Great vessels and lymphatics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Great vessels and lymphatics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Great vessels and lymphatics US Medical PG Question 1: A 72-year-old man presents to his primary care physician because he has been having flank and back pain for the last 8 months. He said that it started after he fell off a chair while doing yard work, but it has been getting progressively worse over time. He reports no other symptoms and denies any weight loss or tingling in his extremities. His medical history is significant for poorly controlled hypertension and a back surgery 10 years ago. He drinks socially and has smoked 1 pack per day since he was 20. His family history is significant for cancer, and he says that he is concerned that his father had similar symptoms before he was diagnosed with multiple myeloma. Physical exam reveals a painful, pulsatile enlargement in the patient's abdomen. Between which of the following locations has the highest risk of developing this patient's disorder?
- A. Superior mesenteric artery and renal arteries
- B. Diaphragm and renal arteries
- C. Renal arteries and common iliac arteries (Correct Answer)
- D. Superior mesenteric artery and common iliac arteries
- E. Diaphragm and superior mesenteric artery
Great vessels and lymphatics Explanation: ***Renal arteries and common iliac arteries***
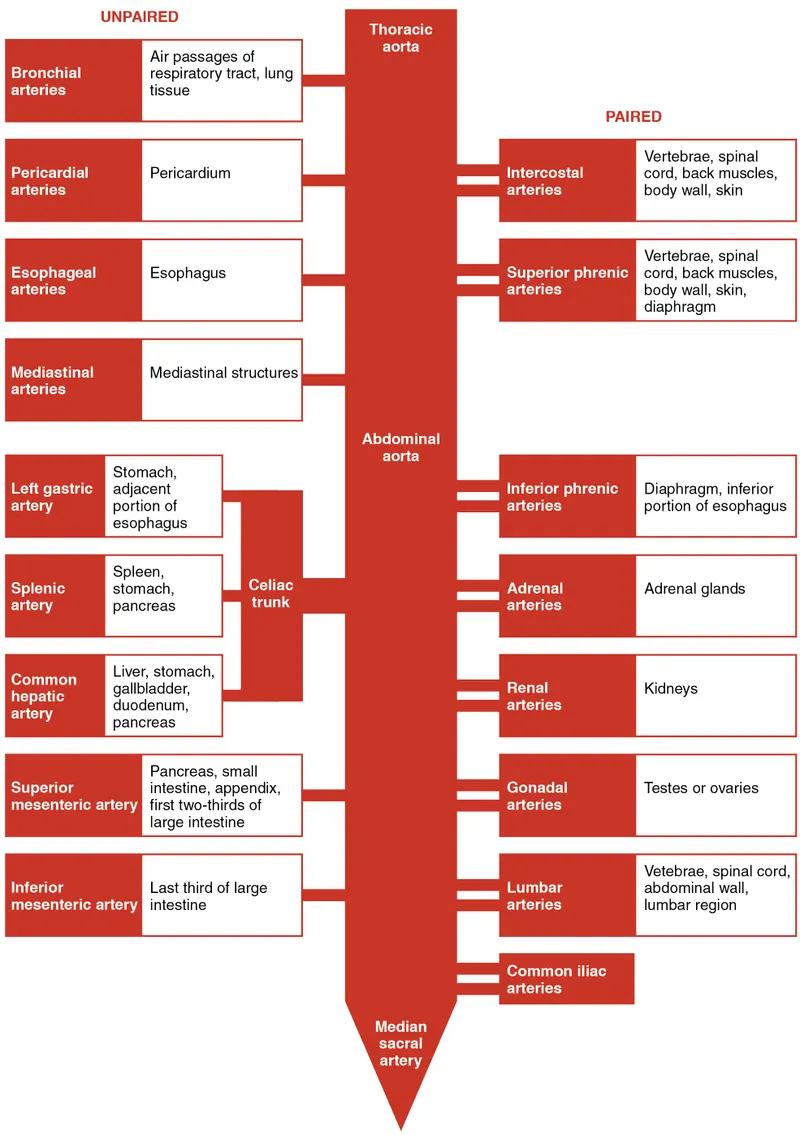
- The most common location for **abdominal aortic aneurysms (AAAs)** is the **infrarenal aorta**, specifically between the renal arteries and the common iliac arteries.
