Upper/Lower Limb

On this page
🏗️ The Limb Architecture: Engineering Marvels of Human Movement
Your limbs are precision instruments where bones lever against gravity, muscles fire in coordinated compartments, and nerves orchestrate split-second commands-yet a single injury can unravel this symphony into paralysis, deformity, or chronic pain. This lesson takes you from architectural blueprints through neural wiring to diagnostic pattern recognition, teaching you to decode limb pathology rapidly and manage it with evidence-based precision. You'll master the multi-system thinking that transforms you from observer to strategist, ready to restore function when anatomy fails.
The limbs represent evolutionary masterpieces of mobility versus stability trade-offs. The upper limb prioritizes precision and range, achieving 7 degrees of freedom at the shoulder alone, while the lower limb emphasizes weight-bearing capacity, supporting forces up to 8x body weight during running.
Fundamental Limb Organization
-
Upper Limb Architecture
- Shoulder girdle: 4 joints creating 360-degree mobility
- Arm segment: 1 bone (humerus) with 2 primary joints
- Forearm: 2 bones enabling 180-degree pronation-supination
- Radius: lateral, thumb-side positioning
- Ulna: medial, stable hinge articulation
- Hand: 27 bones in 3 functional units
-
Lower Limb Framework
- Pelvic girdle: 3 fused bones creating stable weight transfer
- Thigh: 1 bone (femur) - longest, strongest in body
- Leg: 2 bones with minimal rotation (45 degrees max)
- Tibia: medial, primary weight-bearing (85% load)
- Fibula: lateral, muscle attachment and 15% load sharing
- Foot: 26 bones in 3 arch systems
📌 Remember: SALT for limb segments - Shoulder/Sacrum, Arm/Anterior thigh, Leg/Lateral leg, Terminal hand/foot. Each segment contains progressively more bones: 1-2-many pattern from proximal to distal.
Neurovascular Territory Mapping
The limbs follow predictable neurovascular highways that determine clinical presentation patterns. Understanding these territories predicts 90% of nerve injury presentations and 95% of vascular compromise patterns.
| Territory | Upper Limb | Lower Limb | Clinical Significance | Injury Pattern |
|---|---|---|---|---|
| Proximal | Axillary vessels/Brachial plexus | Femoral vessels/Lumbar plexus | High-energy trauma | Complete functional loss |
| Mid-shaft | Brachial artery/Radial nerve | Superficial femoral/Sciatic | Fracture association | Specific deficits |
| Distal | Radial/Ulnar arteries | Anterior/Posterior tibial | Compartment risk | Ischemic complications |
| Terminal | Digital vessels/nerves | Plantar vessels/nerves | Precision loss | Functional impairment |
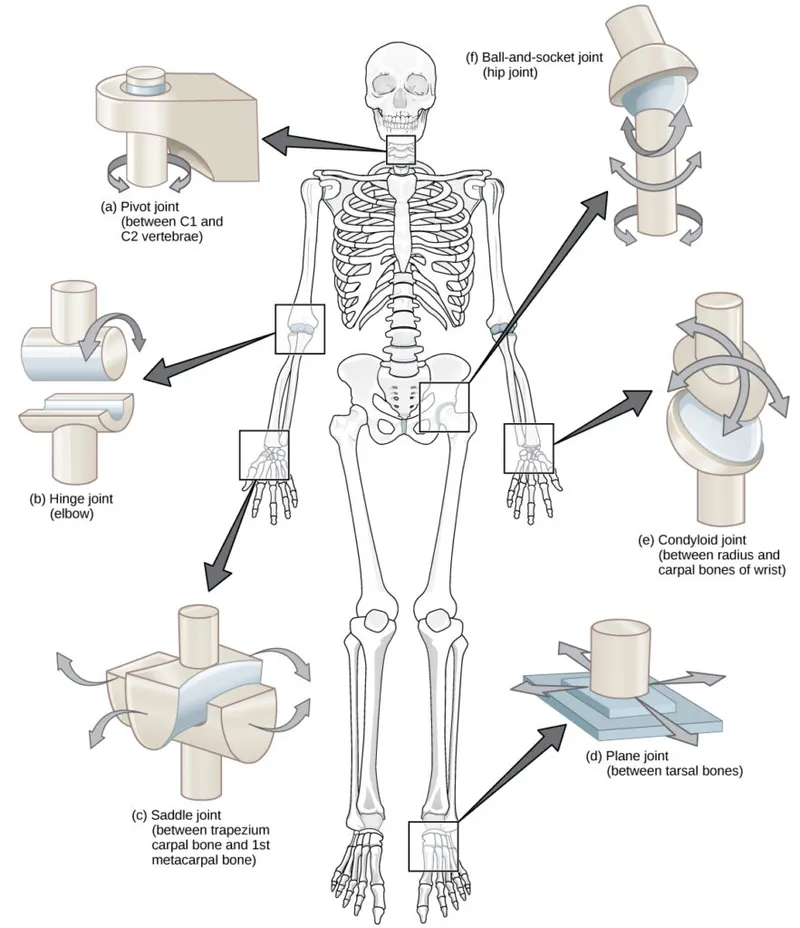
Joint Classification Systems
-
Upper Limb Joint Hierarchy
- Ball-and-socket: Shoulder (3 degrees freedom)
- Hinge: Elbow (1 degree flexion-extension)
- Pivot: Radioulnar (1 degree rotation)
- Superior: 80-degree supination, 85-degree pronation
- Inferior: coupled motion with superior joint
- Condyloid: Wrist (2 degrees flexion-extension, radial-ulnar deviation)
-
Lower Limb Joint Architecture
- Ball-and-socket: Hip (3 degrees but stability-limited)
- Modified hinge: Knee (2 degrees with screw-home mechanism)
- Hinge: Ankle (1 degree dorsi-plantarflexion)
- 20-degree dorsiflexion, 50-degree plantarflexion normal range
- Mortise stability requires intact syndesmosis
💡 Master This: Joint mobility follows the inverse stability rule - greater range of motion correlates with increased injury risk. Shoulder dislocations occur 20x more frequently than hip dislocations due to this mobility-stability trade-off.
