Mediastinum and heart US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Mediastinum and heart. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
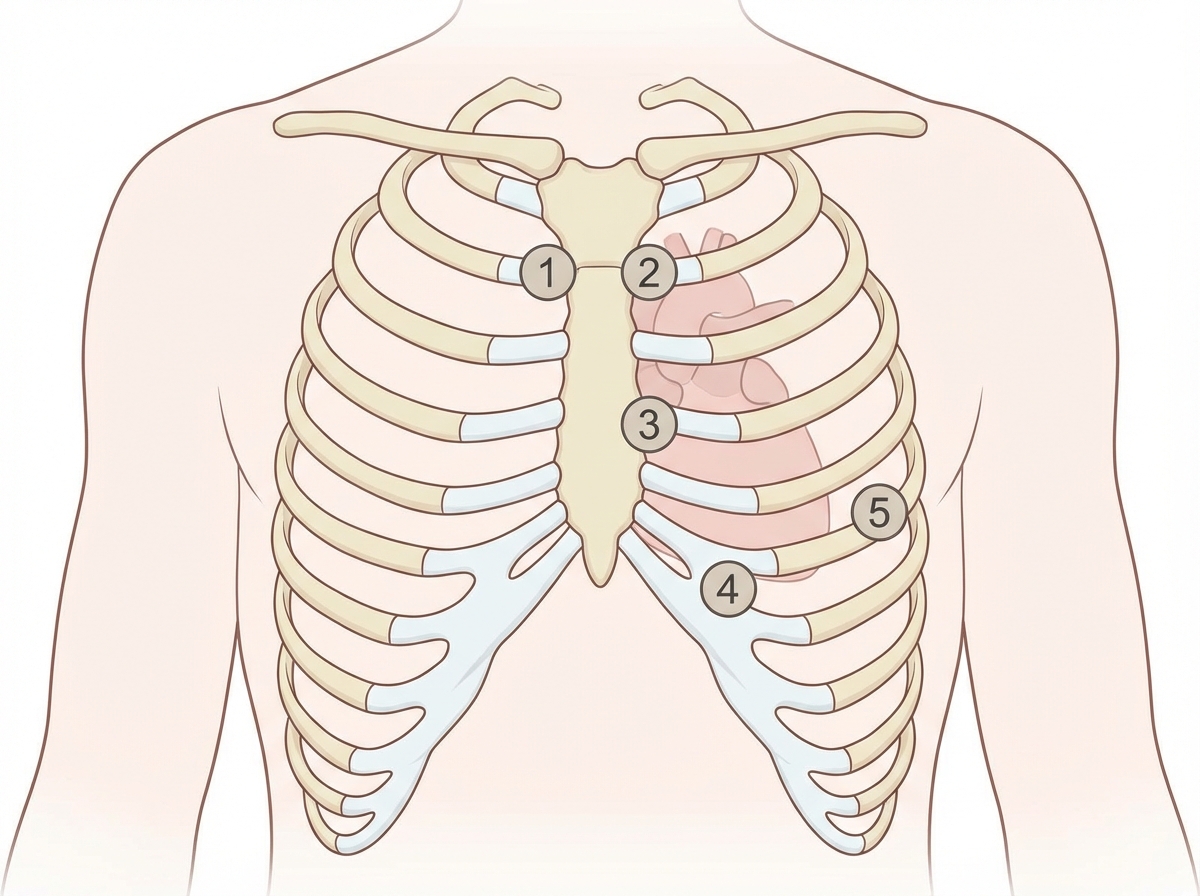
Mediastinum and heart US Medical PG Question 1: A 27-year-old woman, who recently immigrated from Bangladesh, presents to her primary care physician to discuss birth control. During a review of her past medical history, she reports that as a child she had a recurrent sore throat and fever followed by swollen and aching hip and knee joints. These symptoms returned every season and were never treated but went away on their own only to return with the next typhoon season. When asked about any current complaints, the patient says that she sometimes has shortness of breath and palpitations that do not last long. A physical exam is performed. In which of the auscultation sites will a murmur most likely be heard in this patient?
- A. Point 5 (Correct Answer)
- B. Point 4
- C. Point 2
- D. Point 3
- E. Point 1
Mediastinum and heart Explanation: ***Point 5***
- The patient's history of recurrent sore throat, fever, and migratory polyarthritis (swollen and aching hip and knee joints) followed by intermittent shortness of breath and palpitations is highly suggestive of **rheumatic fever** with subsequent **rheumatic heart disease**.
- This condition most commonly affects the **mitral valve**, leading to **mitral stenosis** or regurgitation, which would produce an apical murmur heard best at point 5 (the cardiac apex).
*Point 4*
- Point 4 corresponds to the **tricuspid area** (lower left sternal border). While rheumatic heart disease can affect the tricuspid valve, it is less common than mitral valve involvement and usually occurs in conjunction with severe mitral valve disease.
