Bones and joints of lower limb US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Bones and joints of lower limb. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Bones and joints of lower limb US Medical PG Question 1: A 27-year-old man comes to the physician because of pain and swelling in his right knee that began 3 days ago when he fell during football practice. He fell on his flexed right knee as he dove to complete a pass. He felt some mild knee pain but continued to practice. Over the next 2 days, the pain worsened and the knee began to swell. Today, the patient has an antalgic gait. Examination shows a swollen and tender right knee; flexion is limited by pain. The right knee is flexed and pressure is applied to proximal tibia; 8 mm of backward translation of the foreleg is observed. Which of the following is most likely injured?
- A. Posterior cruciate ligament (Correct Answer)
- B. Anterior cruciate ligament
- C. Medial collateral ligament
- D. Lateral collateral ligament
- E. Lateral meniscus
Bones and joints of lower limb Explanation: ***Posterior cruciate ligament***
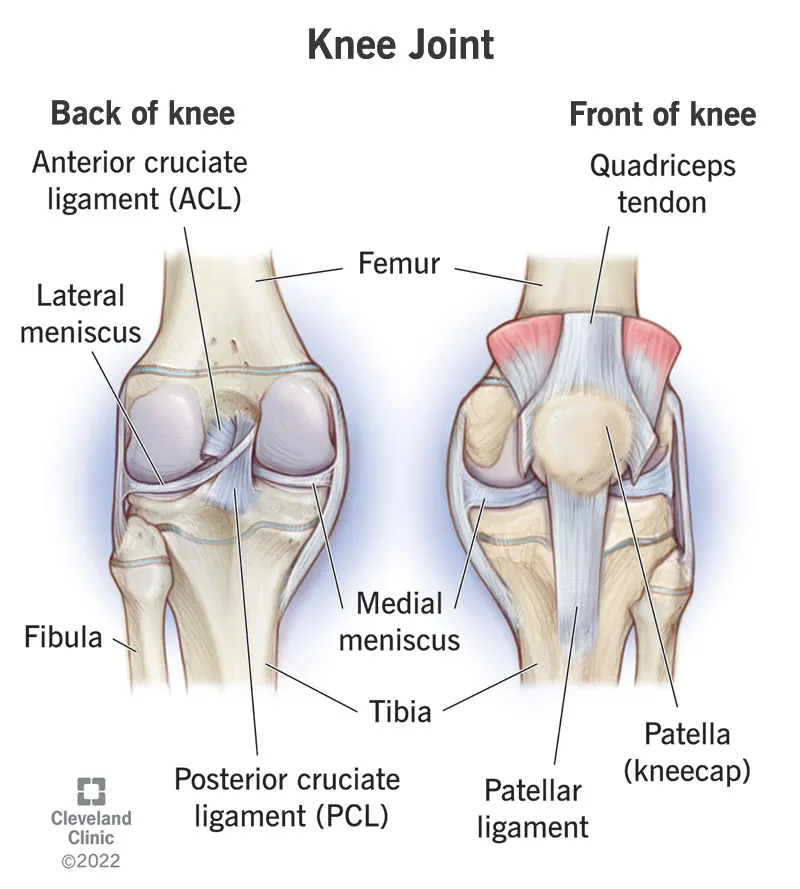
- The mechanism of injury, falling on a **flexed knee** with direct impact to the **proximal tibia**, is classic for a **posterior cruciate ligament (PCL)** injury.
- The finding of **8 mm of backward translation** of the foreleg with pressure applied to the proximal tibia (positive **posterior drawer test**) is diagnostic for PCL injury.
*Anterior cruciate ligament*
- **Anterior cruciate ligament (ACL)** injuries typically result from sudden stopping, pivoting, or direct blows to the **front of the knee**, often causing **anterior translation** of the tibia.
- The **anterior drawer test** or **Lachman test** would show increased anterior translation, not posterior.
*Medial collateral ligament*
- **Medial collateral ligament (MCL)** injuries usually occur due to a force applied to the **outside of the knee** (valgus stress), causing instability on the medial side.