- This segment accounts for **~95% of all AAAs** due to decreased elastin content, hemodynamic stress, and reduced vasa vasorum.
- The patient's presentation with **flank/back pain**, a **pulsatile abdominal mass**, and risk factors like **hypertension** and **smoking** are highly suggestive of an infrarenal AAA [1].
*Superior mesenteric artery and renal arteries*
- This region defines the **suprarenal aorta**, which is less commonly affected by aneurysms than the infrarenal segment.
- Suprarenal aneurysms account for only **~5% of AAAs** and are typically more complex to manage.
*Diaphragm and renal arteries*
- This encompasses a significant portion of the **thoracoabdominal aorta**, including the suprarenal segment.
- While thoracoabdominal aneurysms can occur, they are much less common than infrarenal AAAs and often have different etiologies.
*Superior mesenteric artery and common iliac arteries*
- This range is anatomically imprecise and spans too broad a region, including both suprarenal and infrarenal segments.
- The **superior mesenteric artery** originates anteriorly from the aorta (typically at L1), well above the most common aneurysm site immediately distal to the renal arteries (L1-L2).
- The highest risk is specifically localized to the segment **below the renal arteries**, not this entire broad region.
*Diaphragm and superior mesenteric artery*
- This describes the **supraceliac and proximal suprarenal aorta**, an area significantly less prone to aneurysms compared to the infrarenal segment.
- Aneurysms in this more proximal segment are rare and often have different etiologies (e.g., connective tissue disorders).
Great vessels and lymphatics US Medical PG Question 2: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Great vessels and lymphatics Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
Great vessels and lymphatics US Medical PG Question 3: Six days after undergoing a thoracic endovascular aortic repair following a high-speed motorcycle accident, a 29-year-old woman develops a fever, cough, and shortness of breath. Serum studies show a sodium concentration of 129 mEq/L. An x-ray of the chest shows a left-sided pleural effusion. Thoracentesis is performed and shows milky white fluid in the pleural space that remains uniform after centrifugation. A culture of the pleural fluid shows no organisms. Further analysis of the fluid would most likely show which of the following?
- A. Cholesterol crystals
- B. High triglycerides (Correct Answer)
- C. Antinuclear antibodies
- D. High LDH
- E. High adenosine deaminase
Great vessels and lymphatics Explanation: ***High triglycerides***
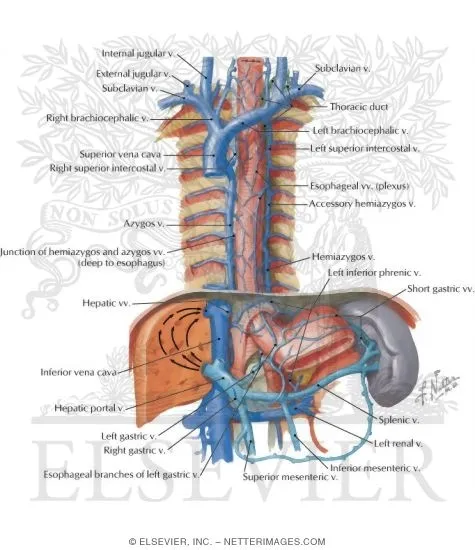
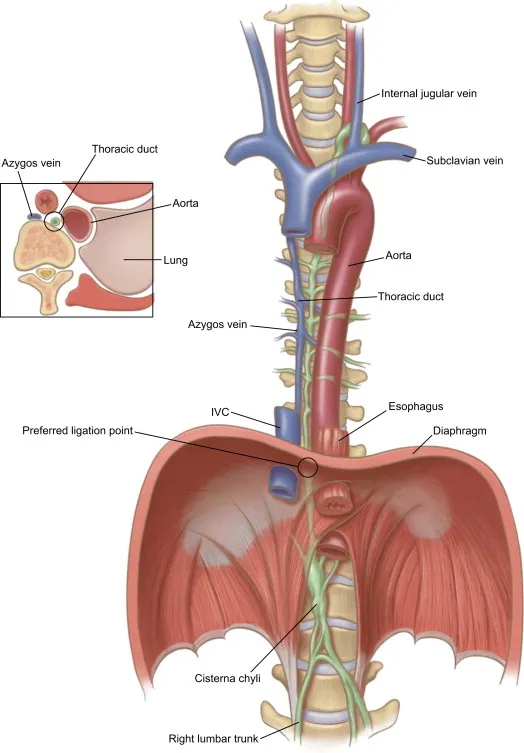
- The milky white pleural fluid that remains uniform after centrifugation describes **chylous effusion**, which is characterized by a **high triglyceride concentration** (typically >110 mg/dL) [1].