- An isolated murmur here would suggest tricuspid valve pathology, which is less likely as the primary presentation in rheumatic heart disease.
*Point 2*
- Point 2 is the **pulmonic area** (left upper sternal border, second intercostal space). Murmurs heard here typically indicate pulmonary valve disease or flow murmurs.
- While pulmonary hypertension can be a complication of severe left-sided heart disease, primary pulmonic valve involvement in rheumatic heart disease is rare.
*Point 3*
- Point 3 (Erb's point, third intercostal space, left sternal border) is often used to auscultate for murmurs of **aortic regurgitation** or to hear the splitting of S2.
- While aortic valve involvement can occur in rheumatic heart disease, **mitral valve disease** is significantly more prevalent and typically presents earlier and more severely.
*Point 1*
- Point 1 is the **aortic area** (right upper sternal border, second intercostal space). Murmurs heard here are typically associated with **aortic stenosis** or regurgitation.
- Although the aortic valve can be affected by rheumatic heart disease, the mitral valve is the most commonly involved valve, making an apical murmur (Point 5) more likely for the initial and most prominent finding.
Mediastinum and heart US Medical PG Question 2: A 38-year-old woman presents with fever and acute onset chest pain for the past 12 hours. She describes the pain as severe, sharp and stabbing in character, and localized to the retrosternal area. She also says the pain is worse when she breathes deeply or coughs. Past medical history is significant for recently diagnosed systemic lupus erythematosus (SLE). Her vital signs include: blood pressure 110/75 mm Hg, pulse 95/min, and temperature 38.0°C (100.4°F). Physical examination is significant for a friction rub heard best at the lower left sternal border. Which of the following is the most likely diagnosis in this patient?
- A. Acute myocardial infarction
- B. Septic shock
- C. Pericardial tamponade
- D. Constrictive pericarditis
- E. Acute pericarditis (Correct Answer)
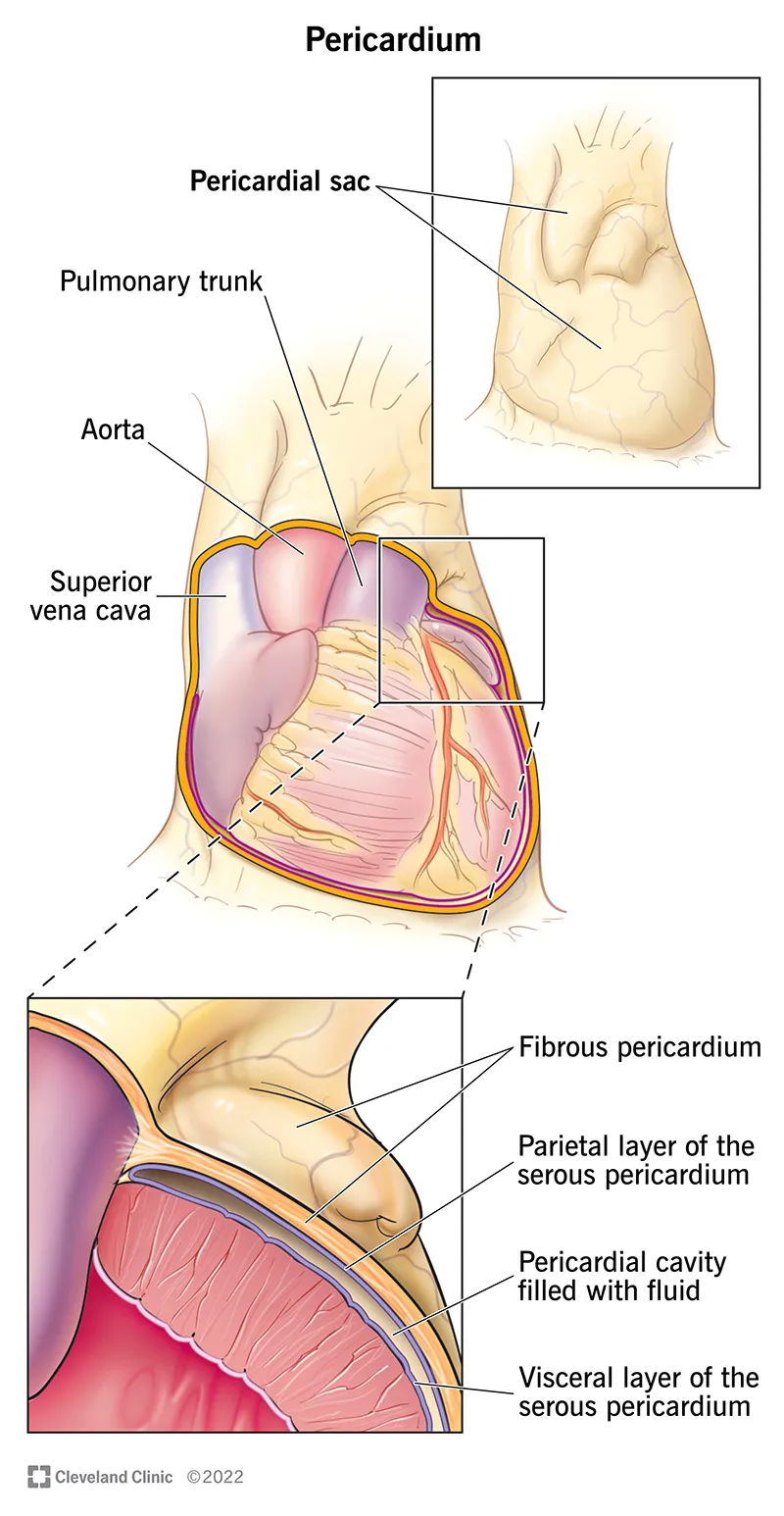
Mediastinum and heart Explanation: ***Acute pericarditis***
- This patient's symptoms of **acute onset, sharp, retrosternal chest pain** that is **worse with deep breathing or coughing**, accompanied by a **pericardial friction rub** and fever, are classic for **acute pericarditis**.
