Peritoneum and peritoneal cavity US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Peritoneum and peritoneal cavity. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Peritoneum and peritoneal cavity US Medical PG Question 1: A 34-year-old patient presents with severe pain in the right upper quadrant that radiates to the right shoulder. During laparoscopic cholecystectomy, which of the following anatomical spaces must be carefully identified to prevent bile duct injury?
- A. Foramen of Winslow
- B. Lesser sac
- C. Calot's triangle (Correct Answer)
- D. Morrison's pouch
Peritoneum and peritoneal cavity Explanation: ***Calot's triangle***
- **Calot's triangle** is the critical anatomical landmark containing the **cystic artery** and **cystic duct**, whose proper identification is essential to prevent injury to the hepatic artery or bile ducts during cholecystectomy.
- Its boundaries are the **cystic duct** (lateral), the **common hepatic duct** (medial), and the **inferior border of the liver** (superior, sometimes described as the cystic artery).
*Foramen of Winslow*
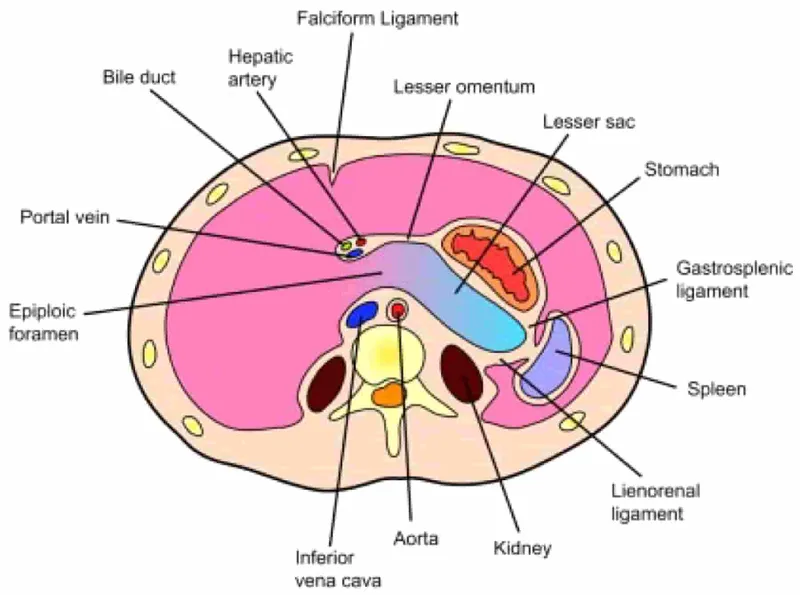
- The **Foramen of Winslow** (epiploic foramen) is an opening connecting the **greater and lesser sacs** of the peritoneal cavity.
- It is not directly relevant to identifying structures during cholecystectomy, but rather to accessing the lesser sac or for surgical procedures involving structures like the portal triad.
*Lesser sac*
- The **lesser sac** (omental bursa) is a peritoneal cavity posterior to the stomach and lesser omentum.
- It is explored in procedures involving the pancreas, posterior gastric wall, or for assessing fluid collections, but not for direct identification of cystic structures during standard cholecystectomy.
*Morrison's pouch*
- **Morrison's pouch** is the **hepatorenal recess**, a potential space between the posterior aspect of the liver and the right kidney and adrenal gland.
- It is a common site for **fluid accumulation** (e.g., ascites, blood) but is not directly incised or dissected for preventing bile duct injury during cholecystectomy.
Peritoneum and peritoneal cavity US Medical PG Question 2: A 12-year-old boy is brought to the emergency department late at night by his worried mother. She says he has not been feeling well since this morning after breakfast. He skipped both lunch and dinner. He complains of abdominal pain as he points towards his lower abdomen but says that the pain initially started at the center of his belly. His mother adds that he vomited once on the way to the hospital. His past medical history is noncontributory and his vaccinations are up to date. His temperature is 38.1°C (100.6°F), pulse is 98/min, respirations are 20/min, and blood pressure is 110/75 mm Hg. Physical examination reveals right lower quadrant tenderness. The patient is prepared for laparoscopic abdominal surgery. Which of the following structures is most likely to aid the surgeons in finding the source of this patient's pain and fever?
- A. McBurney's point
- B. Linea Semilunaris
- C. Transumbilical plane
- D. Arcuate line
- E. Teniae coli (Correct Answer)
Peritoneum and peritoneal cavity Explanation: ***Teniae coli***
- The **teniae coli** are three distinct longitudinal bands of smooth muscle that run along the length of the large intestine, converging at the base of the appendix. They serve as reliable anatomical landmarks for locating the appendix during surgery.