- **Chylous effusion** results from disruption of the **thoracic duct**, leading to leakage of **chyle** (lymphatic fluid rich in triglycerides) into the pleural space [1]. This patient's recent **thoracic endovascular aortic repair (TEVAR)** could have injured the thoracic duct.
*Cholesterol crystals*
- **Pseudochylous effusions** (or cholesterol effusions) also appear milky but will separate into layers upon centrifugation, with a supernatant and a creamy layer at the top, and are characterized by high cholesterol levels and the presence of **cholesterol crystals**.
- These effusions typically develop in chronic inflammatory conditions like tuberculosis or rheumatoid arthritis and are not associated with recent trauma or surgery in the same way as chylous effusions.
*Antinuclear antibodies*
- **Antinuclear antibodies (ANAs)** are markers associated with autoimmune diseases such as **systemic lupus erythematosus (SLE)**, which can cause pleuritis and pleural effusions.
- While SLE can cause pleural effusions, the milky appearance of the fluid and the recent thoracic surgery are not suggestive of an autoimmune etiology.
*High LDH*
- Elevated **lactate dehydrogenase (LDH)** in pleural fluid is a nonspecific marker indicating **cellular injury** or **inflammation**, often seen in exudative effusions [1].
- While it might be present, it does not specifically characterize the **milky white fluid** that remains uniform after centrifugation, which points more directly to a chyle-related issue.
*High adenosine deaminase*
- **High adenosine deaminase (ADA)** levels in pleural fluid are primarily indicative of **tuberculous pleurisy**.
- This patient's presentation with recent thoracic surgery and a milky effusion is not consistent with **tuberculosis**.
Great vessels and lymphatics US Medical PG Question 4: A 29-year-old man presents to his primary care provider complaining of testicular pain. He reports a four-day history of dull chronic pain in his left testicle that is worse with standing. His past medical history is notable for asthma and major depressive disorder. He takes inhaled albuterol as needed and sertraline. He is sexually active with a single female partner and always uses barrier protection. His temperature is 99.2°F (37.3°C), blood pressure is 125/75 mmHg, pulse is 85/min, and respirations are 17/min. Physical examination reveals a non-tender twisted mass along the left spermatic cord that disappears when the patient lies supine. This patient’s condition most likely stems from decreased laminar flow at which of the following vascular junctions?
