Thoracic wall and diaphragm US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thoracic wall and diaphragm. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thoracic wall and diaphragm US Medical PG Question 1: A 60-year-old man comes to the clinic complaining of a persistent cough for the last few months. His cough started gradually about a year ago, and it became more severe and persistent despite all his attempts to alleviate it. During the past year, he also noticed some weight loss and a decrease in his appetite. He also complains of progressive shortness of breath. He has a 40-pack-year smoking history but is a nonalcoholic. Physical examination findings are within normal limits. His chest X-ray shows a mass in the right lung. A chest CT shows a 5 cm mass with irregular borders near the lung hilum. A CT guided biopsy is planned. During the procedure, just after insertion of the needle, the patient starts to feel pain in his right shoulder. Which of the following nerves is responsible for his shoulder pain?
- A. Thoracic spinal nerves
- B. Phrenic nerve (Correct Answer)
- C. Vagus nerve
- D. Pulmonary plexus
- E. Intercostal nerves
Thoracic wall and diaphragm Explanation: **Phrenic nerve**
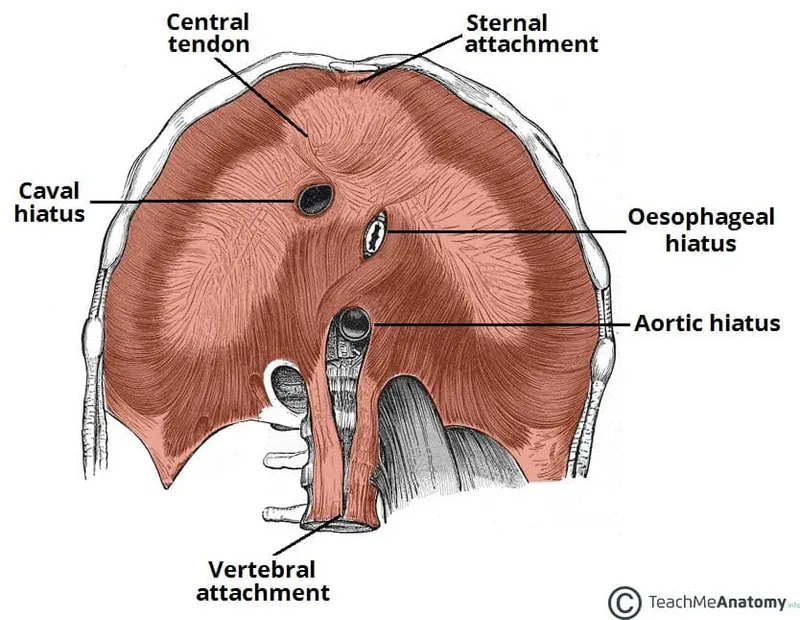
- The **phrenic nerve** innervates the diaphragm and also carries sensory fibers from the **mediastinal and diaphragmatic pleura**, as well as the **pericardium**.
- Irritation of the phrenic nerve, due to its **C3-C5 cervical origin**, can cause **referred pain to the ipsilateral shoulder** or neck.
*Thoracic spinal nerves*
- These nerves primarily serve the **intercostal muscles** and skin of the chest wall.
- While they can transmit pain from the chest wall, they are not typically associated with **referred shoulder pain** from intrathoracic structures.
*Vagus nerve*
- The **vagus nerve** provides parasympathetic innervation to many thoracic and abdominal organs and carries visceral afferents.
- It plays a role in regulating lung function but does not transmit sensory information that would be perceived as **shoulder pain** from diaphragmatic irritation.
*Pulmonary plexus*
- The **pulmonary plexus** is formed by branches of the vagus and sympathetic nerves, primarily involved in regulating **bronchial and vascular tone** in the lungs.
- It does not transmit sensory input that would cause referred pain to the shoulder.