The limb architecture establishes the foundation for understanding movement patterns and injury mechanisms. Connect this structural blueprint through functional muscle organization to understand how anatomy enables complex human movement.
🏗️ The Limb Architecture: Engineering Marvels of Human Movement
⚙️ The Movement Engine: Muscle Compartment Dynamics
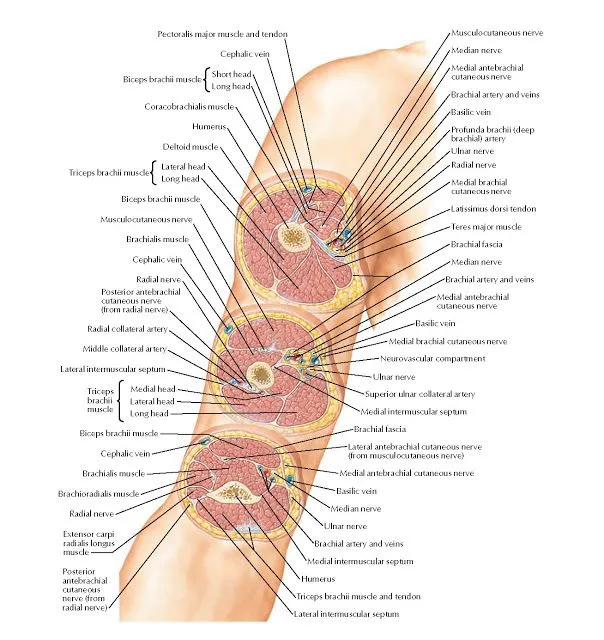
Upper Limb Compartment Architecture
The upper limb organizes into functional motor units that prioritize precision over power, enabling force generation from gram-level fine manipulation to 50+ kilogram lifting capacity.
-
Arm Compartments
- Anterior: Flexor powerhouse (3 muscles)
- Biceps brachii: 2 heads, elbow flexion + supination
- Brachialis: pure flexor, 60% of flexion strength
- Coracobrachialis: shoulder adduction + stabilization
- Posterior: Extensor unit (1 muscle)
- Triceps brachii: 3 heads, primary extensor (85% extension power)
- Long head: shoulder adduction contributor
- Anterior: Flexor powerhouse (3 muscles)
-
Forearm Organization
- Anterior compartments: 2-layer flexor system
- Superficial: 4 muscles - wrist/finger flexion
- Deep: 3 muscles - thumb/index precision control
- Posterior compartments: 2-layer extensor system
- Superficial: 4 muscles - wrist/finger extension
- Deep: 4 muscles - thumb extension + abduction
- Anterior compartments: 2-layer flexor system
📌 Remember: "3-4-4-4" for forearm muscles - 3 deep anterior, 4 superficial anterior, 4 superficial posterior, 4 deep posterior. Total 15 muscles in 4 compartments enable 27-bone hand control.
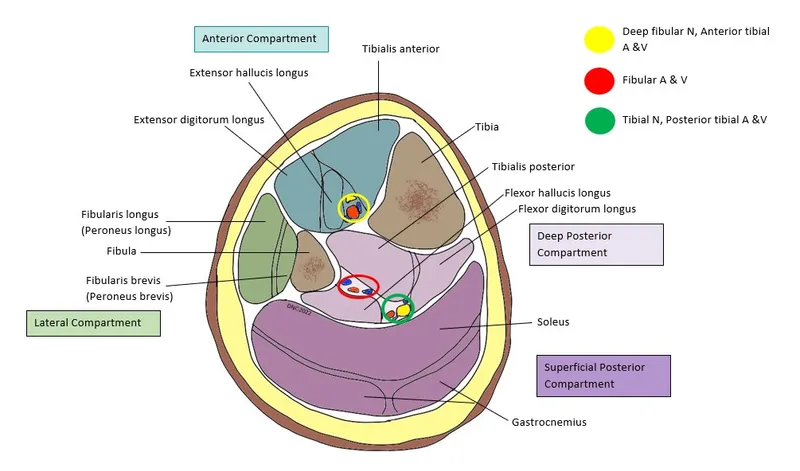
Lower Limb Power Generation
Lower limb compartments prioritize power and stability, generating forces up to 8x body weight during athletic activities while maintaining postural control and locomotion efficiency.