- A. Descending aorta – Left testicular artery
- B. Left testicular vein – Left suprarenal vein
- C. Left testicular vein – Inferior vena cava
- D. Left testicular vein – Left renal vein (Correct Answer)
- E. Left testicular vein – Left internal iliac vein
Great vessels and lymphatics Explanation: ***Left testicular vein – Left renal vein***
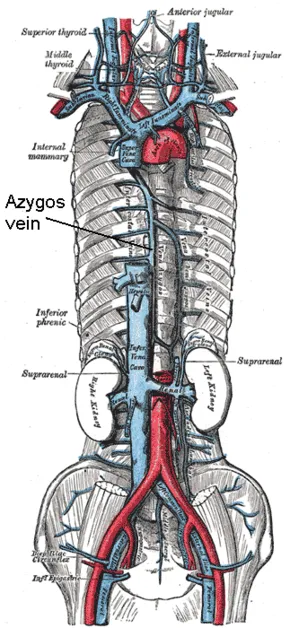
- This clinical presentation of a **nontender, twisted mass along the spermatic cord** that disappears when supine is classic for a **varicocele**. Varicoceles are more common on the left side due to the **anatomic drainage of the left testicular vein** into the left renal vein at a **perpendicular angle**.
- This perpendicular angle, along with the **increased length of the left testicular vein** and its drainage into the higher-pressure left renal vein, creates conditions for **increased hydrostatic pressure** and **decreased laminar flow**, leading to venous engorgement and varicocele formation.
*Descending aorta – Left testicular artery*
- This junction involves an **artery**, not a vein. Varicoceles are caused by **venous insufficiency and dilatation**, not arterial issues.
- The left testicular artery branches directly from the aorta and supplies blood to the testicle; problems with this junction would typically manifest as **ischemia or arterial insufficiency**, not venous congestion.
*Left testicular vein – Left suprarenal vein*
- While the left suprarenal vein also drains into the left renal vein, the **left testicular vein does not directly connect to the left suprarenal vein**.
- This junction is not anatomically relevant to the direct drainage pathway causing a varicocele.
*Left testicular vein – Inferior vena cava*
- The **right testicular vein drains directly into the inferior vena cava**, explaining why varicoceles are less common on the right side.
- The left testicular vein typically drains into the left renal vein, not directly into the inferior vena cava.
*Left testicular vein – Left internal iliac vein*
- The **left internal iliac vein primarily drains pelvic structures** and has no direct anatomical connection or primary drainage role for the left testicular vein.
- The testicular veins follow a retroperitoneal course and do not typically involve the internal iliac venous system in their main drainage.
Great vessels and lymphatics US Medical PG Question 5: A 56-year-old man with substernal chest pain calls 911. When paramedics arrive, they administer drug X sublingually for the immediate relief of angina. What is the most likely site of action of drug X?
- A. Pulmonary arteries
- B. Large veins (Correct Answer)
- C. Cardiac muscle
- D. Large arteries
- E. Arterioles
Great vessels and lymphatics Explanation: ***Large veins***
- Drug X is most likely **nitroglycerin**, which is administered sublingually for rapid relief of angina.
- Its primary mechanism of action involves **vasodilation of large veins**, leading to **decreased preload** and reduced myocardial oxygen demand.
*Pulmonary arteries*
- While nitroglycerin can cause some pulmonary vasodilation, its primary therapeutic effect in angina is not focused on the **pulmonary arteries**.
- Medications targeting pulmonary arteries are typically used for conditions like **pulmonary hypertension**.
*Cardiac muscle*
- Nitroglycerin does not directly act on **cardiac muscle** to improve angina; its effects are primarily vascular.
- It does not directly enhance contractility or directly reduce oxygen consumption at the myocardial cellular level.
*Large arteries*
- Nitroglycerin does cause some **arterial vasodilation**, but this effect is less prominent than its venodilating effect at typical anti-anginal doses.
- Significant arterial dilation can lead to **hypotension**, which is a side effect, not the primary therapeutic mechanism for angina relief.
*Arterioles*
- Nitroglycerin causes **less vasodilation of resistance arterioles** compared to its venodilating effects.
- While some arteriolar dilation occurs, it mainly contributes to a decrease in **afterload**, but the predominant effect for angina relief is preload reduction.