- Given the patient's symptoms (periumbilical pain migrating to the right lower quadrant, fever, vomiting, and right lower quadrant tenderness), **acute appendicitis** is highly suspected, making the teniae coli crucial for surgical identification of the inflamed appendix.
*McBurney's point*
- **McBurney's point** is a clinical landmark on the abdominal wall, two-thirds of the way from the umbilicus to the right anterior superior iliac spine, that often corresponds to the base of the appendix. It is used to elicit tenderness during physical examination.
- While tenderness at McBurney's point is a strong indicator of appendicitis, it is a **surface landmark** for diagnosis and not an internal anatomical structure that aids the surgeon in _finding_ the appendix during a laparoscopic procedure.
*Linea Semilunaris*
- The **linea semilunaris** is the curved tendinous intersection found at the lateral border of the rectus abdominis muscle, extending from the costal margin to the pubic tubercle.
- It defines the lateral extent of the rectus sheath but has **no direct anatomical relationship** to the appendix or its surgical identification.
*Transumbilical plane*
- The **transumbilical plane** is an imaginary horizontal plane passing through the umbilicus. It is used in topographical anatomy for abdominal segmentation.
- It is a **surface and arbitrary anatomical plane** for regional description, not an internal structure that guides surgical access to or identification of the appendix.
*Arcuate line*
- The **arcuate line** is a crescent-shaped anatomical landmark located on the posterior wall of the rectus sheath, inferior to the umbilicus, marking the transition where the aponeuroses of the transverse abdominis and internal oblique muscles pass anterior to the rectus abdominis.
- This line is relevant to the integrity of the rectus sheath but is **anatomically distant from the appendix** and does not assist in its surgical localization.
Peritoneum and peritoneal cavity US Medical PG Question 3: A 2-year-old male is brought to his pediatrician by his mother because of abdominal pain and blood in the stool. Scintigraphy reveals uptake in the right lower quadrant of the abdomen. Persistence of which of the following structures is the most likely cause of this patient's symptoms?
- A. Ureteric bud
- B. Urachus
- C. Paramesonephric duct
- D. Omphalomesenteric duct (Correct Answer)
- E. Allantois
Peritoneum and peritoneal cavity Explanation: ***Omphalomesenteric duct***
- Persistence of the **omphalomesenteric duct** (vitelline duct) can lead to a **Meckel's diverticulum**, which often contains **ectopic gastric or pancreatic tissue**.
- This ectopic tissue can cause **ulceration and bleeding**, leading to abdominal pain and **melena** (blood in stool), and will show uptake on a Technetium-99m pertechnetate scan (scintigraphy) for ectopic gastric mucosa.
*Ureteric bud*
- The ureteric bud forms the **ureter, renal pelvis, calyces**, and **collecting ducts** of the kidney.
- Anomalies of the ureteric bud typically present with **urinary tract issues**, such as hydronephrosis or renal agenesis, not abdominal pain and bloody stools from GI bleeding.
*Urachus*
- The urachus is a remnant of the **allantois** connecting the fetal bladder to the umbilicus.
- Persistent urachal remnants can cause urine leakage from the umbilicus, cysts, or infections, but generally not abdominal pain and bloody stools.
*Paramesonephric duct*
- The paramesonephric (Müllerian) ducts form the **female reproductive organs** (fallopian tubes, uterus, cervix, upper vagina).
- Persistence or anomalies of these ducts are relevant to **gynecological issues** and infertility in females, not the GI symptoms described in a male child.
*Allantois*
- The allantois contributes to the formation of the **urachus** and is involved in early blood formation and bladder development.
- While related to the urachus, its direct persistence or anomalies typically don't cause the specific presentation of abdominal pain and bloody stools due to ectopic gastric mucosa.
Peritoneum and peritoneal cavity US Medical PG Question 4: A child is in the nursery one day after birth. A nurse notices a urine-like discharge being expressed through the umbilical stump. What two structures in the embryo are connected by the structure that failed to obliterate during the embryologic development of this child?
- A. Kidney - large bowel
- B. Liver - umbilical vein
- C. Bladder - small bowel
- D. Pulmonary artery - aorta
- E. Bladder - umbilicus (Correct Answer)
Peritoneum and peritoneal cavity Explanation: ***Bladder - umbilicus***
- A **urine-like discharge** from the umbilical stump indicates a **patent urachus**, which is the embryonic remnant of the allantois.
- The **allantois** (which becomes the urachus) is an embryonic structure that connects the **fetal bladder** to the **umbilicus** during development.