- Associated with tenderness over the medial knee joint line and instability with **valgus stress testing**.
*Lateral collateral ligament*
- **Lateral collateral ligament (LCL)** injuries typically result from a force applied to the **inside of the knee** (varus stress), leading to instability on the lateral aspect.
- Associated with tenderness over the lateral knee joint line and instability with **varus stress testing**.
*Lateral meniscus*
- **Meniscal injuries** often present with mechanical symptoms such as clicking, locking, or catching, and pain that might worsen with specific movements like twisting or squatting.
- While a fall could potentially injure the meniscus, the specific finding of **posterior tibial translation** points more directly to a ligamentous injury.
Bones and joints of lower limb US Medical PG Question 2: A 19-year-old recent ROTC male recruit presents to the university clinic with left foot pain. He reports that the pain started a week ago while running morning drills. The pain will improve with rest but will occur again during exercises or during long periods of standing. He denies any recent trauma. His medical history is significant for partial color blindness. He has no other chronic medical conditions and takes no medications. He denies any surgical history. His family history is significant for schizophrenia in his father and breast cancer in his mother. He denies tobacco, alcohol, or illicit drug use. On physical examination, there is tenderness to palpation of the second metatarsal of the left foot. A radiograph of the left foot shows no abnormalities. Which of the following is the best next step in management?
- A. Splinting
- B. MRI
- C. Rest and ibuprofen (Correct Answer)
- D. Casting
- E. Internal fixation
Bones and joints of lower limb Explanation: ***Rest and ibuprofen***
- The patient's presentation of gradual onset foot pain in a **military recruit** that worsens with activity and improves with rest, with focal metatarsal tenderness, is highly suggestive of a **stress fracture**. Initial radiographs are often normal in early stress fractures, and conservative management with **rest and NSAIDs** like ibuprofen is the first-line treatment.
- This approach aims to reduce inflammation and pain, allowing the bone to heal while preventing further stress and injury.
*Splinting*
- While splinting can provide support and pain relief, it is generally considered for more severe or unstable injuries, or as an adjunct to rest and medication if symptoms are not adequately controlled.
- It's a more restrictive measure that might not be necessary for an initial, unconfirmed stress fracture of this nature.
*MRI*
- An MRI would be the next step if symptoms persist or worsen despite conservative management, or if there is diagnostic uncertainty.
- It is highly sensitive for detecting **stress reactions** and early stress fractures that are not visible on plain radiographs but is not the immediate first step for an uncomplicated presentation.
*Casting*
- Casting provides rigid immobilization and is typically reserved for confirmed, more severe, or unstable stress fractures, or those that fail to heal with rest and non-pharmacological interventions.
- Applying a cast for an initial, suspected stress fracture where conservative measures haven't been tried would be overly aggressive.
*Internal fixation*
- **Internal fixation** is a surgical procedure considered for complicated stress fractures, such as those at high risk of **non-union** or displacement (e.g., in the femoral neck, anterior tibial cortex), or if conservative management and casting fail.
- It is a highly invasive approach and would be inappropriate as the initial management strategy for this patient's presentation.
Bones and joints of lower limb US Medical PG Question 3: A 38-year-old man is brought to the emergency department after suffering a motor vehicle accident as the passenger. He had no obvious injuries, but he complains of excruciating right hip pain. His right leg is externally rotated, abducted, and extended at the hip and the femoral head can be palpated anterior to the pelvis. Plain radiographs of the pelvis reveal a right anterior hip dislocation and femoral head fracture. Which sensory and motor deficits are most likely in this patient's right lower extremity?