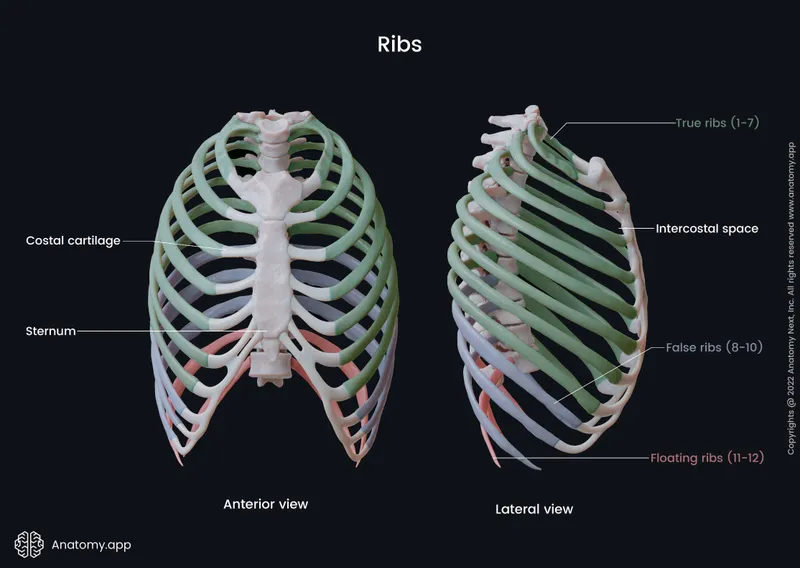
*Intercostal nerves*
- These nerves run along the ribs and innervate the **intercostal muscles** and skin of the **thoracic wall**.
- Pain from these nerves would typically be felt along the **rib cage** or chest wall, not as referred shoulder pain.
Thoracic wall and diaphragm US Medical PG Question 2: A 14-year-old boy is brought to the emergency department because of acute left-sided chest pain and dyspnea following a motor vehicle accident. His pulse is 122/min and blood pressure is 85/45 mm Hg. Physical examination shows distended neck veins and tracheal displacement to the right side. The left chest is hyperresonant to percussion and there are decreased breath sounds. This patient would most benefit from needle insertion at which of the following anatomical sites?
- A. 5th left intercostal space along the midclavicular line
- B. 8th left intercostal space along the posterior axillary line
- C. 2nd left intercostal space along the midclavicular line (Correct Answer)
- D. Subxiphoid space in the left sternocostal margin
- E. 5th left intercostal space along the midaxillary line
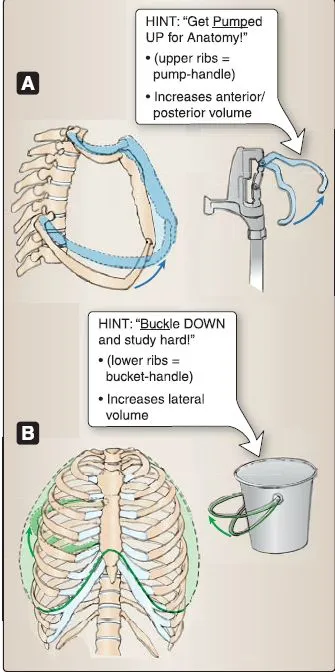
Thoracic wall and diaphragm Explanation: ***2nd left intercostal space along the midclavicular line***
- The patient's symptoms (chest pain, dyspnea, hypotension, distended neck veins, tracheal deviation, hyperresonance, and decreased breath sounds on the left) are classic signs of a **tension pneumothorax**.
- Immediate treatment for **tension pneumothorax** involves needle decompression at the **2nd intercostal space** in the midclavicular line to relieve pressure and restore hemodynamic stability.
*5th left intercostal space along the midclavicular line*
- This location is typically used for **chest tube insertion** in a more controlled setting, not for emergent needle decompression of a tension pneumothorax.
- While it's a safe location for pleural access, it is not the **first-line site** for immediate life-saving decompression.
*8th left intercostal space along the posterior axillary line*
- This site is too low and posterior for effective needle decompression of a tension pneumothorax, which requires rapid access to the **apex of the lung**.