Great vessels and lymphatics US Medical PG Question 6: A 70-year-old male comes to the emergency department complaining of severe back pain. The pain started 20 minutes ago when he was sitting and watching TV. He describes the pain as intense, epigastric, and radiating to his back. His vitals on presentation to the emergency department are blood pressure is 150/75 mmHg, pulse is 110/min, and respirations are 24/min with an oxygen saturation of 98% on room air. His body mass index is 35 kg/m^2 and he appears pale and in visible pain. On abdominal exam, his abdomen is tender and a pulsatile mass is felt in the midline during deep palpation. His past medical history includes diabetes, hypertension well-controlled on medications, and a history of benign prostatic hyperplasia. His social history is notable for consuming 2-3 beers per night and a smoking history of ½ pack per day. Which of the following is considered the greatest risk factor for this patient's condition?
- A. Smoking (Correct Answer)
- B. Benign prostatic hyperplasia
- C. Obesity
- D. Diabetes
- E. Alcohol consumption
Great vessels and lymphatics Explanation: ***Smoking***
- **Smoking** is the single most significant modifiable risk factor for the development and expansion of **abdominal aortic aneurysms (AAAs)** due to its detrimental effects on arterial wall integrity.
- Nicotine and other toxins in smoke contribute to **inflammation**, **oxidative stress**, and **elastin degradation** within the aortic wall.
*Benign prostatic hyperplasia*
- **Benign prostatic hyperplasia (BPH)** is not a risk factor for abdominal aortic aneurysm formation or rupture.
- It is a condition of the prostate gland causing urinary symptoms and has no pathophysiological link to aortic disease.
*Obesity*
- While **obesity** is a risk factor for many cardiovascular diseases, its association with **abdominal aortic aneurysms (AAAs)** is less direct than other factors, often mediated through related conditions like hypertension.
- Some studies suggest a **protective effect** or no significant association between obesity and AAA, although this remains an area of ongoing research.
*Diabetes*
- **Diabetes** is generally considered to have a **paradoxical or even protective effect** against the development of **abdominal aortic aneurysms (AAAs)**, although it significantly increases the risk of other vascular complications.
- The exact mechanism is not fully understood but may involve changes in the aortic wall's structural properties or reduced inflammation in diabetic patients with AAAs.
*Alcohol consumption*
- **Moderate alcohol consumption** has not been consistently linked to an increased risk of **abdominal aortic aneurysms (AAAs)**.
- **Excessive alcohol consumption** can contribute to overall cardiovascular disease risk, but it is not identified as a primary or strong independent risk factor for AAA formation or rupture.
Great vessels and lymphatics US Medical PG Question 7: A 69-year-old smoker presents to physician after noticing that his face seems to be more swollen than usual. Upon further questioning, he reports increasing shortness of breath and cough over the past 6 months. On exam, his physician notices venous distention in his neck and distended veins in the upper chest and arms. Chest radiograph shows a right upper lobe mass. What is the embryologic origin of the vessel being compressed by this patient's tumor?
- A. Cardinal veins (Correct Answer)
- B. Primitive ventricle
- C. Left horn of sinus venosus
- D. Truncus arteriosus
- E. Bulbus cordis
Great vessels and lymphatics Explanation: ***Cardinal veins***
- The symptoms of facial swelling, neck vein distention, and upper chest/arm vein distention, especially with a right upper lobe mass, are classic for **superior vena cava (SVC) syndrome**.
- The **SVC** is formed from the fusion of the anterior **cardinal veins**, which drain the upper body during embryonic development.
*Primitive ventricle*
- The **primitive ventricle** develops into parts of the left and right **ventricles** of the heart.
- It is not directly involved in the formation of major systemic veins like the SVC.
*Left horn of sinus venosus*
- The **left horn of the sinus venosus** mostly regresses and contributes to structures like the **coronary sinus** and the oblique vein of the left atrium.
- It does not form the SVC, which drains the upper body.