- The history of **systemic lupus erythematosus (SLE)** is a significant risk factor for pericarditis, as SLE can cause serositis (inflammation of serous membranes including the pericardium).
*Acute myocardial infarction*
- While chest pain is present, the description of **sharp, stabbing pain worse with breathing** is more typical of pericarditis than the **crushing, pressure-like pain of an MI** that often radiates to the arm or jaw.
- The presence of a **pericardial friction rub** is highly suggestive of pericarditis and not typically found in MI.
*Septic shock*
- This patient's vital signs, including a blood pressure of **110/75 mmHg**, do not indicate **hypotension** as seen in septic shock.
- While fever is present, the primary presentation is **chest pain** and a **friction rub**, not generalized signs of severe infection and organ dysfunction.
*Pericardial tamponade*
- Pericardial tamponade would present with signs of **hemodynamic compromise** such as **hypotension**, **tachycardia**, **muffled heart sounds**, and **jugular venous distention (Beck's triad)**, which are not described.
- The primary symptom is **chest pain** and a **friction rub** indicative of inflammation, not significant fluid accumulation causing cardiac compression.
*Constrictive pericarditis*
- **Constrictive pericarditis** typically presents with signs of **chronic right-sided heart failure** such as **peripheral edema**, **ascites**, and **jugular venous distention**, often after a prolonged course of pericardial inflammation.
- This patient presents with **acute symptoms** and signs of **active inflammation** (fever, friction rub), which is not consistent with the chronic nature of constrictive pericarditis.
Mediastinum and heart US Medical PG Question 3: A 74-year-old woman is brought by ambulance to the emergency department and presents with a complaint of excruciating chest pain that started about 45 minutes ago. The patient was sitting in the garden when she 1st noticed the pain in the upper abdomen. The pain has persisted and now localizes underneath of the sternum and the left shoulder. Milk of magnesia and aspirin were tried with no relief. The patient had previous episodes of chest pain that were of lesser intensity and rarely lasted more than 10 minutes. She is diabetic and has been managed for hypertension and rheumatoid arthritis in the past. On examination, the patient is breathless and sweating profusely. The vital signs include blood pressure 140/90 mm Hg and heart rate 118/min. The electrocardiogram (ECG) shows Q waves in leads V2 and V3 and raised ST segments in leads V2, V3, V4, and V5. Laboratory studies (including cardiac enzymes at 6 hours after admission show:
Hematocrit 45%
Troponin T 1.5 ng/mL
Troponin I 0.28 ng/mL
Creatine kinase (CK)-MB 0.25 ng/mL
The patient is admitted and started on analgesia and reperfusion therapy. She shows initial signs of recovery until the 6th day of hospitalization when she starts vomiting and complaining of dizziness. Physical examination findings at this time included heart rate 110/min, temperature 37.7°C (99.9°F), blood pressure 90/60 mm Hg. Jugular venous pressure is 8 cm. A harsh pansystolic murmur is present at the left lower sternal border. ECG shows sinus tachycardia and ST-segment elevation with terminal negative T waves. Laboratory studies show:
Hematocrit 38%
Troponin T 1.15ng/mL
Troponin I 0.18 ng/mL
CK-MB 0.10 ng/mL
Which of the following best explains the patient's current clinical condition?
