Pleura and lungs US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pleura and lungs. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pleura and lungs US Medical PG Question 1: A 56-year-old man is brought to the emergency department 30 minutes after falling from a height of 3 feet onto a sharp metal fence pole. He is unconscious. Physical examination shows a wound on the upper margin of the right clavicle in the parasternal line that is 3-cm-deep. Which of the following is the most likely result of this patient's injury?
- A. Rotator cuff tear due to supraspinatus muscle injury
- B. Trapezius muscle paresis due to spinal accessory nerve injury
- C. Traumatic aneurysm due to internal carotid artery injury
- D. Pneumothorax due to pleural injury (Correct Answer)
- E. Hemothorax due to azygos vein injury
Pleura and lungs Explanation: ***Pneumothorax due to pleural injury***
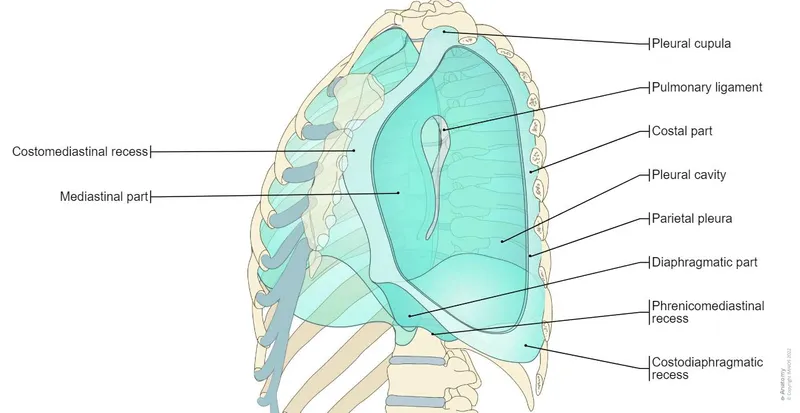
- A 3-cm deep penetrating wound on the upper margin of the **right clavicle** in the parasternal line can easily injure the **pleura** and the **apex of the lung**, which extends above the clavicle.
- Injury to the pleura allows air into the pleural space, leading to a **pneumothorax**, consistent with a patient presenting with an acute injury and unconsciousness.
*Rotator cuff tear due to supraspinatus muscle injury*
- A penetrating injury at the **clavicle** is unlikely to directly injure the **supraspinatus muscle**, which is located more laterally and posteriorly in the shoulder.
- A **rotator cuff tear** would typically result in pain and weakness with arm movement, not immediate unconsciousness.
*Trapezius muscle paresis due to spinal accessory nerve injury*
- The **spinal accessory nerve** (cranial nerve XI) can be injured, especially in the posterior triangle of the neck, leading to **trapezius weakness**.
- However, direct injury to this nerve is less likely from a penetrating wound at the clavicle's **parasternal margin**, and its injury would not lead to sudden unconsciousness.
*Traumatic aneurysm due to internal carotid artery injury*
- The **internal carotid artery** is located deep within the neck, more medially and posteriorly than the described wound location.
- While possible in severe neck trauma, it's less likely to be the primary injury from a clavicular wound and would usually present with signs of significant hemorrhage rather than directly causing unconsciousness without other neurological deficits being mentioned.
*Hemothorax due to azygos vein injury*
- The **azygos vein** is a major vessel located in the posterior mediastinum, deep within the chest, making it highly unlikely to be injured by a 3-cm deep penetrating wound near the **clavicle** unless the injury tract is significantly longer or deviates.
- While a **hemothorax** can occur from vascular injury, a penetrating wound at this location would much more commonly cause a pneumothorax due to the superficial position of the lung apex.
Pleura and lungs US Medical PG Question 2: A 60-year-old man comes to the clinic complaining of a persistent cough for the last few months. His cough started gradually about a year ago, and it became more severe and persistent despite all his attempts to alleviate it. During the past year, he also noticed some weight loss and a decrease in his appetite. He also complains of progressive shortness of breath. He has a 40-pack-year smoking history but is a nonalcoholic. Physical examination findings are within normal limits. His chest X-ray shows a mass in the right lung. A chest CT shows a 5 cm mass with irregular borders near the lung hilum. A CT guided biopsy is planned. During the procedure, just after insertion of the needle, the patient starts to feel pain in his right shoulder. Which of the following nerves is responsible for his shoulder pain?