- It is more commonly used for **thoracentesis** to drain fluid from the pleural cavity.
*Subxiphoid space in the left sternocostal margin*
- This location is primarily used for **pericardiocentesis** to drain fluid from the pericardial sac in cases of cardiac tamponade.
- It is not appropriate for addressing a **pneumothorax**, which involves air in the pleural space.
*5th left intercostal space along the midaxillary line*
- This site is a common alternative for **chest tube insertion** but is not the preferred or most immediate site for needle decompression of a tension pneumothorax.
- While it offers pleural access, the **2nd intercostal space** anteriorly is chosen for expediency and safety in an emergency.
Thoracic wall and diaphragm US Medical PG Question 3: A 35-year-old woman volunteers for a study on respiratory physiology. Pressure probes A and B are placed as follows:
Probe A: between the parietal and visceral pleura
Probe B: within the cavity of an alveolus
The probes provide a pressure reading relative to atmospheric pressure. To obtain a baseline reading, she is asked to sit comfortably and breathe normally. Which of the following sets of values will most likely be seen at the end of inspiration?
- A. Probe A: -6 mm Hg; Probe B: 0 mm Hg (Correct Answer)
- B. Probe A: 0 mm Hg; Probe B: -1 mm Hg
- C. Probe A: -4 mm Hg; Probe B: 0 mm Hg
- D. Probe A: -4 mm Hg; Probe B: -1 mm Hg
- E. Probe A: -6 mm Hg; Probe B: -1 mm Hg
Thoracic wall and diaphragm Explanation: ***Probe A: -6 mm Hg; Probe B: 0 mm Hg***
- At the **end of inspiration**, the **intrapleural pressure (Probe A)** is at its most negative, typically around -6 to -8 cm H2O (equivalent to -4 to -6 mmHg), reflecting the maximum expansion of the thoracic cavity.
- At the **end of inspiration**, just before exhalation begins, there is **no airflow**, so the **intrapulmonary pressure (Probe B)** equalizes with atmospheric pressure, resulting in a 0 mm Hg reading.
*Probe A: 0 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of 0 mm Hg** would indicate a **pneumothorax** since it should always be negative to prevent lung collapse.
- An **intrapulmonary pressure of -1 mm Hg** would indicate that **inspiration is still ongoing**, as air would be flowing into the lungs.
*Probe A: -4 mm Hg; Probe B: 0 mm Hg*
- While an **intrapulmonary pressure of 0 mm Hg** is correct at the end of inspiration, an **intrapleural pressure of -4 mm Hg** is typical for the **end of expiration (Functional Residual Capacity)** during quiet breathing, not the end of inspiration.
- The **intrapleural pressure becomes more negative** during inspiration due to increased thoracic volume, so -4 mm Hg would be insufficient.
*Probe A: -4 mm Hg; Probe B: -1 mm Hg*
- An **intrapleural pressure of -4 mm Hg** is the normal pressure at the **end of expiration**, not the end of inspiration, where it becomes more negative.
- An **intrapulmonary pressure of -1 mm Hg** indicates that **inspiration is still in progress**, not at its end, as air would still be flowing into the lungs.
*Probe A: -6 mm Hg; Probe B: -1 mm Hg*
- While an **intrapleural pressure of -6 mm Hg** is consistent with the end of inspiration, an **intrapulmonary pressure of -1 mm Hg** means that **airflow is still occurring into the lungs**.
- At the **very end of inspiration**, just before the start of exhalation, airflow momentarily ceases, and intrapulmonary pressure becomes zero relative to the atmosphere.
Thoracic wall and diaphragm US Medical PG Question 4: A 2-year-old girl is brought to the emergency department by her mother because the girl has had a cough and shortness of breath for the past 2 hours. Her symptoms began shortly after she was left unattended while eating watermelon. She appears anxious and mildly distressed. Examination shows intercostal retractions and unilateral diminished breath sounds with inspiratory wheezing. Flexible bronchoscopy is most likely to show a foreign body in which of the following locations?