- A. Loss of sensation laterally below the knee, weak thigh extension and knee flexion
- B. Numbness of the ipsilateral scrotum and upper medial thigh
- C. Sensory loss to the dorsal surface of the foot and part of the anterior lower and lateral leg and foot drop
- D. Paresis and numbness of the medial thigh and medial side of the calf, weak hip flexion and knee extension
- E. Numbness of the medial side of the thigh and inability to adduct the thigh (Correct Answer)
Bones and joints of lower limb Explanation: ***Numbness of the medial side of the thigh and inability to adduct the thigh***
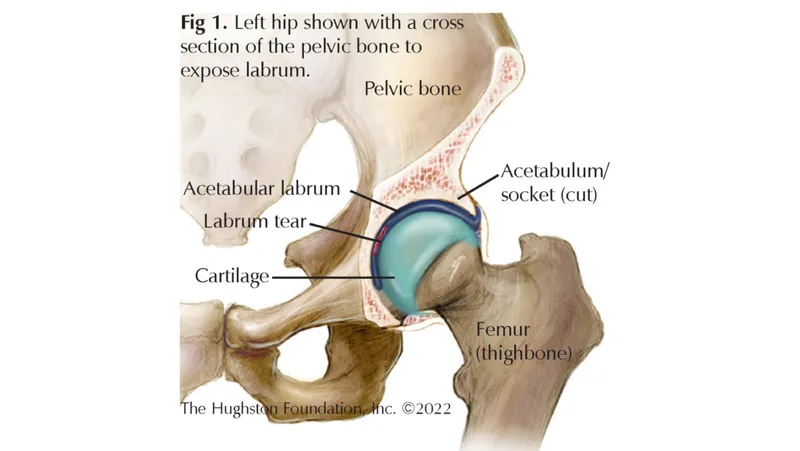
- An **anterior hip dislocation** is caused by forced **abduction** and **external rotation**, putting the **obturator nerve** at risk due to its anatomical course through the **obturator foramen** and proximity to the hip joint.
- Damage to the **obturator nerve** (L2-L4) results in **sensory loss** over the **medial thigh** and paralysis of the **adductor muscles** (adductor longus, brevis, magnus, gracilis), leading to an inability to adduct the thigh.
*Loss of sensation laterally below the knee, weak thigh extension and knee flexion*
- **Sensory loss laterally below the knee** and **weak thigh extension/knee flexion** are characteristic of **sciatic nerve** or common **peroneal nerve injury**, which is more common in **posterior hip dislocations**.
- The presented case describes an **anterior dislocation**, making **obturator nerve** injury more likely than sciatic nerve injury.
*Numbness of the ipsilateral scrotum and upper medial thigh*
- **Numbness of the ipsilateral scrotum** and **upper medial thigh** is associated with injury to the **ilioinguinal nerve** or **genitofemoral nerve**.
- While these nerves supply portions of the **medial thigh** and **genitalia**, they are not typically injured in **anterior hip dislocations** which primarily affect deeper structures like the **obturator nerve**.
*Sensory loss to the dorsal surface of the foot and part of the anterior lower and lateral leg and foot drop*
- **Sensory loss to the dorsal surface of the foot**, **anterior lower and lateral leg**, and **foot drop** are classic signs of **common peroneal nerve** injury due to its superficial course around the fibular head.
- Although the common peroneal nerve is a branch of the **sciatic nerve**, direct injury specifically to the **common peroneal nerve** in an anterior hip dislocation is less probable than obturator nerve injury, and foot drop is characteristic of more severe neural compromise, typically seen in **posterior dislocations or direct trauma**.
*Paresis and numbness of the medial thigh and medial side of the calf, weak hip flexion and knee extension*
- **Paresis and numbness of the medial thigh** are consistent with **obturator nerve** injury. However, **numbness of the medial side of the calf** and **weak hip flexion/knee extension** point towards **femoral nerve** injury.
- While the **femoral nerve** can be injured, the prominent clinical picture of **anterior hip dislocation** points more directly to the **obturator nerve** findings of medial thigh numbness and adduction weakness, rather than primarily femoral nerve symptoms.
Bones and joints of lower limb US Medical PG Question 4: An 80-year-old woman is brought to the emergency department for left hip pain 30 minutes after she fell while walking around in her room. Examination shows left groin tenderness. The range of motion of the left hip is limited because of pain. An x-ray of the hip shows a linear fracture of the left femoral neck with slight posterior displacement of the femur. Which of the following arteries was most likely damaged in the patient's fall?