- A. Thoracic spinal nerves
- B. Phrenic nerve (Correct Answer)
- C. Vagus nerve
- D. Pulmonary plexus
- E. Intercostal nerves
Pleura and lungs Explanation: **Phrenic nerve**
- The **phrenic nerve** innervates the diaphragm and also carries sensory fibers from the **mediastinal and diaphragmatic pleura**, as well as the **pericardium**.
- Irritation of the phrenic nerve, due to its **C3-C5 cervical origin**, can cause **referred pain to the ipsilateral shoulder** or neck.
*Thoracic spinal nerves*
- These nerves primarily serve the **intercostal muscles** and skin of the chest wall.
- While they can transmit pain from the chest wall, they are not typically associated with **referred shoulder pain** from intrathoracic structures.
*Vagus nerve*
- The **vagus nerve** provides parasympathetic innervation to many thoracic and abdominal organs and carries visceral afferents.
- It plays a role in regulating lung function but does not transmit sensory information that would be perceived as **shoulder pain** from diaphragmatic irritation.
*Pulmonary plexus*
- The **pulmonary plexus** is formed by branches of the vagus and sympathetic nerves, primarily involved in regulating **bronchial and vascular tone** in the lungs.
- It does not transmit sensory input that would cause referred pain to the shoulder.
*Intercostal nerves*
- These nerves run along the ribs and innervate the **intercostal muscles** and skin of the **thoracic wall**.
- Pain from these nerves would typically be felt along the **rib cage** or chest wall, not as referred shoulder pain.
Pleura and lungs US Medical PG Question 3: A 27-year-old man presents to the emergency department with severe dyspnea and sharp chest pain that suddenly started an hour ago after he finished exercising. He has a history of asthma as a child, and he achieves good control of his acute attacks with Ventolin. On examination, his right lung field is hyperresonant along with diminished lung sounds. Chest wall motion during respiration is asymmetrical. His blood pressure is 105/67 mm Hg, respirations are 22/min, pulse is 78/min, and temperature is 36.7°C (98.0°F). The patient is supported with oxygen, given corticosteroids, and has had analgesic medications via a nebulizer. Considering the likely condition affecting this patient, what is the best step in management?
- A. CT scan
- B. ABG
- C. Chest X-rays (Correct Answer)
- D. Tube insertion
- E. Sonogram
Pleura and lungs Explanation: ***Chest X-rays***
- The patient's presentation with **sudden onset dyspnea** and **sharp chest pain** post-exercise, along with **hyperresonance** and **diminished lung sounds** in the right lung field, is highly suggestive of a **spontaneous pneumothorax**.
- However, the patient is **hemodynamically stable** (BP 105/67, HR 78/min) with no signs of tension physiology (no severe hypotension, marked tachycardia, or cardiovascular collapse).
- In a stable patient with suspected pneumothorax, **chest X-ray is the appropriate first step** to confirm the diagnosis, determine the size of the pneumothorax, and guide subsequent management (observation for small pneumothorax <20%, aspiration, or tube thoracostomy for larger pneumothoraces).
- Immediate intervention without imaging is reserved for unstable patients with tension pneumothorax.
*Tube insertion*
- Chest tube insertion is the definitive treatment for large pneumothoraces (>20%) or hemodynamically unstable patients with tension pneumothorax.
- In this **stable patient**, proceeding directly to tube insertion without imaging confirmation would be premature and not following standard of care.
- The diagnosis should be confirmed and the size estimated via chest X-ray before determining if tube thoracostomy is necessary.
*CT scan*
- CT scan is not indicated as the initial diagnostic test for suspected pneumothorax.
- It provides more detail than needed for this clinical scenario and causes unnecessary delay and radiation exposure when chest X-ray is sufficient.
- CT may be useful for detecting small pneumothoraces not visible on X-ray or evaluating underlying lung disease, but is not the first-line test.
*ABG*
- An Arterial Blood Gas (ABG) might show hypoxia and respiratory alkalosis, providing information about gas exchange.
- However, ABG does not confirm the diagnosis of pneumothorax or guide immediate management decisions.
- It is an adjunctive test that does not take priority over diagnostic imaging in this scenario.
*Sonogram*
- Lung ultrasound can rapidly detect pneumothorax by showing absent lung sliding and is increasingly used in emergency settings, particularly for bedside evaluation.