- A. Left upper lobe bronchus
- B. Left lower lobe bronchus
- C. Right middle lobe bronchus
- D. Left main bronchus
- E. Right intermediate bronchus (Correct Answer)
Thoracic wall and diaphragm Explanation: ***Right intermediate bronchus***
- Due to the **anatomy of the tracheobronchial tree**, aspirated foreign bodies preferentially enter the **right bronchial tree** because the right main bronchus is wider, shorter, and more vertically oriented than the left.
- In the right bronchial tree, foreign bodies most commonly lodge in the **right lower lobe bronchus or right intermediate bronchus region** (the intermediate bronchus is the segment between the right upper lobe takeoff and the middle/lower lobe bifurcation).
- Among the options provided, the **right intermediate bronchus** is the most anatomically accurate location, as it represents the pathway through which most aspirated foreign bodies travel in the right lung.
- Classic presentation includes sudden onset **cough, shortness of breath, inspiratory wheezing**, and **unilateral diminished breath sounds**.
*Left upper lobe bronchus*
- The **left main bronchus** is narrower and branches at a more acute angle (40-60°) from the trachea compared to the right (20-30°), making aspiration into the left side significantly less common.
- The left upper lobe bronchus branches superiorly and is even less likely to receive aspirated material due to its upward trajectory.
*Left lower lobe bronchus*
- While the **left lower lobe bronchus** is more vertically oriented than the left upper lobe, the entire left bronchial tree receives aspirated foreign bodies much less frequently than the right side.
- If aspiration occurs on the left, this would be the more likely site than the upper lobe, but right-sided aspiration predominates (approximately 60-80% of cases).
*Right middle lobe bronchus*
- The **right middle lobe bronchus** branches anterolaterally from the intermediate bronchus and takes a horizontal course, making it less likely to receive aspirated foreign bodies compared to the more vertical right lower lobe pathway.
- Foreign bodies following gravity tend to bypass this horizontal branch and continue into the lower lobe.
*Left main bronchus*
- While a foreign body could lodge in the **left main bronchus**, this is much less common than right-sided aspiration due to the **more acute angle** (40-60°) at which the left main bronchus branches from the trachea.
- The right main bronchus is the preferential pathway in approximately 60-80% of aspiration cases in young children.
Thoracic wall and diaphragm US Medical PG Question 5: A father brings his 1-year-old son into the pediatrician's office for a routine appointment. He states that his son is well but mentions that he has noticed an intermittent bulge on the right side of his son's groin whenever he cries or strains for bowel movement. Physical exam is unremarkable. The physician suspects a condition that may be caused by incomplete obliteration of the processus vaginalis. Which condition is caused by the same defective process?
- A. Diaphragmatic hernia
- B. Femoral hernia
- C. Testicular torsion
- D. Hydrocele (Correct Answer)
- E. Varicocele
Thoracic wall and diaphragm Explanation: ***Hydrocele***
- The patient's symptoms (intermittent groin bulge with crying/straining) are classic for an **indirect inguinal hernia**, which, like a hydrocele, results from an **incompletely obliterated processus vaginalis**.
- A **hydrocele** involves the accumulation of **serous fluid** within the persistent processus vaginalis, as opposed to abdominal contents in a hernia.
*Diaphragmatic hernia*
- This condition involves the protrusion of abdominal contents into the chest cavity through a defect in the **diaphragm**.
- It is unrelated to the obliteration of the processus vaginalis but rather to **diaphragmatic development**.
*Femoral hernia*
- A femoral hernia involves protrusion through the **femoral canal**, inferior to the inguinal ligament.
- It does not involve the processus vaginalis and is more common in **multiparous women**.
*Testicular torsion*
- This condition is a surgical emergency caused by the **twisting of the spermatic cord**, compromising blood supply to the testis.