- Thigh Compartment Distribution
- Anterior: Quadriceps complex (4 muscles)
- Rectus femoris: 2-joint muscle (hip flexion + knee extension)
- Vastus group: 3 muscles - pure knee extensors
- Combined force: 3,000+ Newtons extension capability
- Posterior: Hamstring group (3 muscles)
- Biceps femoris: 2 heads - lateral hamstring
- Semimembranosus/Semitendinosus: medial hamstrings
- Dual innervation: tibial + common fibular nerves
- Medial: Adductor complex (5 muscles)
- 3 true adductors + gracilis + obturator externus
- Hip stabilization during single-leg stance
- Anterior: Quadriceps complex (4 muscles)
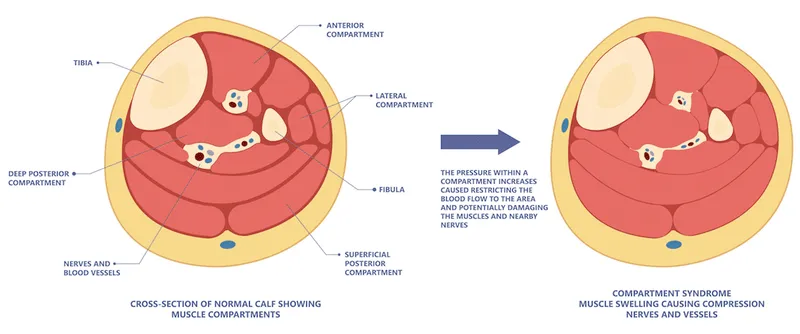
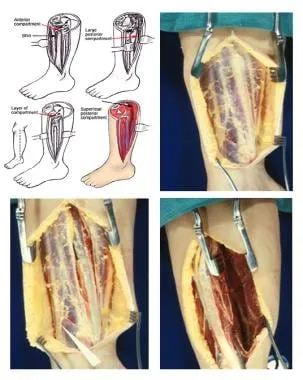
Compartment Syndrome Recognition
| Compartment | Early Signs | Late Signs | Pressure Threshold | Time to Irreversible Damage |
|---|---|---|---|---|
| Forearm Anterior | Finger flexion pain | Volkmann contracture | >30 mmHg | 6-8 hours |
| Leg Anterior | Toe extension weakness | Foot drop | >30 mmHg | 4-6 hours |
| Leg Deep Posterior | Toe flexion pain | Claw toes | >30 mmHg | 6-8 hours |
| Thigh Anterior | Knee extension weakness | Quadriceps fibrosis | >40 mmHg | 8-12 hours |
Muscle Fiber Architecture
-
Power vs. Precision Design
- Pennate muscles: Greater force generation
- Deltoid: multipennate - maximum power at shoulder
- Gastrocnemius: bipennate - explosive plantarflexion
- Parallel muscles: Greater range of motion
- Biceps brachii: long excursion for elbow flexion
- Sartorius: longest muscle - hip/knee flexibility
- Pennate muscles: Greater force generation
-
Fiber Type Distribution
- Type I (slow-twitch): Postural muscles (60-80%)
- Soleus: 90% Type I - endurance standing
- Deep spinal muscles: sustained postural control
- Type II (fast-twitch): Power muscles (60-80%)
- Gastrocnemius: explosive push-off
- Triceps brachii: rapid extension power
- Type I (slow-twitch): Postural muscles (60-80%)
💡 Master This: Muscle architecture determines function - pennate design maximizes force at short ranges, while parallel design optimizes range and speed. This principle explains why deltoid tears cause profound weakness while biceps tears may preserve functional strength.
Understanding compartment organization reveals how muscles coordinate to produce complex movements. Connect this motor framework through nerve control patterns to understand how the nervous system orchestrates limb function.
⚙️ The Movement Engine: Muscle Compartment Dynamics
🧠 The Neural Command Center: Limb Innervation Mastery
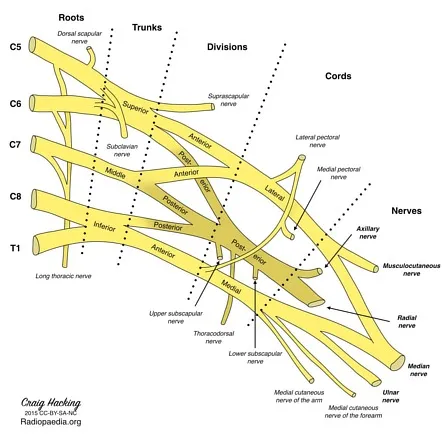
Brachial Plexus: The Upper Limb Command Network
The brachial plexus transforms 5 nerve roots (C5-T1) into 5 terminal branches through a systematic reorganization that distributes motor and sensory functions across the entire upper limb.