- A. Superior gluteal artery
- B. Deep circumflex iliac
- C. Deep femoral artery
- D. Obturator
- E. Medial circumflex femoral (Correct Answer)
Bones and joints of lower limb Explanation: ***Medial circumflex femoral***
- This artery is the **primary blood supply** to the femoral head and neck, making it highly vulnerable to injury in cases of femoral neck fractures.
- Damage to the medial circumflex femoral artery significantly increases the risk of **avascular necrosis** of the femoral head.
*Superior gluteal artery*
- The superior gluteal artery primarily supplies the **gluteus medius** and **minimus muscles**.
- It is **not directly involved** in the primary blood supply to the femoral head and neck.
*Deep circumflex iliac*
- This artery mainly supplies the **iliac fossa** and the **abdominal wall muscles**.
- It does not contribute significantly to the blood supply of the femoral neck.
*Deep femoral artery*
- The deep femoral artery, also known as the **profunda femoris artery**, is the main supply to the **thigh muscles**.
- While it gives rise to the circumflex arteries, it is not the artery directly compromised in a femoral neck fracture.
*Obturator*
- The obturator artery primarily supplies the **adductor muscles** of the thigh and contributes a small branch to the femoral head via the **ligamentum teres**.
- This contribution is **insufficient** to maintain viability of the femoral head, especially in trauma to the femoral neck.
Bones and joints of lower limb US Medical PG Question 5: A 24-year-old professional soccer player presents to the clinic with discomfort and pain while walking. He says that he has an unstable knee joint that started after an injury during a match last week. He adds that he heard a popping sound at the time of the injury. Physical examination of the knee reveals swelling of the knee joint with a positive anterior drawer test. Which of the following structures is most likely damaged in this patient?
- A. Lateral collateral ligament
- B. Ligamentum patellae
- C. Anterior cruciate ligament (Correct Answer)
- D. Medial collateral ligament
- E. Posterior cruciate ligament
Bones and joints of lower limb Explanation: ***Anterior cruciate ligament***
- The **"popping sound"** at the time of injury, associated with knee **instability** and a **positive anterior drawer test**, are classic signs of an **ACL tear**.
- The **anterior drawer test** specifically assesses the integrity of the ACL by checking for excessive anterior translation of the tibia relative to the femur.
*Lateral collateral ligament*
- Injury to the LCL typically results from a **varus stress** to the knee and is less commonly associated with a distinct "popping" sound or significant instability.
- While it causes pain and instability, the **anterior drawer test** would likely be negative, and a **varus stress test** would be more indicative.
*Ligamentum patellae*
- Damage to the patellar ligament usually presents as pain and difficulty with knee extension, often following a forceful quadriceps contraction.
- It does not typically cause the described popping sensation or knee instability assessed by the anterior drawer test.
*Medial collateral ligament*
- MCL injuries commonly result from a **valgus stress** (force to the outside of the knee) and are diagnosed with a **valgus stress test**, not the anterior drawer test.
- While it can cause instability, the "popping" sound and specific findings of the anterior drawer test point away from an isolated MCL injury.
*Posterior cruciate ligament*
- A PCL injury is often associated with a **posteriorly directed force** to the tibia, such as a dashboard injury, and would present with a **positive posterior drawer test**.
- The clinical presentation of a **positive anterior drawer test** and significant anterior instability rules out isolated PCL damage.
Bones and joints of lower limb US Medical PG Question 6: A 69-year-old woman presents with pain in her hip and groin. She states that the pain is present in the morning, and by the end of the day it is nearly unbearable. Her past medical history is notable for a treated episode of acute renal failure, diabetes mellitus, obesity, and hypertension. Her current medications include losartan, metformin, insulin, and ibuprofen. The patient recently started taking high doses of vitamin D as she believes that it could help her symptoms. She also states that she recently fell off the treadmill while exercising at the gym. On physical exam you note an obese woman. There is pain, decreased range of motion, and crepitus on physical exam of her right hip. The patient points to the areas that cause her pain stating that it is mostly over the groin. The patient's skin turgor reveals tenting. Radiography is ordered.