- It is not related to the processus vaginalis but often involves an inadequately fixed testis (bell-clapper deformity).
*Varicocele*
- A varicocele is an abnormal dilation of the **pampiniform venous plexus** within the spermatic cord.
- It is caused by incompetent valves in the testicular veins and not by a patent processus vaginalis.
Thoracic wall and diaphragm US Medical PG Question 6: A 21-year-old lacrosse player comes to the doctor for an annual health assessment. She does not smoke or drink alcohol. She is 160 cm (5 ft 3 in) tall and weighs 57 kg (125 lb); BMI is 22 kg/m2. Pulmonary function tests show an FEV1 of 90% and an FVC of 3600 mL. Whole body plethysmography is performed to measure airway resistance. Which of the following structures of the respiratory tree is likely to have the highest contribution to total airway resistance?
- A. Conducting bronchioles
- B. Terminal bronchioles
- C. Segmental bronchi (Correct Answer)
- D. Respiratory bronchioles
- E. Mainstem bronchi
Thoracic wall and diaphragm Explanation: ***Segmental bronchi***
- In healthy individuals, **medium-sized bronchi** (including segmental and subsegmental bronchi, approximately generations 4-8) contribute approximately **80% of total airway resistance**.
- While **Poiseuille's Law** states resistance is inversely proportional to radius to the fourth power (R ∝ 1/r⁴), the key factor is the **total cross-sectional area** and **degree of branching**.
- Medium-sized bronchi have moderate individual resistance and **limited parallel branching**, making them the dominant site of resistance.
- This is why diseases affecting medium-sized airways (e.g., asthma, bronchitis) cause significant increases in airway resistance.
*Terminal bronchioles*
- Although individual terminal bronchioles have small radii and high individual resistance, there are **millions of them arranged in parallel**.
- With parallel resistances, total resistance decreases: 1/R_total = 1/R₁ + 1/R₂ + 1/R₃...
- The **massive number** of small airways means their collective resistance is actually quite **low** (~10-20% of total).
- This is why small airways disease is called the "**silent zone**" - significant pathology can occur before detection.
*Conducting bronchioles*
- These airways also benefit from extensive **parallel branching**, reducing their contribution to total resistance.
- They contribute less than medium-sized bronchi due to their large cumulative cross-sectional area.
*Respiratory bronchioles*
- Part of the **respiratory zone** with the largest total cross-sectional area in the lungs.
- Minimal contribution to airway resistance due to enormous parallel arrangement.
- Primary function is **gas exchange**, not air conduction.
*Mainstem bronchi*
- These large airways have **low individual resistance** due to large diameter.
- Together with the trachea, they contribute approximately **20% of total airway resistance**.
- Not the primary site despite being early in the airway tree.
Thoracic wall and diaphragm US Medical PG Question 7: A 47-year-old woman comes to the emergency department after coughing up 2 cups of bright red blood. A CT angiogram of the chest shows active extravasation from the right bronchial artery. A coil embolization is planned to stop the bleeding. During this procedure, a catheter is first inserted into the right femoral artery. Which of the following represents the correct subsequent order of the catheter route?
- A. Thoracic aorta, right superior epigastric artery, right bronchial artery
- B. Thoracic aorta, right bronchial artery (Correct Answer)
- C. Thoracic aorta, left ventricle, left atrium, pulmonary artery, right bronchial artery
- D. Thoracic aorta, brachiocephalic trunk, right subclavian artery, right internal thoracic artery, right bronchial artery
- E. Thoracic aorta, right subclavian artery, right internal thoracic artery, right bronchial artery
Thoracic wall and diaphragm Explanation: ***Thoracic aorta, right bronchial artery***
- The **femoral artery** leads directly into the **aorta**. From the aorta, the catheter can be navigated to the **thoracic aorta**, where the **bronchial arteries** typically originate.
- The **bronchial arteries** usually arise directly from the **descending thoracic aorta** (most commonly T5-T6 vertebral level) to supply the lung parenchyma and airways.