- Normally, the allantois obliterates after birth to form the **median umbilical ligament**, but failure to obliterate results in a patent urachus allowing urine to discharge through the umbilicus.
*Kidney - large bowel*
- These two structures are not directly connected by an obliterating embryonic structure relevant to urine discharge from an umbilical stump.
- The kidneys form urine, and the large bowel is part of the digestive tract, with no direct embryonic communication to the umbilicus for urine expression.
*Liver - umbilical vein*
- The umbilical vein connects the **placenta to the fetal liver** (and ductus venosus) to transport oxygenated blood, not urine.
- Failure of the umbilical vein to obliterate would result in a patent umbilical vein, typically presenting as a vascular anomaly, not urine discharge.
*Pulmonary artery - aorta*
- These structures are connected by the **ductus arteriosus** in fetal circulation, bypassing the pulmonary circulation.
- While important for fetal development, a patent ductus arteriosus (PDA) is a cardiovascular anomaly and would not manifest as urine discharge from the umbilical stump.
*Bladder - small bowel*
- While both structures are involved in waste elimination, there is no normal embryonic structure directly connecting the bladder and small bowel that obliterates to prevent urine discharge from the umbilicus.
- An abnormal connection between the bladder and bowel would typically involve a **fistula** and present with stool in urine or urine in stool, not umbilical discharge.
Peritoneum and peritoneal cavity US Medical PG Question 5: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Peritoneum and peritoneal cavity Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Peritoneum and peritoneal cavity US Medical PG Question 6: A 31-year-old woman presents to the emergency room with high-grade fever and abdominal pain for the past 2 days. She also complains of malaise and has vomited several times since last night. The past medical history is benign. The vital signs include: temperature 40.0°C (104.0°F), pulse 120/min, respiratory rate 28/min, and blood pressure 120/89 mm Hg. On physical examination, severe costovertebral angle tenderness is noted. She is admitted to the medical floor and blood is drawn. The laboratory testing reveals leukocytosis with predominant neutrophilia and increased C-reactive protein and ferritin levels. She is suspected to have a retroperitoneal organ infection. Which of the following best describes the involved organ?
- A. It is the most common site of Meckel's diverticulum.
- B. It is composed of white pulp and red pulp.
- C. It is composed of tubules and parenchyma. (Correct Answer)
- D. It stores and concentrates bile.
- E. It produces hydrochloric acid.
Peritoneum and peritoneal cavity Explanation: ***It is composed of tubules and parenchyma.***
- The patient's symptoms of **high-grade fever**, **abdominal pain**, and **costovertebral angle (CVA) tenderness** are highly suggestive of **pyelonephritis**, an infection of the kidney.
- The **kidney** is a retroperitoneal organ composed of millions of **nephrons**, which include **renal tubules** and surrounding **parenchyma**.
*It is the most common site of Meckel's diverticulum.*
- **Meckel's diverticulum** is a remnant of the vitelline duct and is typically found in the **ileum** (small intestine), an intraperitoneal organ, not a retroperitoneal one.
- Its presence is not associated with costovertebral angle tenderness or the described systemic symptoms.
*It is composed of white pulp and red pulp.*
- The **spleen** is composed of white pulp (lymphoid tissue) and red pulp (vascular sinuses), but it is an **intraperitoneal organ** and its infection typically does not present with costovertebral angle tenderness.
- Splenic infection (e.g., abscess) is less common and usually presents with left upper quadrant pain, not the retroperitoneal symptoms described.
*It stores and concentrates bile.*
- The **gallbladder** stores and concentrates bile, and while it is partially retroperitoneal or intraperitoneal depending on its location, an infection (cholecystitis) typically causes right upper quadrant pain, not costovertebral angle tenderness.
- Its function is unrelated to the described symptoms of a kidney infection.
*It produces hydrochloric acid.*
- The **stomach** produces hydrochloric acid, but it is an **intraperitoneal organ**, and its infection or inflammation (gastritis, peptic ulcer) would cause epigastric pain, not costovertebral angle tenderness.
- The clinical picture does not align with symptoms related to the stomach.
Peritoneum and peritoneal cavity US Medical PG Question 7: What is the most common site of congenital diaphragmatic hernia?
- A. Central tendon
- B. Posterolateral (Correct Answer)
- C. Crural
- D. Anterolateral
- E. Esophageal hiatus
Peritoneum and peritoneal cavity Explanation: ***Posterolateral***
- The **posterolateral** region, specifically the foramen of Bochdalek, is the most common site for congenital diaphragmatic hernia (CDH).