Which of the following is most likely to be found on radiography?
- A. Loss of joint space and osteophytes (Correct Answer)
- B. Posterior displacement of the femoral head
- C. Hyperdense foci in the ureters
- D. Femoral neck fracture
- E. Normal radiography
Bones and joints of lower limb Explanation: ***Loss of joint space and osteophytes***
- The patient's presentation with **hip and groin pain worsened by activity**, improved with rest, and associated with **crepitus** and **decreased range of motion**, is highly suggestive of **osteoarthritis**.
- **Osteoarthritis** is characterized radiographically by **loss of joint space**, **osteophytes** (bone spurs), subchondral sclerosis, and subchondral cysts.
*Posterior displacement of the femoral head*
- This finding is characteristic of a **posterior hip dislocation**, which usually presents with severe pain and an inability to bear weight after a significant traumatic event.
- While the patient fell, her symptoms are chronic and progressive, and she has signs of arthritis rather than acute dislocation.
*Hyperdense foci in the ureters*
- These would indicate **kidney stones**, which typically present with acute, severe flank pain radiating to the groin, and hematuria.
- The patient's symptoms are chronic and localized to the hip joint, making kidney stones an unlikely cause of her primary complaint.
*Femoral neck fracture*
- A **femoral neck fracture** would cause acute, severe hip pain, inability to bear weight, and often external rotation and shortening of the leg, usually following a fall.
- Although she fell, her chronic, activity-related pain and crepitus are more indicative of a degenerative process.
*Normal radiography*
- Given the patient's age, chronic and worsening hip pain, physical exam findings of crepitus and decreased range of motion, and risk factors like obesity, it is highly improbable that her hip X-rays would be normal.
- These symptoms are classic for **osteoarthritis**, which shows distinct radiographic changes.
Bones and joints of lower limb US Medical PG Question 7: An MRI of a patient with low back pain reveals compression of the L5 nerve root. Which of the following muscles would most likely show weakness during physical examination?
- A. Tibialis posterior
- B. Tibialis anterior (Correct Answer)
- C. Gastrocnemius
- D. Quadriceps femoris
Bones and joints of lower limb Explanation: ***Tibialis anterior***
- The **L5 nerve root** primarily innervates muscles responsible for **dorsiflexion** of the foot, with the **tibialis anterior** being the primary dorsiflexor.
- Weakness of the tibialis anterior would manifest as difficulty lifting the front of the foot, potentially leading to a **foot drop** gait.
*Tibialis posterior*
- The **tibialis posterior** is primarily innervated by the **tibial nerve** (S1-S2) and is responsible for **plantarflexion** and **inversion** of the foot.
- Weakness in this muscle would not be the most likely presentation of L5 nerve root compression.
*Gastrocnemius*
- The **gastrocnemius** muscle is primarily innervated by the **tibial nerve** (S1-S2) and is a powerful **plantarflexor** of the foot.
- Weakness in this muscle would indicate an S1 or S2 nerve root issue, not typically L5.
*Quadriceps femoris*
- The **quadriceps femoris** is innervated by the **femoral nerve**, predominantly originating from the **L2, L3, and L4 nerve roots**.
- Weakness would manifest as difficulty extending the knee, which is not characteristic of L5 compression.
Bones and joints of lower limb US Medical PG Question 8: A 4-year-old boy is brought to the pediatrician by his mother for a routine medical examination. His medical history is relevant for delayed gross motor milestones. The mother is concerned about a growth delay because both of his brothers were twice his size at this age. Physical examination reveals a well-groomed and healthy boy with a prominent forehead and short stature, in addition to shortened upper and lower extremities with a normal vertebral column. The patient’s vitals reveal: temperature 36.5°C (97.6°F); pulse 60/min; and respiratory rate 17/min and a normal intelligence quotient (IQ). A mutation in which of the following genes is the most likely cause underlying the patient’s condition?