- Plexus Organization Pattern
- Roots (C5-T1): Spinal nerve origins
- Trunks (3): Superior (C5-C6), Middle (C7), Inferior (C8-T1)
- Divisions (6): Anterior/posterior from each trunk
- Cords (3): Lateral, posterior, medial (named by axillary artery relationship)
- Branches (5): Terminal nerves to limb regions
📌 Remember: "Real Truckers Drink Cold Beer" for plexus organization - Roots, Trunks, Divisions, Cords, Branches. Each level has specific injury patterns and predictable deficits.
Terminal Nerve Distribution Patterns
| Terminal Nerve | Motor Territory | Sensory Territory | Key Clinical Test | Injury Mechanism |
|---|---|---|---|---|
| Musculocutaneous | Biceps, brachialis | Lateral forearm | Elbow flexion strength | Shoulder dislocation |
| Axillary | Deltoid, teres minor | Shoulder badge area | Arm abduction | Humeral neck fracture |
| Radial | Triceps, extensors | First web space | Wrist extension | Humeral shaft fracture |
| Median | Thenar muscles | Thumb, index, middle | Thumb opposition | Carpal tunnel |
| Ulnar | Hypothenar, interossei | Ring, little finger | Finger abduction | Elbow trauma |
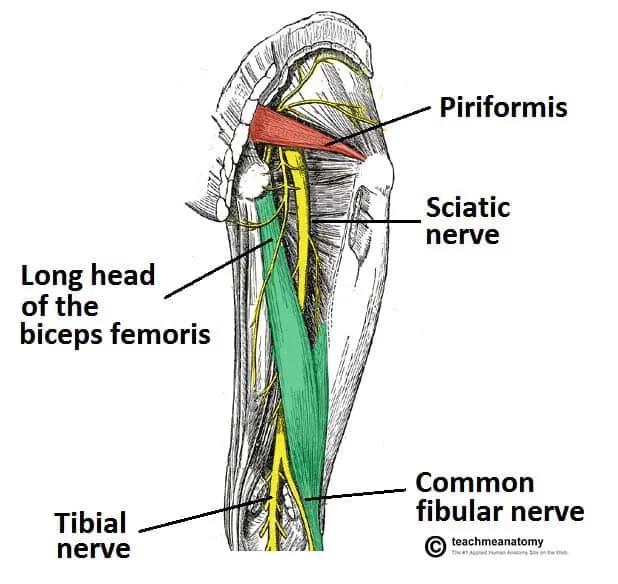
Lower Limb Neural Architecture
The lower limb receives innervation from 2 major plexuses - lumbar (L1-L4) and sacral (L4-S3) - creating overlapping territories that provide redundancy for critical functions like weight-bearing and locomotion.
-
Lumbar Plexus Derivatives
- Femoral nerve (L2-L4): Quadriceps power + anterior thigh sensation
- Obturator nerve (L2-L4): Adductor strength + medial thigh sensation
- Lateral femoral cutaneous (L2-L3): Lateral thigh sensation only
-
Sacral Plexus Organization
- Sciatic nerve (L4-S3): Largest nerve in body (2cm diameter)
- Tibial division: Posterior compartments + plantar foot
- Common fibular division: Lateral/anterior compartments + dorsal foot
- Superior/Inferior gluteal: Hip stabilizer muscles
- Posterior femoral cutaneous: Posterior thigh sensation
- Sciatic nerve (L4-S3): Largest nerve in body (2cm diameter)
Nerve Injury Classification System
-
Seddon Classification (Functional)
- Neurapraxia: Temporary conduction block (days to weeks recovery)
- Axonotmesis: Axon damage, intact sheath (months recovery)
- Neurotmesis: Complete transection (surgical repair required)
-
Sunderland Classification (Anatomical - 5 degrees)
- Grade 1: Myelin damage only (complete recovery)
- Grade 2: Axon + myelin damage (good recovery)
- Grade 3: Endoneurium damage (variable recovery)
- Grade 4: Perineurium damage (poor recovery)
- Grade 5: Complete transection (no recovery without surgery)
💡 Master This: Tinel's sign progression indicates nerve regeneration at 1mm per day (1 inch per month). Advancing tingling sensation confirms axonal regrowth and predicts functional recovery timeline.
Dermatome vs. Peripheral Nerve Patterns
Understanding the difference between dermatome (spinal nerve) and peripheral nerve sensory distributions enables precise localization of neurological lesions.