*Thoracic aorta, right superior epigastric artery, right bronchial artery*
- The **superior epigastric artery** is a terminal branch of the **internal thoracic artery**, supplying the anterior abdominal wall, and is not a direct path to the bronchial arteries.
- Navigating from the superior epigastric artery to the main bronchial artery without passing through intermediary large vessels would be anatomically incorrect and impractical.
*Thoracic aorta, left ventricle, left atrium, pulmonary artery, right bronchial artery*
- This path describes the venous and then pulmonary circulation (right heart, lungs), which is incorrect for reaching the **arterial system** of the bronchial arteries.
- A catheter inserted via the **femoral artery** remains within the arterial system and would not cross into the pulmonary circulation or the left heart chambers in this manner.
*Thoracic aorta, brachiocephalic trunk, right subclavian artery, right internal thoracic artery, right bronchial artery*
- This pathway involves ascending from the **thoracic aorta** to the **brachiocephalic trunk** and subsequently into the **right subclavian** and **internal thoracic arteries**, which is a route primarily to the upper limb and chest wall.
- While the internal thoracic artery can sometimes have small anastomoses, it is not the primary or direct route for embolizing a bronchial artery, which typically originates directly from the descending thoracic aorta.
*Thoracic aorta, right subclavian artery, right internal thoracic artery, right bronchial artery*
- Similar to the previous incorrect option, this route involves navigating through the **subclavian** and **internal thoracic arteries**, which is an indirect and unnecessarily complex path to the bronchial arteries.
- The **bronchial arteries** are direct branches of the **thoracic aorta**, making this a much more convoluted and less likely route for therapeutic embolization.
Thoracic wall and diaphragm US Medical PG Question 8: A 23-year-old man is brought to the emergency department by a coworker for an injury sustained at work. He works in construction and accidentally shot himself in the chest with a nail gun. Physical examination shows a bleeding wound in the left hemithorax at the level of the 4th intercostal space at the midclavicular line. Which of the following structures is most likely injured in this patient?
- A. Right atrium of the heart
- B. Inferior vena cava
- C. Left upper lobe of the lung (Correct Answer)
- D. Left atrium of the heart
- E. Superior vena cava
Thoracic wall and diaphragm Explanation: ***Left upper lobe of the lung***
- The **left upper lobe of the lung** extends to the 4th intercostal space at the midclavicular line, making it the most probable structure to be traversed by a penetrating injury at this location.
- The **pleural cavity** and lung tissue are superficially located in this region, making them highly susceptible to injury from a nail gun.
*Right atrium of the heart*
- The **right atrium** is located predominantly on the right side of the sternum, more centrally, and slightly to the right of the midclavicular line.
- An injury at the **left 4th intercostal space at the midclavicular line** would typically be too lateral and superior to directly injure the right atrium.
*Inferior vena cava*
- The **inferior vena cava (IVC)** enters the right atrium from below, primarily located within the abdomen and passing through the diaphragm at the level of T8.
- Its position is far too **inferior and posterior** relative to the 4th intercostal space to be directly injured by this wound.
*Left atrium of the heart*
- The **left atrium** is the most posterior chamber of the heart and is largely covered by the left ventricle.
- Although part of the heart is on the left, an injury at the **4th intercostal space, midclavicular line**, would likely impact the left ventricle or lung tissue before reaching the left atrium, which is located more posteriorly and medially.
*Superior vena cava*
- The **superior vena cava (SVC)** is located to the right of the midline, formed by the brachiocephalic veins behind the right first costal cartilage.
- Its position is too **medial and superior**, on the right side, to be directly injured by a nail penetrating the left 4th intercostal space at the midclavicular line.
Thoracic wall and diaphragm US Medical PG Question 9: A 28-year-old man comes to the physician because of a 3-month history of pain in his left shoulder. He is physically active and plays baseball twice a week. The pain is reproduced when the shoulder is externally rotated against resistance. Injury of which of the following tendons is most likely in this patient?
