abduction.
Clinical correlations of lower limb US Medical PG Question 10: A 48-year-old male presents to his primary care provider with a two-week history of low back pain and left leg pain. He reports that his symptoms started while he was working at his job as a construction worker. He has since experienced intermittent achy pain over his lumbar spine. He has also noticed pain radiating into his left leg and weakness in left ankle dorsiflexion. On exam, he demonstrates the following findings on strength testing of the left leg: 5/5 in knee extension, 4/5 in ankle dorsiflexion, 4/5 in great toe extension, 5/5 in ankle plantarflexion, and 5/5 in great toe flexion. The patellar reflexes are 5/5 bilaterally. He is able to toe walk but has difficulty with heel walking. Weakness in which of the following compartments of the leg is most likely causing this patient’s foot drop?
- A. Lateral compartment
- B. Superficial posterior compartment
- C. Deep posterior compartment
- D. Anterior compartment (Correct Answer)
- E. Medial compartment
Clinical correlations of lower limb Explanation: ***Anterior compartment***
- Weakness in **ankle dorsiflexion** and **great toe extension**, coupled with difficulty **heel walking**, indicates a foot drop due to dysfunction of muscles in the anterior compartment, such as the **tibialis anterior**, **extensor hallucis longus**, and **extensor digitorum longus**.
- These muscles are primarily innervated by the **deep fibular nerve**, which is susceptible to compression from conditions like **lumbar radiculopathy** (L4-L5 nerve root involvement).
*Lateral compartment*
- Muscles in the lateral compartment (**fibularis longus** and **brevis**) are responsible for **eversion** of the foot.
- Weakness in this compartment would manifest as difficulty everting the foot, not primarily ankle dorsiflexion or great toe extension deficits.
*Superficial posterior compartment*
- This compartment contains muscles like the **gastrocnemius** and **soleus**, which are primarily responsible for **ankle plantarflexion**.
- The patient exhibits 5/5 strength in ankle plantarflexion and is able to toe walk, indicating these muscles are functioning well.
*Deep posterior compartment*
- Muscles in the deep posterior compartment (**tibialis posterior**, **flexor digitorum longus**, **flexor hallucis longus**) are involved in **inversion** and **toe flexion**.
- The patient has 5/5 strength in great toe flexion, suggesting intact function of these muscles, and his primary deficit is in dorsiflexion.
*Medial compartment*
- There is no distinct "medial compartment" of the leg in the anatomical sense comparable to the other listed compartments; rather, various muscles contribute to medial actions.
- The symptoms described specifically point to weakness in dorsiflexion and toe extension, localizing the problem to the anterior compartment.
More Clinical correlations of lower limb US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.