- A. Aortic dissection complicating myocardial infarction
- B. A new myocardial infarction (re-infarction)
- C. Acute ventricular septal rupture complicating myocardial infarction (Correct Answer)
- D. Acute pericarditis complicating myocardial infarction
- E. Cardiac tamponade complicating myocardial infarction
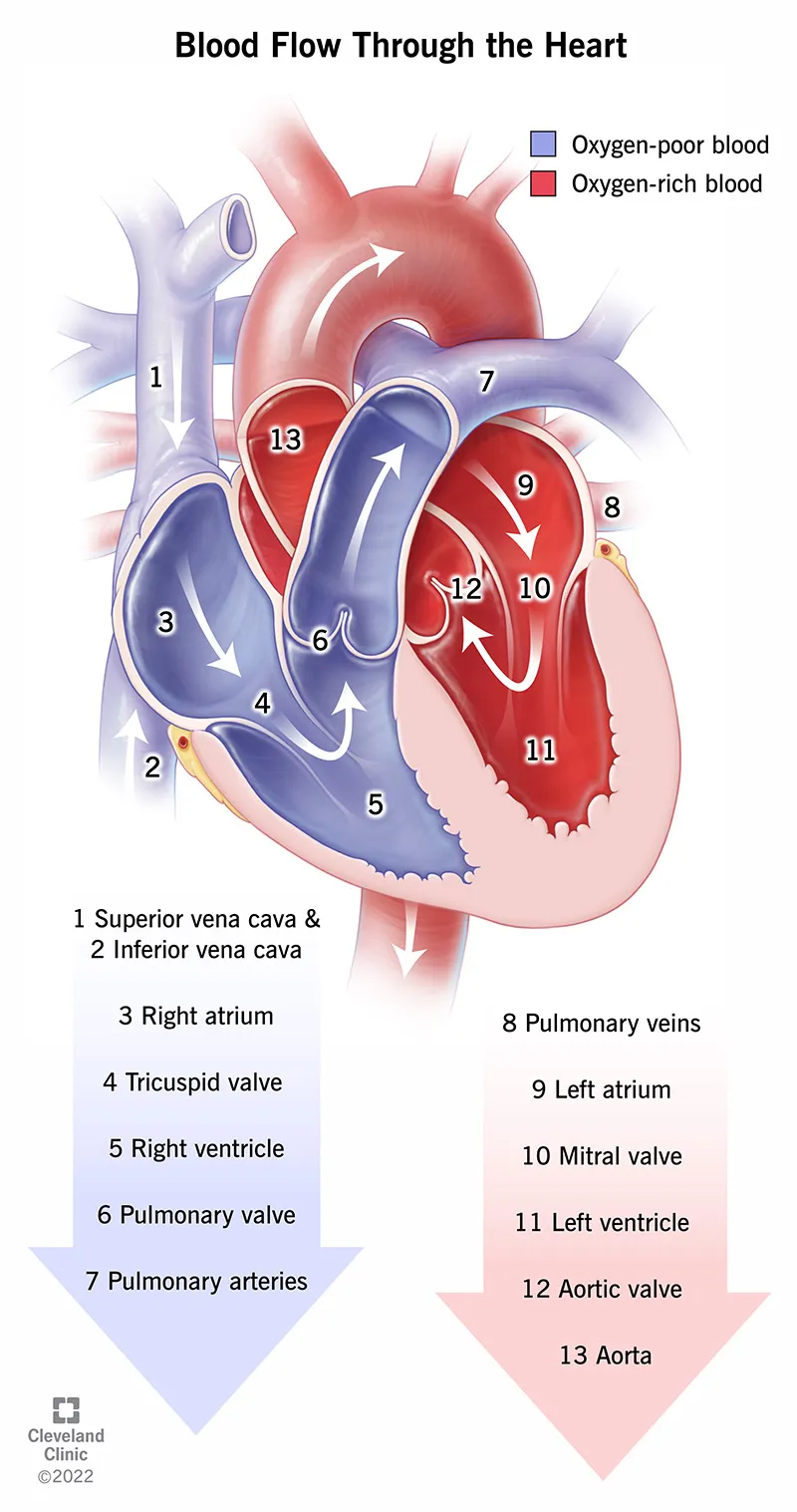
Mediastinum and heart Explanation: ***Acute ventricular septal rupture complicating myocardial infarction***
- The development of a **harsh pansystolic murmur** at the **left lower sternal border** along with signs of **heart failure** (hypotension, tachycardia, increased JVP) approximately a week after a large anterior MI is highly suggestive of **ventricular septal rupture (VSR)**.
- The continued ECG changes (ST elevation with terminal negative T waves) and elevated, though improving, cardiac enzymes are consistent with the ongoing myocardial injury and the complications related to it.
*Aortic dissection complicating myocardial infarction*
- **Aortic dissection** typically presents with **sudden, severe, tearing chest pain** radiating to the back, which is distinct from the patient's initial presentation.
- While it can cause hemodynamic instability, it does not typically produce a **pansystolic murmur** at the left lower sternal border.