- While potentially useful, **chest X-ray remains the standard initial imaging modality** for suspected pneumothorax in most emergency departments, as it provides clear documentation of pneumothorax size and is more universally available and interpreted.
- Ultrasound may be preferred in specific situations (unstable patients, point-of-care evaluation), but chest X-ray is the conventional first-line imaging test.
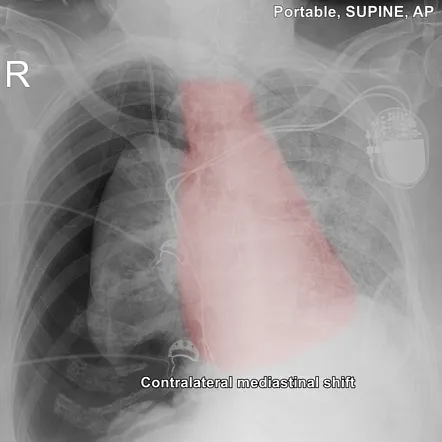
Pleura and lungs US Medical PG Question 4: A 68-year-old male is diagnosed with squamous cell carcinoma in the upper lobe of his right lung. A chest radiograph can be seen in image A. Which of the following would you most expect to find in this patient?
- A. Anisocoria (Correct Answer)
- B. Superior vena cava syndrome
- C. Digital clubbing
- D. Polydipsia
- E. Lateral gaze palsy
Pleura and lungs Explanation: ***Anisocoria***
- A tumor in the **upper lobe of the right lung** (a **Pancoast tumor**) can compress the **sympathetic chain**, leading to **Horner's syndrome**.
- **Horner's syndrome** classically presents with unilateral symptoms on the affected side, including **miosis** (constricted pupil), **ptosis** (drooping eyelid), and **anhydrosis** (decreased sweating), which would cause an apparent **anisocoria** due to the difference in pupil size.
- This is the **most expected finding** for an upper lobe lung tumor due to direct anatomical proximity to the sympathetic chain.
*Superior vena cava syndrome*
- This syndrome is usually caused by tumors in the **upper or middle mediastinum** compressing the **superior vena cava**, leading to facial and upper extremity edema, and distended neck veins.
- While it can occur with lung cancer, a tumor specifically located in the right upper lobe is **less likely** to directly compress the SVC compared to one in the mediastinum.
*Digital clubbing*
- **Digital clubbing** is a common paraneoplastic syndrome associated with various lung diseases, including **lung cancer**, particularly **adenocarcinoma**.
- While possible with squamous cell carcinoma, it is **not location-specific** and can occur with any lung tumor, making it less specific than the neurological findings expected with a Pancoast tumor.
*Polydipsia*
- **Polydipsia** (excessive thirst) can be a symptom of **hypercalcemia**, a paraneoplastic syndrome sometimes associated with **squamous cell carcinoma of the lung** due to the production of **parathyroid hormone-related peptide (PTHrP)**.
- While a possible paraneoplastic syndrome, it is a **metabolic feature** rather than a direct anatomical finding highly specific to an upper lobe tumor compressing local structures.
*Lateral gaze palsy*
- A **lateral gaze palsy** is caused by damage to the **abducens nerve (CN VI)** or its nucleus, leading to an **inability to move the eye laterally**.
- This symptom is **not typically associated** with a primary lung tumor in the upper lobe unless there is widespread metastatic disease affecting the brainstem or cranial nerves, which is not directly indicated.
Pleura and lungs US Medical PG Question 5: A 17-year-old boy is brought to the emergency department by his parents 6 hours after he suddenly began to experience dyspnea and pleuritic chest pain at home. He has a remote history of asthma in childhood but has not required any treatment since the age of four. His temperature is 98.4°F (36.9°C), blood pressure is 100/76 mmHg, pulse is 125/min, respirations are 24/min. On exam, he has decreased lung sounds and hyperresonance in the left upper lung field. A chest radiograph shows a slight tracheal shift to the right. What is the best next step in management?
- A. Needle decompression
- B. CT scan for apical blebs
- C. Observe for another six hours for resolution
- D. Chest tube placement (Correct Answer)
- E. Pleurodesis
Pleura and lungs Explanation: ***Chest tube placement***
- The patient's presentation with **sudden dyspnea**, **pleuritic chest pain**, **decreased lung sounds**, **hyperresonance**, **tachycardia**, and **tracheal shift** indicates a **tension pneumothorax**, which requires immediate **chest tube insertion** for definitive management.