- A. Runt-related transcription factor 2
- B. Alpha-1 type I collagen
- C. Fibroblast growth factor receptor 3 (Correct Answer)
- D. Insulin-like growth factor 1 receptor
- E. Fibrillin-1
Bones and joints of lower limb Explanation: ***Fibroblast growth factor receptor 3***
- The constellation of **short stature**, prominent forehead, and **shortened upper and lower extremities** with a normal vertebral column in a child with normal intelligence is characteristic of **achondroplasia**.
- Achondroplasia is caused by a gain-of-function mutation in the **fibroblast growth factor receptor 3 (FGFR3)** gene, which inhibits chondrocyte proliferation and differentiation, leading to impaired endochondral ossification.
*Runt-related transcription factor 2*
- Mutations in **Runt-related transcription factor 2 (RUNX2)** are associated with **cleidocranial dysplasia**, a condition characterized by absent or hypoplastic clavicles, delayed closure of fontanelles, and dental abnormalities, which are not described in this patient.
- While it affects bone development, the specific features of achondroplasia, such as rhizomelic dwarfism and a prominent forehead, are not typical of RUNX2 mutations.
*Alpha-1 type I collagen*
- Mutations in **collagen genes**, particularly type I collagen (COL1A1, COL1A2), are linked to **osteogenesis imperfecta**, characterized by **fragile bones**, blue sclera, and hearing loss.
- The patient's presentation does not include these features, and the primary issue is disproportionate short stature due to impaired cartilage growth, not bone fragility.
*Insulin-like growth factor 1 receptor*
- Mutations in the **insulin-like growth factor 1 receptor (IGF1R)** can lead to **pre- and postnatal growth retardation** and microcephaly, often associated with developmental delay and feeding difficulties.
- While IGF1R mutations cause short stature, the specific skeletal dysmorphology (e.g., prominent forehead, shortened limbs) and normal intelligence are much more suggestive of achondroplasia.
*Fibrillin-1*
- Mutations in **fibrillin-1** are responsible for **Marfan syndrome**, which typically presents with **tall stature**, long limbs (dolichostenomelia), joint hypermobility, and cardiovascular abnormalities such as aortic root dilation.
- The patient's short stature and shortened limbs directly contradict the clinical picture of Marfan syndrome.
Bones and joints of lower limb US Medical PG Question 9: A 43-year-old man comes to the physician because of a swelling at the back of his left knee that he first noticed 2 months ago. The swelling is not painful, but he occasionally experiences pain at the back of his knee when he is standing for prolonged periods. He also reports mild stiffness of the knee when he wakes up in the morning that disappears after a few minutes of waking up and moving about. Examination shows no local calf tenderness, but forced dorsiflexion of the foot aggravates his knee pain. There is a 3-cm, mildly tender, fixed mass at the medial side of the left popliteal fossa. The mass is more prominent on extension and disappears upon flexion of the left knee. Which of the following is the strongest predisposing risk factor for this patient's condition?
- A. Family history of multiple lipomatosis
- B. History of meniscal tear (Correct Answer)
- C. Purine-rich diet
- D. Mutation of coagulation factor V gene
- E. Varicose veins
Bones and joints of lower limb Explanation: ***History of meniscal tear***
- The patient's presentation with a **non-painful popliteal swelling**, morning stiffness, and pain with prolonged standing is highly suggestive of a **Baker's cyst**.
- A Baker's cyst, also known as a popliteal cyst, is typically a secondary condition arising from underlying knee joint pathology, with a **meniscal tear** being a very common predisposing factor due to increased intra-articular pressure and fluid accumulation.
*Family history of multiple lipomatosis*
- **Lipomatosis** involves the presence of multiple benign fatty tumors (**lipomas**) and is not directly related to the formation of a Baker's cyst, which is a fluid-filled sac.
- While lipomas can occur, they do not cause the specific symptoms of knee stiffness, pain with prolonged standing, or the characteristic changes in prominence with knee flexion/extension seen in this case.