*A new myocardial infarction (re-infarction)*
- While the patient is still experiencing symptoms and some ECG changes, the **prominent new pansystolic murmur** and signs of acute heart failure are more indicative of a **mechanical complication** than simply a new MI.
- The cardiac enzyme levels, though still elevated, are trending downwards, which would be inconsistent with a large new infarction.
*Acute pericarditis complicating myocardial infarction*
- **Acute pericarditis** would typically present with **pleuritic chest pain** that improves when leaning forward and a characteristic **pericardial friction rub**.
- It would not explain the **pansystolic murmur** or the sudden hemodynamic deterioration to the same extent as VSR.
*Cardiac tamponade complicating myocardial infarction*
- **Cardiac tamponade** is characterized by **Beck's triad** (hypotension, JVD, muffled heart sounds) and pulsus paradoxus. While the patient has hypotension and JVD, the presence of a **harsh pansystolic murmur** points away from tamponade and towards a structural defect.
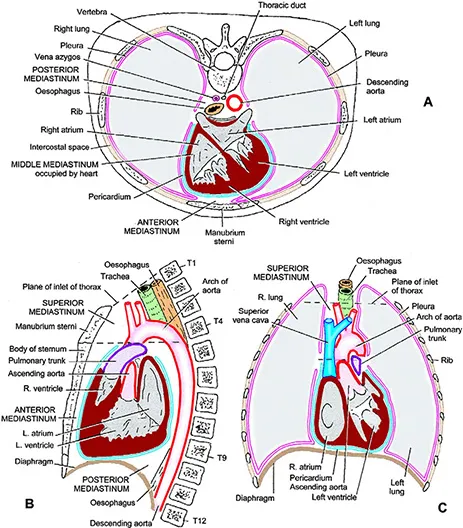
Mediastinum and heart US Medical PG Question 4: During a thoracotomy procedure, a surgeon needs to access the posterior mediastinum. Which of the following structures forms the anterior boundary of the posterior mediastinum?
- A. Descending thoracic aorta
- B. Pericardial sac (Correct Answer)
- C. Azygos vein
- D. Thoracic vertebrae
- E. Sternum
Mediastinum and heart Explanation: ***Pericardial sac***
- The **pericardial sac** (and the diaphragm, inferiorly) forms the anterior boundary of the **posterior mediastinum** [1].
- This anatomical relationship is crucial for surgeons during thoracotomy to distinguish between the middle and posterior mediastinal compartments [1].
*Descending thoracic aorta*
- The **descending thoracic aorta** is a large vessel located *within* the posterior mediastinum itself, typically running along its left side [2].
- Therefore, it is a content of the posterior mediastinum, not a boundary.
*Azygos vein*
- The **azygos vein** is also a major structure *within* the posterior mediastinum, running along the right side of the vertebral column.
- It is a content, not a boundary, of this compartment.
*Thoracic vertebrae*
- The **thoracic vertebrae** form the *posterior* boundary of the posterior mediastinum [1].
- This anatomical landmark gives the posterior mediastinum its name and defines its dorsal limit.
Mediastinum and heart US Medical PG Question 5: A researcher is studying how electrical activity propagates across the heart. In order to do this, he decides to measure the rate at which an action potential moves within various groups of cardiac muscle tissue. In particular, he isolates fibers from areas of the heart with the following characteristics:
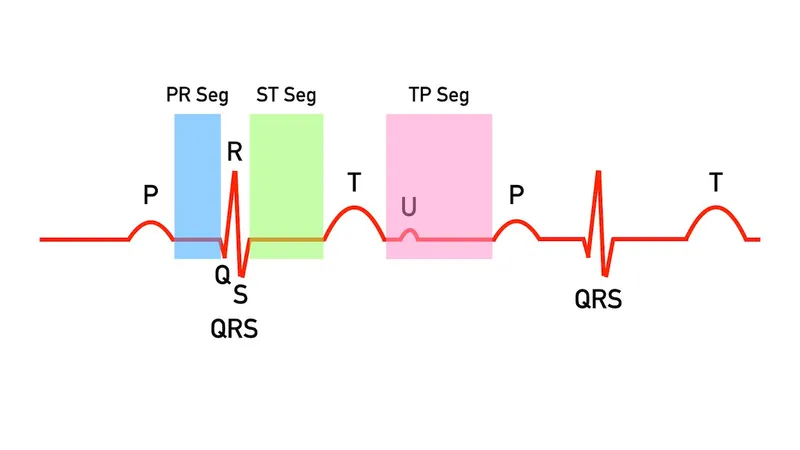
A) Dysfunction leads to fixed PR intervals prior to a dropped beat
B) Dysfunction leads to increasing PR intervals prior to a dropped beat
C) Dysfunction leads to tachycardia with a dramatically widened QRS complex
D) Dysfunction leads to tachycardia with a sawtooth pattern on electrocardiogram
Which of the following is the proper order of these tissues from fastest action potential propagation to slowest action potential propagation.