- While the tracheal shift might suggest tension pneumothorax, the patient's relative **hemodynamic stability** (BP 100/76, pulse 125/min) and the fact that he was stable for 6 hours implies it's a large **primary spontaneous pneumothorax** rather than an emergent tension pneumothorax. A chest tube is the appropriate next step for symptomatic patients with a large pneumothorax.
*Needle decompression*
- This procedure is reserved for true **tension pneumothorax** where there is imminent **hemodynamic compromise** (e.g., hypotension, severe tachycardia, hypoxemia) due to severe intrathoracic pressure buildup.
- The patient's blood pressure is stable, indicating that while there is a significant pneumothorax, it's not immediately life-threatening enough to warrant needle decompression before chest tube placement.
*CT scan for apical blebs*
- A **CT scan** might be useful for identifying the cause of the pneumothorax, such as **apical blebs**, but it's not an immediate management step for an acute, symptomatic pneumothorax.
- Prioritizing definitive treatment to reinflate the lung and relieve symptoms is crucial before investigating the underlying cause.
*Observe for another six hours for resolution*
- Observation is only appropriate for **small, asymptomatic pneumothoraces**.
- This patient is symptomatic with significant findings (dyspnea, chest pain, decreased lung sounds, hyperresonance, slight tracheal shift), making observation an unsafe option.
*Pleurodesis*
- **Pleurodesis** is a procedure used to prevent recurrent pneumothoraces and is typically performed after the acute event has been resolved, or for patients with **recurrent pneumothoraces**.
- It is not an acute management step for a new, symptomatic pneumothorax.
Pleura and lungs US Medical PG Question 6: A 15-year-old boy is brought to the emergency department with a 30 minute history of difficulty breathing. He was playing basketball in gym class when he suddenly felt pain in the right side of his chest that got worse when he tried to take a deep breath. Physical exam reveals a tall, thin boy taking rapid shallow breaths. There are decreased breath sounds in the right lung fields and the right chest is hyperresonant to percussion. Which of the following is true of the lesions that would most likely be seen in this patient's lungs?
- A. Found in the lower lobes
- B. Related to liver failure
- C. Found predominantly in the lower lobes
- D. Related to smoking
- E. Found near the pleura (Correct Answer)
Pleura and lungs Explanation: ***Found near the pleura***
- This patient's symptoms (sudden chest pain, difficulty breathing, decreased breath sounds, hyperresonance) are classic for a **spontaneous pneumothorax**.
- In primary spontaneous pneumothorax, the air leak typically results from the rupture of **subpleural blebs** or **bullae**, which are small air-filled sacs located just beneath the visceral pleura at the lung apices.
- This is the key anatomic characteristic of the lesions responsible for this condition.
*Found predominantly in the lower lobes*
- Blebs causing primary spontaneous pneumothorax are typically found in the **apical (upper) regions** of the lung, not the lower lobes.
- The apices experience greater mechanical stress during breathing, making blebs more likely to form and rupture there.
- Lower lobe involvement is not characteristic of primary spontaneous pneumothorax in young, healthy individuals.
*Related to liver failure*
- **Liver failure** is not directly associated with the formation of subpleural blebs or bullae that cause spontaneous pneumothorax.
- Liver failure can cause respiratory issues like **hepatopulmonary syndrome** or **ascites-related diaphragmatic splinting**, but not this specific type of lung lesion.
*Related to smoking*
- Smoking is a significant risk factor for **secondary spontaneous pneumothorax** by causing emphysema and damaging lung parenchyma, leading to bullae formation.
- However, in a **15-year-old boy** with a primary spontaneous pneumothorax, the underlying blebs are often congenital or idiopathic, and smoking is less likely to be the direct cause.
- The key feature is the **subpleural location** of these blebs, typically at the lung apices.
Pleura and lungs US Medical PG Question 7: A 35-year-old male presents to the emergency room with difficulty breathing. He is accompanied by his wife who reports that they were eating peanuts while lying in bed on their backs when he suddenly started coughing profusely. He has a significant cough and has some trouble breathing. His past medical history is notable for obesity, obstructive sleep apnea, seasonal allergies, and alcohol abuse. He uses a continuous positive airway pressure machine nightly. His medications include cetirizine and fish oil. He has a 10 pack-year smoking history. His temperature is 98.6°F (37°C), blood pressure is 125/30 mmHg, pulse is 110/min, and respirations are 23/min. Which of the following lung segments is most likely affected in this patient?