*Truncus arteriosus*
- The **truncus arteriosus** is an embryonic structure that separates to form the **aorta** and the **pulmonary artery**.
- It is an arterial structure, not a venous structure that would be compressed in SVC syndrome.
*Bulbus cordis*
- The **bulbus cordis** develops into the **conus arteriosus** (infundibulum) of the right ventricle and the **aortic vestibule** of the left ventricle.
- Like the truncus arteriosus, it is involved in arterial outflow tracts and not the formation of the SVC.
Great vessels and lymphatics US Medical PG Question 8: A 50-year-old man presents with severe chest pain for a week. His pain increases with breathing and is localized to the right. He has tried over-the-counter medications at home, but they did not help. The patient has a 20-pack-year smoking history and currently smokes 2 packs of cigarettes daily, and he drinks 3 to 4 cans of beer daily before dinner. His temperature is 39.1°C (102.3°F), blood pressure is 127/85 mm Hg, pulse is 109/min, and respirations are 20/min. Respiratory examination shows dullness to percussion from the 7th rib inferiorly at the right midaxillary line, decreased vocal tactile fremitus, and diminished breath sounds in the same area. Chest radiograph is shown in the image. The patient is prepared for thoracocentesis. Which of the following locations would be the most appropriate for insertion of a chest tube?
- A. Below the inferior border of the 7th rib in the midaxillary line
- B. Above the superior border of the 8th rib in the midaxillary line (Correct Answer)
- C. Above the superior border of the 5th rib in the midclavicular line
- D. Below the inferior border of the 5th rib in the midaxillary line
- E. Above the superior border of the 7th rib in the midclavicular line
Great vessels and lymphatics Explanation: ***Above the superior border of the 8th rib in the midaxillary line***
- The patient presents with symptoms and signs suggestive of a **pleural effusion** (dullness to percussion, decreased fremitus, diminished breath sounds) and potentially an **empyema** given the fever and lung consolidation on the radiograph.
- Thoracocentesis should be performed in the **midaxillary line** between the 6th and 9th ribs to avoid injuring the **diaphragm and abdominal organs**, which can rise as high as the 5th intercostal space during expiration. To prevent damage to the neurovascular bundle that runs along the inferior border of the ribs, the needle should be inserted just **above the superior border** of the rib below the chosen intercostal space.
*Below the inferior border of the 7th rib in the midaxillary line*
- Inserting below the inferior border of the 7th rib increases the risk of injuring the **neurovascular bundle** that runs along the inferior rib margin.
- Such placement might also be too low, increasing the risk of penetrating the **diaphragm** or **abdominal organs**. This location would correspond to the 8th intercostal space, but the 'below inferior border' part is incorrect.
*Above the superior border of the 5th rib in the midclavicular line*
- The **midclavicular line** is typically used for needle decompression of a tension pneumothorax (2nd intercostal space) but is not the preferred site for thoracocentesis due to the risk of striking the lung parenchyma or internal mammary artery.
- Even if considering a pneumothorax, the 5th intercostal space in the midclavicular line is not the standard site, and an effusion is indicated here.
*Below the inferior border of the 5th rib in the midaxillary line*
- Inserting below the inferior border of the 5th rib, similar to option A, risks injury to the **neurovascular bundle**.
- While in the midaxillary line, the 5th rib might be too high for an effusion, and the technique of inserting below the inferior border is incorrect.
*Above the superior border of the 7th rib in the midclavicular line*
- The **midclavicular line** is generally avoided for thoracocentesis of effusions due to the risks mentioned previously and poor drainage if the effusion is posterior.
- The 7th intercostal space in the midclavicular line is also a non-standard and less safe location for this procedure.
Great vessels and lymphatics US Medical PG Question 9: A researcher is investigating the blood supply of the adrenal gland. While performing an autopsy on a patient who died from unrelated causes, he identifies a vessel that supplies oxygenated blood to the inferior aspect of the right adrenal gland. Which of the following vessels most likely gave rise to the vessel in question?