- A. B > D > C > A
- B. D > C > A > B
- C. B > C > D > A
- D. A > D > C > B (Correct Answer)
- E. A > C > D > B
Mediastinum and heart Explanation: ***A > D > C > B***
* **Purkinje fibers (A)** have the fastest conduction velocity in the heart to ensure rapid and synchronous ventricular depolarization. The description of "fixed PR intervals prior to a dropped beat" in **Mobitz type II second-degree AV block** indicates an issue with conduction distal to the AV node, often in the His-Purkinje system, while still maintaining typical conduction through the atria and AV node for conducted beats.
* **Atrial muscle (D)** has a faster conduction velocity than the AV node but slower than Purkinje fibers. The "sawtooth pattern on electrocardiogram" unequivocally points to **atrial flutter**, which is characterized by rapid, regular depolarization of the atria.
* **Ventricular muscle (C)** has a conduction velocity slower than Purkinje fibers but faster than the AV node. "Tachycardia with a dramatically widened QRS complex" is characteristic of **ventricular tachycardia (VT)**, which arises from abnormal electrical activity within the ventricles.
* **AV node (B)** has the slowest conduction velocity in the heart, which allows for proper ventricular filling. "Increasing PR intervals prior to a dropped beat" describes **Mobitz type I second-degree AV block (Wenckebach phenomenon)**, which is due to progressive prolongation of conduction delay within the AV node itself.
*B > D > C > A*
* This order incorrectly places the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest, which is contrary to the known conduction velocities in the heart.
* The AV node is critical for delaying the impulse, making it the slowest, while Purkinje fibers are designed for rapid spread, making them the fastest.
*D > C > A > B*
* This option incorrectly places **atrial muscle (D)** as faster than **Purkinje fibers (A)**. Purkinje fibers have the fastest conduction velocity in the heart, considerably faster than atrial muscle.
*B > C > D > A*
* This arrangement incorrectly lists the **AV node (B)** as the fastest and **Purkinje fibers (A)** as the slowest. The AV node is the slowest for its physiological role of delaying ventricular contraction, while Purkinje fibers are optimized for rapid conduction.
*A > C > D > B*
* While placing **Purkinje fibers (A)** as the fastest and the **AV node (B)** as the slowest is correct, this order incorrectly places **ventricular muscle (C)** as faster than **atrial muscle (D)**. Atrial muscle generally conducts faster than ventricular muscle in normal physiology.
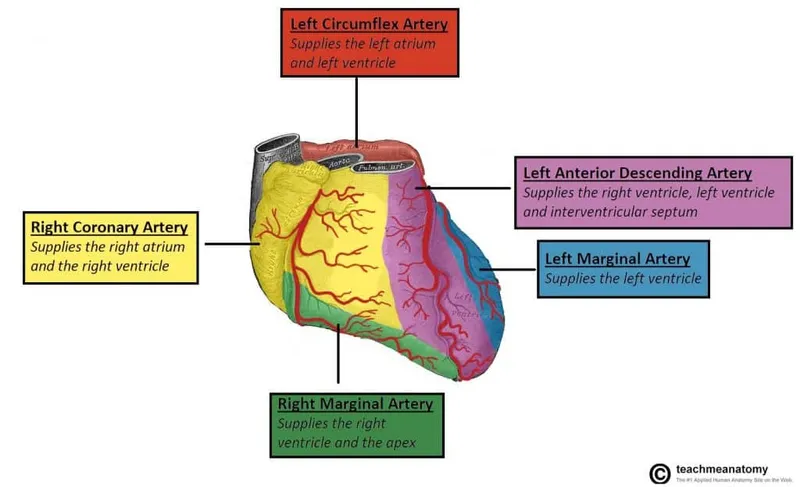
Mediastinum and heart US Medical PG Question 6: A 27-year-old man is brought to the emergency department after a motorcycle accident 30 minutes ago. He was found at the scene of the accident with a major injury to the anterior chest by a metallic object that was not removed during transport to the hospital. The medical history could not be obtained. His blood pressure is 80/50 mm Hg, pulse is 130/min, and respiratory rate is 40/min. Evaluation upon arrival to the emergency department reveals a sharp metal object penetrating through the anterior chest to the right of the sternum at the 4th intercostal space. The patient is taken to the operating room immediately, where it is shown the heart has sustained a major injury. Which of the following arteries supplies the part of the heart most likely injured in this patient?
- A. Right marginal artery (Correct Answer)
- B. Left anterior descending artery
- C. Left coronary artery
- D. Posterior descending artery
- E. Left circumflex coronary artery
Mediastinum and heart Explanation: ***Right marginal artery***
- The right marginal artery typically arises from the **right coronary artery** and supplies the **right ventricle**.