-
Key Dermatome Landmarks
- C6: Thumb and index finger
- C7: Middle finger (pure C7)
- C8: Ring and little finger
- L4: Medial leg and big toe
- L5: Lateral leg and middle toes
- S1: Lateral foot and little toe
-
Peripheral Nerve Territories
- Median: 3.5 digits (thumb, index, middle, half ring)
- Ulnar: 1.5 digits (little, half ring)
- Radial: First web space (anatomical snuffbox)
- Common fibular: First web space of foot
- Tibial: Plantar surface of foot
Neural command systems establish the foundation for coordinated movement and sensory feedback. Connect this control framework through pattern recognition principles to understand how clinical presentations reveal specific injury locations.
🧠 The Neural Command Center: Limb Innervation Mastery
🔍 The Diagnostic Detective: Pattern Recognition Mastery
Upper Limb Injury Signatures
Each nerve injury creates a unique constellation of findings that enables immediate recognition and accurate prognosis. Understanding these patterns eliminates diagnostic uncertainty and guides appropriate management.
- Radial Nerve Palsy Recognition
- "Saturday Night Palsy" presentation
- Wrist drop: Cannot extend wrist against gravity
- Thumb extension loss: Cannot lift thumb off table
- Finger extension weakness: MCP joints only affected
- Preserved grip strength: Flexors intact
- Sensory loss: First web space only (anatomical snuffbox)
- Spared functions: Triceps (high radial injury) vs preserved (spiral groove)
- "Saturday Night Palsy" presentation
📌 Remember: "WRIST" for radial nerve testing - Wrist extension, Radial deviation, Index finger extension, Snuffbox sensation, Thumb extension. All 5 components must be tested for complete assessment.
Systematic Motor Testing Hierarchy
| Clinical Finding | Primary Nerve | Secondary Considerations | Injury Location | Recovery Prognosis |
|---|---|---|---|---|
| Wrist drop | Radial | C7 radiculopathy | Spiral groove | Good (6-12 weeks) |
| Claw hand | Ulnar | C8-T1 injury | Elbow/wrist | Variable |
| Ape hand | Median | Carpal tunnel | Wrist level | Excellent with surgery |
| Deltoid weakness | Axillary | C5-C6 injury | Quadrilateral space | Good (3-6 months) |
| Biceps weakness | Musculocutaneous | Lateral cord | Coracoid process | Fair |
Lower Limb Diagnostic Patterns
Lower limb nerve injuries follow predictable patterns based on anatomical relationships and common injury mechanisms. Recognition of these patterns enables rapid diagnosis and appropriate referral.
- Sciatic Nerve Injury Spectrum
- Complete sciatic palsy: Devastating functional loss
- Foot drop: Cannot dorsiflex or plantarflex
- Sensory loss: Entire foot except medial border
- Reflex loss: Achilles reflex absent
- Common fibular division (more vulnerable)
- Foot drop: Dorsiflexion weakness
- Steppage gait: High-stepping to clear foot
- Sensory loss: First web space + lateral leg
- Tibial division (less common)
- Plantarflexion weakness: Cannot push off
- Intrinsic foot weakness: Claw toes
- Sensory loss: Plantar surface
- Complete sciatic palsy: Devastating functional loss
Compartment Syndrome Recognition Matrix
-
Early Warning Signs (<6 hours)
- Pain out of proportion: Severe pain with minimal stimulus
- Pain with passive stretch: Most sensitive early sign
- Paresthesias: Nerve compression beginning
- Palpable tension: Compartment firmness
-
Late Findings (>6 hours)
- Pulselessness: Vascular compromise (late sign)
- Paralysis: Motor nerve damage
- Pallor: Ischemic changes
- Poikilothermia: Temperature changes
💡 Master This: Compartment pressure measurement is diagnostic when within 30 mmHg of diastolic pressure. Formula: Perfusion pressure = Diastolic BP - Compartment pressure. <30 mmHg perfusion pressure indicates immediate fasciotomy.
Reflex Testing Interpretation
-
Upper Limb Reflexes
- Biceps (C5-C6): Musculocutaneous nerve
- Brachioradialis (C6): Radial nerve
- Triceps (C7-C8): Radial nerve
-
Lower Limb Reflexes
- Patellar (L3-L4): Femoral nerve
- Achilles (S1-S2): Tibial nerve
-
Pathological Reflexes
- Hoffman sign: Upper motor neuron lesion
- Babinski sign: Corticospinal tract damage
- Clonus: Spasticity indicator
Pattern recognition transforms clinical assessment from random testing to systematic diagnosis. Connect these recognition skills through treatment algorithms to understand how accurate diagnosis guides optimal management decisions.