- A. Posterior segment of right superior lobe
- B. Inferior segment of right inferior lobe
- C. Anterior segment of right superior lobe
- D. Inferior segment of left inferior lobe
- E. Superior segment of right inferior lobe (Correct Answer)
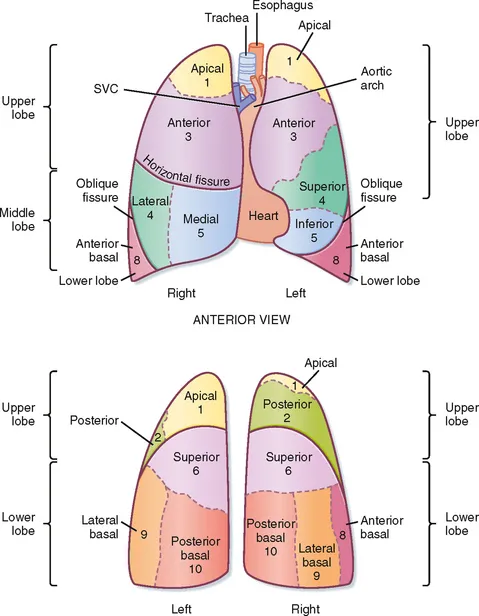
Pleura and lungs Explanation: ***Superior segment of right inferior lobe***
- The patient was found to be lying on his back while eating peanuts, which is a position that predisposes to aspiration into the **superior segment of the right inferior lobe**.
- Aspiration during supine positioning typically leads to foreign body entry into the most posterior-inferiorly directed airways.
*Posterior segment of right superior lobe*
- Aspiration into the **posterior segment of the right superior lobe** is less common in a supine position unless the patient is positioned slightly to the side.
- While the right lung is generally more prone to aspiration due to the straighter main bronchus, the specific segment depends on body position.
*Inferior segment of right inferior lobe*
- The **inferior segment of the right inferior lobe** would be more likely affected if the patient were in an upright position (e.g., sitting or standing) when aspiration occurred.
- In a supine position, gravity directs aspirated material more towards the superior segment of the inferior lobe.
*Anterior segment of right superior lobe*
- Aspiration into the **anterior segment of the right superior lobe** is rare regardless of body position during aspiration.
- This segment is anatomically less susceptible to gravitational flow of aspirated material compared to more posterior or inferior segments.
*Inferior segment of left inferior lobe*
- The **left main bronchus** branches at a sharper angle than the right, making aspiration into the left lung in general less common than into the right lung.
- If aspiration were to occur in the left lung, the specific segment would still largely depend on the patient's body position.
Pleura and lungs US Medical PG Question 8: A 21-year-old lacrosse player comes to the doctor for an annual health assessment. She does not smoke or drink alcohol. She is 160 cm (5 ft 3 in) tall and weighs 57 kg (125 lb); BMI is 22 kg/m2. Pulmonary function tests show an FEV1 of 90% and an FVC of 3600 mL. Whole body plethysmography is performed to measure airway resistance. Which of the following structures of the respiratory tree is likely to have the highest contribution to total airway resistance?
- A. Conducting bronchioles
- B. Terminal bronchioles
- C. Segmental bronchi (Correct Answer)
- D. Respiratory bronchioles
- E. Mainstem bronchi
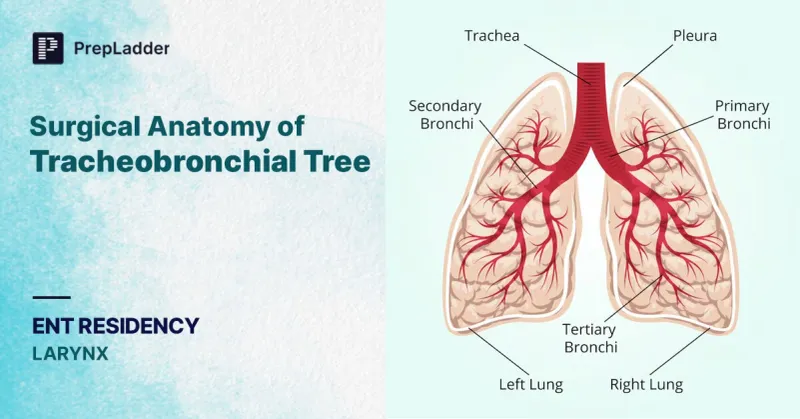
Pleura and lungs Explanation: ***Segmental bronchi***
- In healthy individuals, **medium-sized bronchi** (including segmental and subsegmental bronchi, approximately generations 4-8) contribute approximately **80% of total airway resistance**.