*Purine-rich diet*
- A **purine-rich diet** is a risk factor for **gout**, a form of inflammatory arthritis caused by uric acid crystal deposition.
- Gout typically presents with acute, painful joint inflammation and swelling, which is distinct from the described painless popliteal swelling and mild stiffness.
*Mutation of coagulation factor V gene*
- A mutation in the **coagulation factor V gene** (e.g., Factor V Leiden) increases the risk of **thrombosis** and **deep vein thrombosis (DVT)**.
- While a DVT can cause calf swelling and pain, the mass described is fixed, more prominent on extension, and disappears on flexion, which is characteristic of a Baker's cyst, not a DVT.
*Varicose veins*
- **Varicose veins** are dilated and tortuous superficial veins, often found in the lower extremities, and are associated with chronic venous insufficiency.
- Varicose veins do not cause the formation of a popliteal cyst or the specific knee mechanical symptoms described; they present as visible dilated veins and leg discomfort, sometimes swelling, but not a distinct fixed mass in the popliteal fossa that changes with knee position.
Bones and joints of lower limb US Medical PG Question 10: A 44-year-old woman comes to the physician for the evaluation of right knee pain for 1 week. The pain began after the patient twisted her knee during basketball practice. At the time of the injury, she felt a popping sensation and her knee became swollen over the next few hours. The pain is exacerbated by walking up or down stairs and worsens throughout the day. She also reports occasional locking of the knee. She has been taking acetaminophen during the past week, but the pain is worse today. Her mother has rheumatoid arthritis. The patient is 155 cm (4 ft 11 in) tall and weighs 75 kg (165 lb); BMI is 33 kg/m2. Vital signs are within normal limits. Examination shows effusion of the right knee; range of motion is limited by pain. There is medial joint line tenderness. Knee extension with rotation results in an audible snap. Further evaluation is most likely to show which of the following?
- A. Hyperintense line in the meniscus on MRI (Correct Answer)
- B. Trabecular loss in the proximal femur on x-ray
- C. Posterior tibial translation on examination
- D. Erosions and synovial hyperplasia on MRI
- E. Anterior tibial translation on examination
Bones and joints of lower limb Explanation: ***Hyperintense line in the meniscus on MRI***
- This patient's symptoms of a **popping sensation**, rapid swelling, pain with stairs, and **locking of the knee** after a twisting injury are highly suggestive of a **meniscal tear**.
- An MRI with a **hyperintense line within the substance of the meniscus extending to the articular surface** is the classic finding for a meniscal tear.
*Trabecular loss in the proximal femur on x-ray*
- **Trabecular loss** in the proximal femur on X-ray is characteristic of **osteoporosis**, a condition affecting bone density.
- While this patient is a woman, there are no other clinical signs pointing to osteoporosis, and it would not explain the acute knee injury symptoms.
*Posterior tibial translation on examination*
- **Posterior tibial translation** on examination (positive posterior drawer test) indicates damage to the **posterior cruciate ligament (PCL)**.
- While a knee injury, the symptoms of initial popping, rapid swelling, and locking are more characteristic of a meniscal tear or ACL injury than an isolated PCL tear.
*Erosions and synovial hyperplasia on MRI*
- **Erosions and synovial hyperplasia** on MRI are classic findings in **inflammatory arthropathies** like **rheumatoid arthritis**, which primarily affect the joint lining (synovium).
- Although the patient's mother has rheumatoid arthritis, there is no indication of chronic inflammatory arthritis, and the patient's acute injury symptoms are not consistent with this.
*Anterior tibial translation on examination*
- **Anterior tibial translation** on examination (positive anterior drawer test or Lachman test) indicates damage to the **anterior cruciate ligament (ACL)**.
- While an ACL injury can cause a pop and swelling, the prominent symptom of **locking** is more specifically associated with meniscal tears where a torn piece of cartilage intermittently blocks joint movement.
More Bones and joints of lower limb US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.