🔍 The Diagnostic Detective: Pattern Recognition Mastery
⚖️ The Treatment Strategist: Evidence-Based Management Algorithms
Fracture Management Decision Tree
- Open Fracture Classification (Gustilo-Anderson)
- Type I: <1cm wound, minimal contamination (95% union rate)
- Type II: 1-10cm wound, moderate contamination (90% union rate)
- Type IIIA: >10cm wound, adequate soft tissue (85% union rate)
- Type IIIB: Extensive soft tissue loss (75% union rate)
- Type IIIC: Vascular injury requiring repair (65% union rate)
Nerve Injury Treatment Protocols
| Injury Type | Immediate Management | Surgical Timing | Expected Recovery | Rehabilitation Duration |
|---|---|---|---|---|
| Neurapraxia | Observation + splinting | None | Days to weeks | 2-6 weeks |
| Axonotmesis | Splinting + therapy | 3-6 months if no recovery | Months | 6-12 months |
| Neurotmesis | Immediate exploration | Within 72 hours | Limited | 12-24 months |
| Brachial plexus | MRI + EMG | 3-6 months | Variable | 2-5 years |
Compartment Syndrome Management
-
Diagnostic Criteria
- Clinical suspicion + pressure >30 mmHg
- Perfusion pressure <30 mmHg (Diastolic BP - Compartment pressure)
- Pain with passive stretch of compartment muscles
- Progressive neurological deficit
-
Surgical Technique Requirements
- Complete fasciotomy of all compartments
- Skin incisions must be adequate length
- Muscle viability assessment (4 C's: Color, Consistency, Contractility, Circulation)
- Delayed closure at 48-72 hours
💡 Master This: Fasciotomy incisions must decompress all compartments - 2 incisions for leg (4 compartments), 2 incisions for forearm (3 compartments). Inadequate decompression leads to persistent ischemia and poor outcomes.
Rehabilitation Protocols
- Phase-Based Recovery (Evidence-based timelines)
- Phase 1 (0-2 weeks): Protection + pain control
- Immobilization in functional position
- Edema control with elevation + compression
- Pain management with multimodal approach
- Phase 2 (2-6 weeks): Early mobilization
- Passive range of motion to prevent contractures
- Nerve gliding exercises for neural mobility
- Strengthening of unaffected muscles
- Phase 3 (6-12 weeks): Progressive strengthening
- Active range of motion as healing permits
- Resistance training starting at 30% maximum
- Functional activities introduction
- Phase 4 (3-6 months): Return to function
- Sport-specific or work-specific training
- Strength goals: 85% of contralateral limb
- Endurance goals: 90% of pre-injury level
- Phase 1 (0-2 weeks): Protection + pain control
Outcome Prediction Models
-
Upper Limb Functional Scores
- DASH Score: 0-100 scale (<15 = excellent function)
- QuickDASH: 11-item abbreviated version
- Michigan Hand Score: 0-100 scale for hand function
-
Lower Limb Assessment Tools
- Lower Extremity Functional Scale: 0-80 points
- Foot and Ankle Outcome Score: 5 subscales
- Western Ontario McMaster (WOMAC): Hip/knee specific
📌 Remember: "TIME" factors predict outcomes - Tissue quality, Injury mechanism, Medical comorbidities, Early intervention. Optimal outcomes require all 4 factors to be favorable.
Complication Prevention Strategies
-
Infection Prevention (Open injuries)
- Antibiotic prophylaxis within 3 hours
- Tetanus prophylaxis if >5 years since last dose
- Irrigation volume: 9L for Type III open fractures
- Serial debridement until clean margins
-
Thromboembolism Prevention
- Mechanical prophylaxis: Sequential compression devices
- Chemical prophylaxis: LMWH or factor Xa inhibitors
- Duration: 35 days for major lower limb surgery
- Risk stratification: Caprini score >5 = high risk
Treatment algorithms provide systematic approaches to complex clinical decisions. Connect these management principles through integration concepts to understand how multiple systems work together during injury and recovery.
⚖️ The Treatment Strategist: Evidence-Based Management Algorithms
🔗 The Integration Matrix: Multi-System Orchestration
Neuromuscular Integration Dynamics
The limb operates through sophisticated feedback loops that integrate sensory input, motor output, and postural control in real-time, enabling adaptive responses to changing demands.
-
Motor Control Hierarchy
- Spinal level: Reflexes + basic patterns (10-50 ms response)
- Brainstem level: Postural control + balance (50-100 ms)
- Cortical level: Voluntary movement + fine control (100-200 ms)
- Cerebellar modulation: Movement smoothing + error correction
-
Proprioceptive Integration
- Muscle spindles: Length and velocity detection
- Golgi tendon organs: Tension monitoring (protective inhibition)
- Joint mechanoreceptors: Position and movement sensing
- Cutaneous receptors: Touch, pressure, vibration input
📌 Remember: "SPICE" for sensory integration - Spindles (length), Pressure (skin), Inner ear (balance), Cerebellum (coordination), Eyes (visual). All 5 systems contribute to movement control.
Vascular-Lymphatic Coordination
The limb circulation operates as an integrated network where arterial delivery, venous return, and lymphatic drainage coordinate to maintain tissue homeostasis and optimal function.