- This type of hernia accounts for approximately 80-90% of all CDH cases and usually occurs on the **left side**.
*Central tendon*
- Hernias through the **central tendon** are extremely rare and are distinct from the more common forms of CDH.
- Defects in the central tendon are often associated with **pericardial defects** rather than typical diaphragmatic hernias which allow abdominal contents into the thoracic cavity.
*Crural*
- Hernias involving the **crura** of the diaphragm are typically **hiatal hernias** (e.g., sliding or paraesophageal), which are different in origin and presentation from CDH.
- These are usually acquired and involve the stomach moving into the mediastinum, rather than a congenital defect leading to abdominal viscera migrating into the chest.
*Anterolateral*
- While congenital diaphragmatic hernias can occur **anterolaterally** through the foramen of Morgagni, these are much less common than posterolateral hernias.
- Morgagni hernias account for a small percentage of CDH cases (around 2-5%) and are typically located on the right side, often containing omentum or colon.
*Esophageal hiatus*
- The **esophageal hiatus** is the normal opening in the diaphragm through which the esophagus passes.
- While hiatal hernias can occur at this site, these are typically **acquired hernias** in adults, not congenital diaphragmatic hernias.
- Congenital CDH refers to developmental defects in the diaphragm itself, not enlargement of normal openings.
Peritoneum and peritoneal cavity US Medical PG Question 8: Identify the labeling correctly

- A. A - Ascending aorta, B - Pulmonary trunk, C - Superior vena cava, D - Descending aorta (Correct Answer)
- B. A - Ascending aorta, B - Superior vena cava, C - Pulmonary trunk, D - Descending aorta
- C. A - Superior vena cava, B - Pulmonary trunk, C - Ascending aorta, D - Descending aorta
- D. A - Pulmonary trunk, B - Ascending aorta, C - Superior vena cava, D - Descending aorta
- E. A - Ascending aorta, B - Pulmonary trunk, C - Descending aorta, D - Superior vena cava
Peritoneum and peritoneal cavity Explanation: ***A - Ascending aorta, B - Pulmonary trunk, C - Superior vena cava, D - Descending aorta***
- **A** points to the **ascending aorta**, the initial segment of the aorta emerging from the left ventricle.
- **B** indicates the **pulmonary trunk**, which originates from the right ventricle and carries deoxygenated blood to the lungs.
- **C** correctly identifies the **superior vena cava**, responsible for draining deoxygenated blood from the upper body into the right atrium.
- **D** is correctly labeled as the **descending aorta**, the portion of the aorta that descends through the thorax and abdomen.
*A - Ascending aorta, B - Superior vena cava, C - Pulmonary trunk, D - Descending aorta*
- This option incorrectly identifies **B as superior vena cava** and **C as pulmonary trunk**. B is clearly emerging from the right ventricle, characteristic of the pulmonary trunk, while C is positioned where the superior vena cava would be.
- The superior vena cava (C) would be located to the right and anterior to the ascending aorta, while the pulmonary trunk (B) is anterior to the ascending aorta, emerging from the right ventricle.
*A - Superior vena cava, B - Pulmonary trunk, C - Ascending aorta, D - Descending aorta*
- This option incorrectly labels **A as superior vena cava** and **C as ascending aorta**. A is clearly the large vessel emerging from the left side of the heart, consistent with the ascending aorta.
- The ascending aorta (A) would be the largest vessel emerging from the left ventricle, and the superior vena cava (C) would be entering the right atrium.
*A - Pulmonary trunk, B - Ascending aorta, C - Superior vena cava, D - Descending aorta*
- This option incorrectly identifies **A as pulmonary trunk** and **B as ascending aorta**. A is the large vessel originating from the left ventricle, which is the ascending aorta.
- The pulmonary trunk (B) arises from the right ventricle and is usually anterior to the ascending aorta (A).
*A - Ascending aorta, B - Pulmonary trunk, C - Descending aorta, D - Superior vena cava*
- This option incorrectly swaps **C and D**, labeling C as descending aorta and D as superior vena cava. C is positioned in the superior mediastinum where the superior vena cava enters the right atrium, not in the posterior mediastinum where the descending aorta would be located.
- The descending aorta (D) runs posteriorly in the thorax, while the superior vena cava (C) is an anterior structure draining into the right atrium.