- Given the injury location to the **right of the sternum** and the 4th intercostal space, the right ventricle is the most superficial and anterior chamber and thus the most likely to be injured.
*Left anterior descending artery*
- The left anterior descending artery supplies the **anterior** two-thirds of the **interventricular septum** and the anterior wall of the **left ventricle**.
- While located anteriorly, it is generally to the left of the sternum and would be protected by the more anterior right ventricle from an injury to the right of the sternum.
*Left coronary artery*
- The left coronary artery is a **short main stem** that quickly branches into the left anterior descending and left circumflex arteries.
- It is located more superiorly and to the left, making it less likely to be directly injured by a penetrating trauma to the **right of the sternum** at the 4th intercostal space.
*Posterior descending artery*
- The posterior descending artery supplies the **posterior** wall of both ventricles and the posterior one-third of the **interventricular septum**.
- This vessel is located on the posterior aspect of the heart, making it extremely unlikely to be injured by an anterior penetrating trauma.
*Left circumflex coronary artery*
- The left circumflex coronary artery supplies the **lateral and posterior walls of the left ventricle** and the left atrium.
- Its location on the posterior-lateral aspect of the heart makes it much less vulnerable to a penetrating injury coming from the **anterior chest**.
Mediastinum and heart US Medical PG Question 7: A 68-year-old man comes to the physician because of a 4-month history of difficulty swallowing. During this time, he has also had a 7-kg (15-lb) weight loss. Esophagogastroduodenoscopy shows an exophytic mass in the distal third of the esophagus. Histological examination of a biopsy specimen shows a well-differentiated adenocarcinoma. The patient is scheduled for surgical resection of the tumor. During the procedure, the surgeon damages a structure that passes through the diaphragm along with the esophagus at the level of the tenth thoracic vertebra (T10). Which of the following structures was most likely damaged?
- A. Azygos vein
- B. Vagus nerve (Correct Answer)
- C. Right phrenic nerve
- D. Inferior vena cava
- E. Thoracic duct
Mediastinum and heart Explanation: ***Vagus nerve***
- The **esophagus** passes through the diaphragm at the level of the **T10 vertebra**, accompanied by the **anterior and posterior vagal trunks**. Damage to these nerves is a known complication of esophageal surgery.
- The vagus nerves provide **parasympathetic innervation** to the gastrointestinal tract, and their close proximity to the esophagus makes them vulnerable during tumor resection.
*Azygos vein*
- The **azygos vein** typically passes through the diaphragm at the level of **T12** through the **aortic hiatus**, not with the esophagus at T10.
- It drains into the superior vena cava and is located more posteriorly in the mediastinum.
*Right phrenic nerve*
- The **right phrenic nerve** passes through the diaphragm with the **inferior vena cava** at the level of **T8**, innervating the diaphragm.
- It is located more anteriorly and laterally to the esophagus, making direct damage during esophageal surgery less likely than the vagus nerves.
*Inferior vena cava*
- The **inferior vena cava (IVC)** passes through its own opening in the central tendon of the diaphragm at the level of **T8**, not with the esophagus at T10.
- Damage to the IVC would result in significant hemorrhage and is typically a separate surgical concern.
*Thoracic duct*
- The **thoracic duct** passes through the **aortic hiatus** at the level of **T12** along with the aorta, collecting lymph from most of the body.
- Its location makes it less likely to be damaged during a standard esophageal resection at T10 compared to the vagus nerves.
Mediastinum and heart US Medical PG Question 8: A 3175-g (7-lb) male newborn is delivered at 39 weeks' gestation to a 29-year-old primigravid woman following a spontaneous vaginal delivery. Apgar scores are 8 and 9 at 1 and 5 minutes, respectively. Cardiac examination in the delivery room shows a continuous machine-like murmur. An echocardiogram shows a structure with blood flow between the pulmonary artery and the aorta. This structure is most likely a derivate of which of the following?
- A. 4th aortic arch
- B. 1st aortic arch
- C. 6th aortic arch (Correct Answer)
- D. 2nd aortic arch
- E. 3rd aortic arch
Mediastinum and heart Explanation: ***6th aortic arch***
- The description of a "continuous machine-like murmur" and a structure with blood flow between the pulmonary artery and the aorta is characteristic of a **patent ductus arteriosus (PDA)**.
- The **ductus arteriosus** is a remnant of the **6th aortic arch**, connecting the pulmonary artery to the aorta in fetal life.
*4th aortic arch*
- The **4th aortic arch** contributes to the formation of the **aortic arch** itself on the left side and the proximal **right subclavian artery** on the right.
- Abnormalities of the 4th arch can lead to conditions like **coarctation of the aorta** or **vascular rings**, which do not typically present as a PDA.
*1st aortic arch*
- The **1st aortic arch** largely disappears, but its remnants contribute to the formation of the **maxillary artery** and the **external carotid artery**.