- A. Inferior phrenic artery
- B. Abdominal aorta
- C. Renal artery (Correct Answer)
- D. Superior mesenteric artery
- E. Common iliac artery
Great vessels and lymphatics Explanation: ***Renal artery***
- The **inferior suprarenal artery**, which supplies the inferior part of the adrenal gland, typically arises from the **renal artery**.
- The adrenal glands receive a rich blood supply from three main arterial sources: superior, middle, and inferior suprarenal arteries.
*Inferior phrenic artery*
- The **superior suprarenal arteries** typically arise from the **inferior phrenic arteries** and supply the superior aspect of the adrenal glands.
- While critical for adrenal blood supply, they do not typically contribute to the inferior aspect directly.
*Abdominal aorta*
- The **middle suprarenal artery** usually arises directly from the **abdominal aorta**.
- This vessel supplies the central part of the adrenal gland, but not primarily the inferior aspect.
*Superior mesenteric artery*
- The **superior mesenteric artery** primarily supplies structures of the midgut (e.g., small intestine, ascending colon) and does not typically give rise to vessels supplying the adrenal glands.
- It is located inferior to the origin of the renal arteries and the adrenal glands.
*Common iliac artery*
- The **common iliac arteries** supply the lower limbs and pelvic organs, originating from the abdominal aorta bifurcation.
- These arteries are located much too far inferior to supply the adrenal glands, which are retroperitoneal structures in the upper abdomen.
Great vessels and lymphatics US Medical PG Question 10: A 65-year-old man presents to the emergency department with abdominal pain and a pulsatile abdominal mass. Further examination of the mass shows that it is an abdominal aortic aneurysm. A computed tomography scan with contrast reveals an incidental finding of a horseshoe kidney, and the surgeon is informed of this finding prior to operating on the aneurysm. Which of the following may complicate the surgical approach in this patient?
- A. Anomalous origins of multiple renal arteries (Correct Answer)
- B. Low glomerular filtration rate due to unilateral renal agenesis
- C. Proximity of the fused kidney to the celiac artery
- D. Abnormal relationship between the kidney and the superior mesenteric artery
- E. There are no additional complications
Great vessels and lymphatics Explanation: ***Anomalous origins of multiple renal arteries***
- A horseshoe kidney often receives its blood supply from **multiple renal arteries** arising anomalously from the aorta, iliac arteries, or inferior mesenteric artery.
- These aberrant vessels can cross the surgical field and complicate **abdominal aortic aneurysm repair**, increasing the risk of injury and hemorrhage.
*Low glomerular filtration rate due to unilateral renal agenesis*
- This patient has a **horseshoe kidney**, which involves fused kidneys, not renal agenesis (absence of a kidney).
- While chronic kidney disease can be associated with horseshoe kidneys, **unilateral agenesis** is a distinct condition and not described in this scenario.
*Proximity of the fused kidney to the celiac artery*
- The fused portion of a horseshoe kidney (the **isthmus**) typically lies anterior to the great vessels at the L3-L5 vertebral level, below the origin of the celiac artery.
- Therefore, its proximity to the **celiac artery** is generally not the primary surgical concern during abdominal aortic aneurysm repair.
*Abnormal relationship between the kidney and the superior mesenteric artery*
- The superior mesenteric artery typically originates from the aorta above the level of the horseshoe kidney's isthmus.
- While other anomalies can exist, an **abnormal relationship** between the kidney and the superior mesenteric artery is not a classic or primary complication of horseshoe kidney during AAA repair.
*There are no additional complications*
- The presence of a horseshoe kidney significantly increases the complexity of **abdominal aortic aneurysm** surgery.
- The potential for **vascular anomalies** and altered anatomical relationships makes this statement incorrect, as there are definite additional surgical considerations.
More Great vessels and lymphatics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.