-
Arterial Supply Redundancy
- Collateral circulation: Multiple pathways for critical regions
- Anastomotic networks: Shoulder (4 arteries), Elbow (8 arteries)
- End-artery territories: Digital vessels - no collaterals
- Autoregulation: Maintains flow across pressure ranges
-
Venous Return Mechanisms
- Muscle pump: Calf muscles generate 60 mmHg pressure
- Valve system: 150+ valves in lower limb prevent reflux
- Respiratory pump: Thoracic pressure changes aid return
- Gravitational effects: Hydrostatic pressure = 90 mmHg when standing
| System Component | Normal Function | Failure Mechanism | Clinical Consequence | Recovery Timeline |
|---|---|---|---|---|
| Arterial | Oxygen delivery | Thrombosis/trauma | Ischemia | Hours to days |
| Venous | Waste removal | Valve failure | Edema/ulceration | Weeks to months |
| Lymphatic | Protein clearance | Node damage | Lymphedema | Months to years |
| Capillary | Nutrient exchange | Inflammation | Tissue dysfunction | Days to weeks |
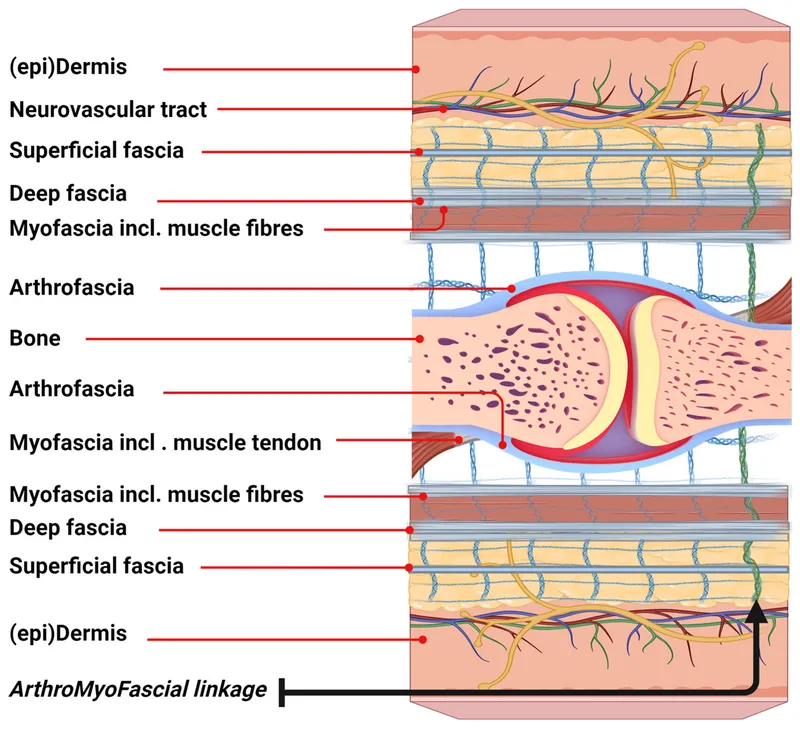
Fascial System Integration
Recent research reveals the fascial system as a continuous network that transmits forces, coordinates movement, and influences proprioception throughout the limb.
-
Fascial Continuity Patterns
- Superficial fascia: Global tension distribution
- Deep fascia: Compartment organization + force transmission
- Intermuscular septa: Load sharing between muscle groups
- Aponeurotic connections: Multi-joint force transfer
-
Clinical Implications
- Myofascial release: Improves mobility by 15-25%
- Scar tissue formation: Disrupts fascial continuity
- Compensation patterns: Remote effects from local injuries
- Movement quality: Fascial health affects coordination
Metabolic Integration During Activity
-
Energy System Coordination
- Phosphocreatine: Immediate energy (0-10 seconds)
- Glycolytic: Short-term power (10 seconds - 2 minutes)
- Oxidative: Sustained activity (>2 minutes)
- System transition: Seamless handoff maintains power output
-
Substrate Utilization
- Rest: 60% fat, 40% carbohydrate
- Moderate exercise: 50% fat, 50% carbohydrate
- High intensity: 5% fat, 95% carbohydrate
- Recovery: Lactate clearance + glycogen resynthesis
💡 Master This: System integration explains why isolated strengthening often fails. Functional rehabilitation must address neuromuscular coordination, fascial mobility, vascular health, and metabolic conditioning simultaneously for optimal outcomes.
Adaptive Response Mechanisms
-
Training Adaptations (Timeline)
- Neural (1-2 weeks): Coordination + recruitment improvements
- Vascular (2-4 weeks): Capillary density + blood flow increases
- Metabolic (4-8 weeks): Enzyme activity + mitochondrial changes
- Structural (8-12 weeks): Muscle hypertrophy + bone remodeling
-
Injury Adaptations
- Acute phase (0-72 hours): Inflammatory response + protection
- Repair phase (3 days - 6 weeks): Tissue regeneration + scar formation
- Remodeling phase (6 weeks - 6 months): Strength restoration + function
- Maturation phase (6 months - 2 years): Tissue optimization
Multi-system integration reveals the complexity underlying simple movements and the interconnected nature of injury and recovery. Connect these integration principles through mastery frameworks to develop comprehensive clinical approaches that address all system components.