- While **Poiseuille's Law** states resistance is inversely proportional to radius to the fourth power (R ∝ 1/r⁴), the key factor is the **total cross-sectional area** and **degree of branching**.
- Medium-sized bronchi have moderate individual resistance and **limited parallel branching**, making them the dominant site of resistance.
- This is why diseases affecting medium-sized airways (e.g., asthma, bronchitis) cause significant increases in airway resistance.
*Terminal bronchioles*
- Although individual terminal bronchioles have small radii and high individual resistance, there are **millions of them arranged in parallel**.
- With parallel resistances, total resistance decreases: 1/R_total = 1/R₁ + 1/R₂ + 1/R₃...
- The **massive number** of small airways means their collective resistance is actually quite **low** (~10-20% of total).
- This is why small airways disease is called the "**silent zone**" - significant pathology can occur before detection.
*Conducting bronchioles*
- These airways also benefit from extensive **parallel branching**, reducing their contribution to total resistance.
- They contribute less than medium-sized bronchi due to their large cumulative cross-sectional area.
*Respiratory bronchioles*
- Part of the **respiratory zone** with the largest total cross-sectional area in the lungs.
- Minimal contribution to airway resistance due to enormous parallel arrangement.
- Primary function is **gas exchange**, not air conduction.
*Mainstem bronchi*
- These large airways have **low individual resistance** due to large diameter.
- Together with the trachea, they contribute approximately **20% of total airway resistance**.
- Not the primary site despite being early in the airway tree.
Pleura and lungs US Medical PG Question 9: An 18-year-old man is brought to the emergency department 30 minutes after being stabbed in the chest during a fight. He has no other injuries. His pulse is 120/min, blood pressure is 90/60 mm Hg, and respirations are 22/min. Examination shows a 4-cm deep, straight stab wound in the 4th intercostal space 2 cm medial to the right midclavicular line. The knife most likely passed through which of the following structures?
- A. Serratus anterior muscle, pleura, inferior vena cava
- B. External oblique muscle, superior epigastric artery, azygos vein
- C. Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver
- D. Intercostal muscles, internal thoracic artery, right heart
- E. Pectoral fascia, transversus thoracis muscle, right lung (Correct Answer)
Pleura and lungs Explanation: ***Pectoral fascia, transversus thoracis muscle, right lung***
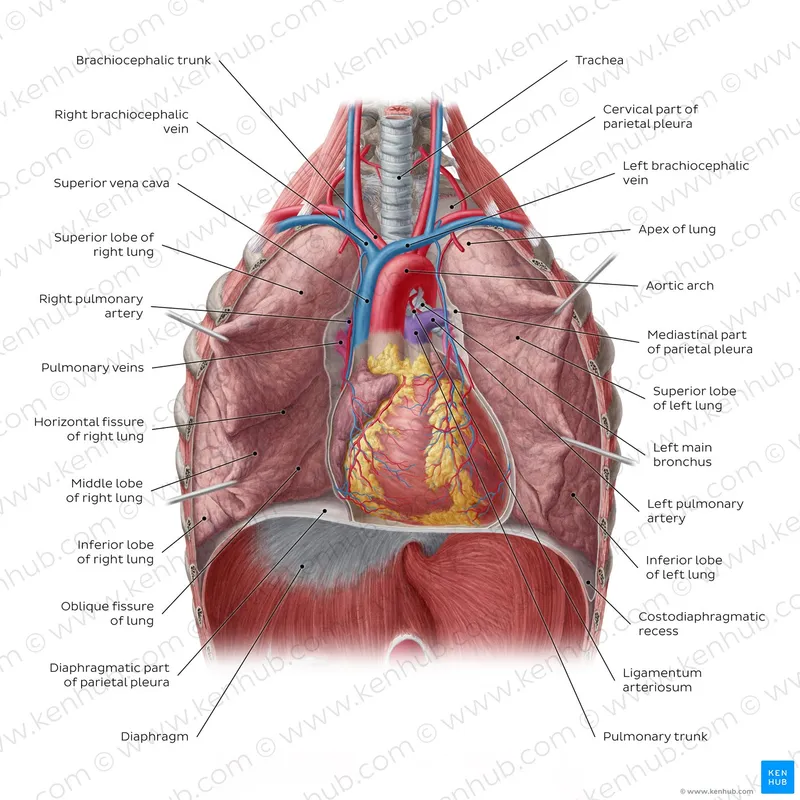
* The stab wound is in the **4th intercostal space**, 2 cm medial to the right midclavicular line, placing it over the anterior chest wall. This trajectory would first penetrate the **pectoral fascia**.