- A. Infraspinatus (Correct Answer)
- B. Subscapularis
- C. Pectoralis major
- D. Supraspinatus
- E. Teres major
Thoracic wall and diaphragm Explanation: ***Infraspinatus***
- Pain during **external rotation against resistance** is a classic sign of infraspinatus tendon injury, as it is a primary muscle for this action.
- The patient's history of playing baseball and experiencing pain, especially with resistive external rotation, points to an injury of this **rotator cuff muscle**.
*Subscapularis*
- The subscapularis primarily causes **internal rotation** of the shoulder; injury would typically present with pain during resisted internal rotation, not external.
- While it is a rotator cuff muscle, its function does not align with the specific maneuver causing pain described in the patient.
*Pectoralis major*
- The pectoralis major is a large chest muscle involved primarily in **adduction**, **internal rotation**, and **flexion of the humerus**, not external rotation.
- Injury to this muscle would present with pain during these specific movements, not resisted external rotation.
*Supraspinatus*
- The supraspinatus is primarily involved in **initiation of abduction** and helps stabilize the shoulder joint, and pain would usually be elicited during these movements.
- While a common site of rotator cuff injury, its function does not directly cause pain with resisted external rotation as described.
*Teres major*
- The teres major acts as an **adductor** and **internal rotator** of the humerus, similar to the latissimus dorsi.
- Pain from a teres major injury would be associated with these actions, not with resisted external rotation.
Thoracic wall and diaphragm US Medical PG Question 10: An 18-year-old man is brought to the emergency department 30 minutes after being stabbed in the chest during a fight. He has no other injuries. His pulse is 120/min, blood pressure is 90/60 mm Hg, and respirations are 22/min. Examination shows a 4-cm deep, straight stab wound in the 4th intercostal space 2 cm medial to the right midclavicular line. The knife most likely passed through which of the following structures?
- A. Serratus anterior muscle, pleura, inferior vena cava
- B. External oblique muscle, superior epigastric artery, azygos vein
- C. Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver
- D. Intercostal muscles, internal thoracic artery, right heart
- E. Pectoral fascia, transversus thoracis muscle, right lung (Correct Answer)
Thoracic wall and diaphragm Explanation: ***Pectoral fascia, transversus thoracis muscle, right lung***
* The stab wound is in the **4th intercostal space**, 2 cm medial to the right midclavicular line, placing it over the anterior chest wall. This trajectory would first penetrate the **pectoral fascia**.
* Deeper structures in this region include the **transversus thoracis muscle** and, given the depth, the **right lung** as it extends superiorly behind the anterior chest wall.
* *Serratus anterior muscle, pleura, inferior vena cava*
* The **serratus anterior muscle** is more laterally positioned, typically covering the side of the rib cage.
* The **inferior vena cava** is located more medially and posteriorly within the mediastinum, deep to the diaphragm, making it an unlikely target for an anterior 4th intercostal stab.
* *External oblique muscle, superior epigastric artery, azygos vein*
* The **external oblique muscle** is part of the abdominal wall and would not be penetrated in the 4th intercostal space.
* The **superior epigastric artery** is lower, typically extending into the abdominal wall, and the **azygos vein** is in the posterior mediastinum, not in the path of this superficial anterior stab wound.
* *Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver*
* The **pectoralis minor muscle** is located deep to the pectoralis major, which would be penetrated. However, a stab at the 4th intercostal space would be too high to directly involve the **dome of the diaphragm** or the **right lobe of the liver**, which are typically below the 5th intercostal space, especially in forced expiration.
* *Intercostal muscles, internal thoracic artery, right heart*
* The **intercostal muscles** would certainly be traversed.
* However, the **internal thoracic artery** runs paramedially (about 1-2 cm from the sternum), and getting to the **right heart** would require a more medial and deeper trajectory, potentially causing immediate tamponade or severe hemorrhage.
More Thoracic wall and diaphragm US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.