🔗 The Integration Matrix: Multi-System Orchestration
🎯 The Clinical Mastery Arsenal: Rapid Assessment Protocols
The 90-Second Limb Screen
- FASTER Protocol for Emergency Assessment
- Function: Can they move it? (5 seconds)
- Appearance: Obvious deformity? (5 seconds)
- Sensation: Can they feel this? (10 seconds)
- Temperature: Warm and pink? (5 seconds)
- Examination: Focused testing (60 seconds)
- Reassessment: Document baseline (5 seconds)
📌 Remember: "FASTER saves limbs" - This 90-second screen identifies 95% of limb-threatening injuries and guides immediate management priorities. Never skip this systematic approach, even in obvious injuries.
Essential Clinical Arsenal
| Assessment Tool | Time Required | Key Findings | Clinical Decision | Sensitivity |
|---|---|---|---|---|
| Pulse check | 10 seconds | Vascular integrity | Surgical emergency? | 98% |
| Two-point discrimination | 15 seconds | Nerve function | Repair needed? | 92% |
| Compartment palpation | 20 seconds | Pressure buildup | Fasciotomy? | 85% |
| Range of motion | 30 seconds | Joint/tendon integrity | Surgical repair? | 90% |
| Strength testing | 45 seconds | Motor nerve function | Nerve injury grade? | 88% |
-
Upper Limb Motor Screen (30 seconds total)
- C5: Shoulder shrug (deltoid/supraspinatus)
- C6: Elbow flexion (biceps)
- C7: Wrist extension (extensor carpi radialis)
- C8: Finger abduction (interossei)
- T1: Thumb pinch (adductor pollicis)
-
Lower Limb Motor Screen (30 seconds total)
- L2: Hip flexion (iliopsoas)
- L3: Knee extension (quadriceps)
- L4: Ankle dorsiflexion (tibialis anterior)
- L5: Great toe extension (extensor hallucis longus)
- S1: Ankle plantarflexion (gastrocnemius)
⭐ Clinical Pearl: The "Rule of 5s" for motor testing - 5 nerve roots, 5 key muscles, 5 seconds each = 25-second complete motor screen. Grade 4/5 or better strength indicates functional preservation.
Critical Numbers Reference
-
Vascular Thresholds
- Ankle-brachial index: >0.9 normal, <0.5 critical ischemia
- Capillary refill: <2 seconds normal, >4 seconds concerning
- Compartment pressure: >30 mmHg abnormal, >40 mmHg surgical
- Perfusion pressure: <30 mmHg indicates fasciotomy
-
Neurological Benchmarks
- Two-point discrimination: <6mm fingertips, <10mm palm
- Monofilament testing: 5.07 (10g) = protective sensation
- Nerve conduction: >40 m/s normal, <30 m/s abnormal
- EMG changes: 3 weeks for denervation potentials
💡 Master This: Document everything with specific numbers and timestamps. "Weak" is not acceptable - use "3/5 strength at 14:30". Precise documentation enables accurate monitoring and medicolegal protection.
Rapid Decision Algorithms
-
Immediate Surgical Indications ("Cannot Wait")
- Open fracture with bone exposure
- Vascular injury with absent pulses
- Compartment syndrome with pressure >40 mmHg
- Complete nerve transection with sharp mechanism
- Mangled extremity with MESS score >7
-
Urgent Referral Criteria ("Same Day")
- Displaced fracture requiring reduction
- Joint dislocation with neurovascular compromise
- Progressive neurological deficit
- Infection with systemic signs
-
Routine Follow-up ("Next Available")
- Non-displaced fractures
- Stable nerve injuries
- Chronic conditions
- Rehabilitation needs
Quality Assurance Checklist
- Before Patient Leaves ("Never Miss")
- Pulses documented (bilateral comparison)
- Sensation mapped (specific dermatomes)
- Motor function graded (0-5 scale)
- Range of motion measured (degrees)
- Pain score recorded (0-10 scale)
- Follow-up arranged (specific timeline)
📌 Remember: "PULSE" for discharge checklist - Pulses present, Understanding confirmed, Limb function documented, Sensation intact, Emergency instructions given. All 5 must be confirmed before patient discharge.
These rapid assessment protocols provide systematic frameworks for efficient, accurate limb evaluation. Master these tools, and you possess the clinical arsenal necessary for expert-level limb assessment in any clinical setting.
🎯 The Clinical Mastery Arsenal: Rapid Assessment Protocols
Practice Questions: Upper/Lower Limb
Test your understanding with these related questions
A 52-year-old man with stage IV melanoma comes to the physician with his wife for a routine follow-up examination. He was recently diagnosed with new bone and brain metastases despite receiving aggressive chemotherapy but has not disclosed this to his wife. He has given verbal consent to discuss his prognosis with his wife and asks the doctor to inform her of his condition because he does not wish to do so himself. She is tearful and has many questions about his condition. Which of the following would be the most appropriate statement by the physician to begin the interview with the patient's wife?