* Deeper structures in this region include the **transversus thoracis muscle** and, given the depth, the **right lung** as it extends superiorly behind the anterior chest wall.
* *Serratus anterior muscle, pleura, inferior vena cava*
* The **serratus anterior muscle** is more laterally positioned, typically covering the side of the rib cage.
* The **inferior vena cava** is located more medially and posteriorly within the mediastinum, deep to the diaphragm, making it an unlikely target for an anterior 4th intercostal stab.
* *External oblique muscle, superior epigastric artery, azygos vein*
* The **external oblique muscle** is part of the abdominal wall and would not be penetrated in the 4th intercostal space.
* The **superior epigastric artery** is lower, typically extending into the abdominal wall, and the **azygos vein** is in the posterior mediastinum, not in the path of this superficial anterior stab wound.
* *Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver*
* The **pectoralis minor muscle** is located deep to the pectoralis major, which would be penetrated. However, a stab at the 4th intercostal space would be too high to directly involve the **dome of the diaphragm** or the **right lobe of the liver**, which are typically below the 5th intercostal space, especially in forced expiration.
* *Intercostal muscles, internal thoracic artery, right heart*
* The **intercostal muscles** would certainly be traversed.
* However, the **internal thoracic artery** runs paramedially (about 1-2 cm from the sternum), and getting to the **right heart** would require a more medial and deeper trajectory, potentially causing immediate tamponade or severe hemorrhage.
Pleura and lungs US Medical PG Question 10: A 23-year-old man is brought to the emergency department by a coworker for an injury sustained at work. He works in construction and accidentally shot himself in the chest with a nail gun. Physical examination shows a bleeding wound in the left hemithorax at the level of the 4th intercostal space at the midclavicular line. Which of the following structures is most likely injured in this patient?
- A. Right atrium of the heart
- B. Inferior vena cava
- C. Left upper lobe of the lung (Correct Answer)
- D. Left atrium of the heart
- E. Superior vena cava
Pleura and lungs Explanation: ***Left upper lobe of the lung***
- The **left upper lobe of the lung** extends to the 4th intercostal space at the midclavicular line, making it the most probable structure to be traversed by a penetrating injury at this location.
- The **pleural cavity** and lung tissue are superficially located in this region, making them highly susceptible to injury from a nail gun.
*Right atrium of the heart*
- The **right atrium** is located predominantly on the right side of the sternum, more centrally, and slightly to the right of the midclavicular line.
- An injury at the **left 4th intercostal space at the midclavicular line** would typically be too lateral and superior to directly injure the right atrium.
*Inferior vena cava*
- The **inferior vena cava (IVC)** enters the right atrium from below, primarily located within the abdomen and passing through the diaphragm at the level of T8.
- Its position is far too **inferior and posterior** relative to the 4th intercostal space to be directly injured by this wound.
*Left atrium of the heart*
- The **left atrium** is the most posterior chamber of the heart and is largely covered by the left ventricle.
- Although part of the heart is on the left, an injury at the **4th intercostal space, midclavicular line**, would likely impact the left ventricle or lung tissue before reaching the left atrium, which is located more posteriorly and medially.
*Superior vena cava*
- The **superior vena cava (SVC)** is located to the right of the midline, formed by the brachiocephalic veins behind the right first costal cartilage.
- Its position is too **medial and superior**, on the right side, to be directly injured by a nail penetrating the left 4th intercostal space at the midclavicular line.
More Pleura and lungs US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.