Peritoneum and peritoneal cavity US Medical PG Question 9: Structure preventing vertical descent of spleen
- A. Ligamentum teres
- B. Ligamentum flavum
- C. Hepatogastric ligament
- D. Phrenocolic ligament (Correct Answer)
- E. Lienorenal ligament
Peritoneum and peritoneal cavity Explanation: ***Phrenocolic ligament***
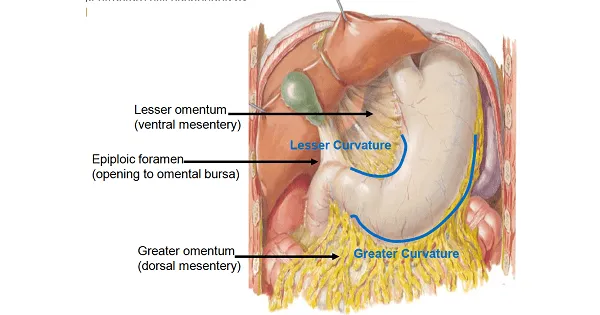
- The **phrenocolic ligament** is a fold of peritoneum that extends from the left colic (splenic) flexure of the colon to the diaphragm.
- It forms a shelf or sling underneath the spleen, providing crucial support and preventing its **vertical descent**.
*Ligamentum teres*
- The **ligamentum teres hepatis** is the remnant of the obliterated umbilical vein, found in the free margin of the falciform ligament.
- It connects the umbilicus to the liver and plays no role in supporting the spleen.
*Ligamentum flavum*
- The **ligamentum flavum** is a series of elastic ligaments connecting the laminae of adjacent vertebrae in the spinal column.
- It is a component of the vertebral column and has no anatomical or functional relationship with the spleen.
*Hepatogastric ligament*
- The **hepatogastric ligament** is part of the lesser omentum, extending from the liver to the lesser curvature of the stomach.
- Its primary function is to contain the **gastric arteries** and connect these organs, not to support the spleen.
*Lienorenal ligament*
- The **lienorenal ligament** (splenorenal ligament) connects the hilum of the spleen to the anterior surface of the left kidney.
- While it provides **lateral support** to the spleen, it does not prevent **vertical descent** as effectively as the phrenocolic ligament.
Peritoneum and peritoneal cavity US Medical PG Question 10: A 46-year-old male presents in consultation for weight loss surgery. He is 6’0” and weighs 300 pounds. He has tried multiple dietary and exercise regimens but has been unsuccessful in losing weight. The surgeon suggests a sleeve gastrectomy, a procedure that reduces the size of the stomach removing a large portion of the stomach along the middle part of the greater curvature. The surgeon anticipates having to ligate a portion of the arterial supply to this part of the stomach in order to complete the resection. Which of the following vessels gives rise to the vessel that will need to be ligated in order to complete the resection?
- A. Right gastroepiploic artery
- B. Splenic artery (Correct Answer)
- C. Left gastric artery
- D. Gastroduodenal artery
- E. Right gastric artery
Peritoneum and peritoneal cavity Explanation: ***Splenic artery***
- A sleeve gastrectomy involves resecting a large portion of the **greater curvature of the stomach**. This portion is primarily supplied by the **short gastric arteries** and the **left gastroepiploic artery**.
- The **splenic artery** is the main vessel that gives rise to the **short gastric arteries** and the **left gastroepiploic artery**, which originate from the distal portion of the splenic artery prior to its terminal branches. Therefore, ligation of branches from the splenic artery would be necessary.
*Right gastroepiploic artery*
- The **right gastroepiploic artery** primarily supplies the distal part of the greater curvature and arises from the **gastroduodenal artery**.
- While it contributes to the vascular supply of the greater curvature, the bulk of the vessels needing ligation for a *sleeve gastrectomy* are the short gastrics and left gastroepiploic, which stem from the **splenic artery**.
*Left gastric artery*
- The **left gastric artery** primarily supplies the lesser curvature of the stomach near the cardia and arises directly from the **celiac trunk**.
- Its branches would not be the primary vessels ligated in a procedure focused on the **greater curvature**.
*Gastroduodenal artery*
- The **gastroduodenal artery** arises from the **common hepatic artery** and typically supplies the pylorus, duodenum, and head of the pancreas, giving rise to the **right gastroepiploic artery**.
- It is not the main source of arterial supply to the proximal and middle greater curvature resected during a sleeve gastrectomy.
*Right gastric artery*
- The **right gastric artery** typically arises from the **common hepatic artery** or **proper hepatic artery** and primarily supplies the lesser curvature of the stomach.
- Its role in the robust blood supply to the **greater curvature** is minimal, and its ligation would not be central to a sleeve gastrectomy focused on this region.
More Peritoneum and peritoneal cavity US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.