- It is not involved in developmental anomalies of the major vessels between the pulmonary artery and aorta.
*2nd aortic arch*
- The **2nd aortic arch** also largely regresses, but its remnants contribute to the **stapedial artery** and part of the **hyoid artery**.
- It does not play a role in the formation of the ductus arteriosus or other major arteries of the heart.
*3rd aortic arch*
- The **3rd aortic arch** develops into the common carotid arteries and the proximal internal carotid arteries.
- Genetic disorders and malformations involving this arch typically affect the carotid system, not the connection between the pulmonary artery and aorta.
Mediastinum and heart US Medical PG Question 9: A 55-year-old man comes to the emergency department because of left-sided chest pain and difficulty breathing for the past 30 minutes. His pulse is 88/min. He is pale and anxious. Serum studies show increased cardiac enzymes. An ECG shows ST-elevations in leads I, aVL, and V5-V6. A percutaneous coronary intervention is performed. In order to localize the site of the lesion, the catheter must pass through which of the following structures?
- A. Left coronary artery → left circumflex artery (Correct Answer)
- B. Right coronary artery → posterior descending artery
- C. Left coronary artery → left anterior descending artery
- D. Right coronary artery → right marginal artery
- E. Left coronary artery → posterior descending artery
Mediastinum and heart Explanation: ***Left coronary artery → left circumflex artery***
- **ST-elevations** in leads I, aVL, and V5-V6 are indicative of a **lateral myocardial infarction**.
- The **left circumflex artery** primarily supplies the lateral wall of the left ventricle.
*Right coronary artery → posterior descending artery*
- The **posterior descending artery** (PDA) typically supplies the inferior wall and posterior interventricular septum.
- An occlusion here would cause **ST-elevations** in leads II, III, and aVF, which is not seen in this case.
*Left coronary artery → left anterior descending artery*
- The **left anterior descending** (LAD) artery supplies the anterior wall and apex of the left ventricle.
- Occlusion of the LAD would typically cause **ST-elevations** in leads V1-V4, indicating an anterior MI.
*Right coronary artery → right marginal artery*
- The **right marginal artery** is a branch of the right coronary artery and supplies part of the right ventricle.
- Occlusion here would primarily affect the **right ventricle**, and is not typically associated with the given ECG changes.
*Left coronary artery → posterior descending artery*
- While the **posterior descending artery** can sometimes originate from the left circumflex artery (**left dominant circulation**), it primarily supplies the inferior wall.
- The observed ECG changes in leads I, aVL, and V5-V6 are characteristic of a **lateral wall infarct**, which is supplied by the left circumflex artery.
Mediastinum and heart US Medical PG Question 10: A 42-year-old Caucasian woman is enrolled in a randomized controlled trial to study cardiac function in the setting of several different drugs. She is started on verapamil and instructed to exercise at 50% of her VO2 max while several cardiac parameters are being measured. During this experiment, which of the following represents the relative conduction speed through the heart from fastest to slowest?
- A. Purkinje fibers > ventricles > atria > AV node
- B. Purkinje fibers > atria > ventricles > AV node (Correct Answer)
- C. Atria > Purkinje fibers > ventricles > AV node
- D. AV node > ventricles > atria > Purkinje fibers
- E. Purkinje fibers > AV node > ventricles > atria
Mediastinum and heart Explanation: ***Purkinje fibers > atria > ventricles > AV node***
- The **Purkinje fibers** have the fastest conduction velocity, ensuring rapid and synchronous ventricular depolarization.
- The **atria** conduct impulses faster than the ventricles, but slower than the Purkinje fibers, allowing for atrial contraction before ventricular systole.
*Purkinje fibers > ventricles > atria > AV node*
- This option correctly identifies the **Purkinje fibers** and **AV node** at the fastest and slowest ends, respectively, but incorrectly orders the atria and ventricles.
- While Purkinje fibers are fastest, cardiac muscle cells (atria then ventricles) conduct slower than Purkinje fibers.
*Atria > Purkinje fibers > ventricles > AV node*
- This option incorrectly places the **atria** as having the fastest conduction speed, which is not true as Purkinje fibers are significantly faster.
- It also misorders the Purkinje fibers relative to the atria in terms of speed.
*AV node > ventricles > atria > Purkinje fibers*
- This option is incorrect as it places the **AV node** as the fastest conductor and the **Purkinje fibers** as the slowest, which is the exact opposite of their actual conduction speeds.
- The AV node is known for its slow conduction to allow for ventricular filling.
*Purkinje fibers > AV node > ventricles > atria*
- This option incorrectly places the **AV node** as the second fastest conductor, and the ventricles as slower than the atria.
- The AV node is specifically designed to slow the impulse to allow for proper ventricular filling.
More Mediastinum and heart US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.