GI tract anatomy (esophagus to rectum) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GI tract anatomy (esophagus to rectum). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GI tract anatomy (esophagus to rectum) US Medical PG Question 1: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
GI tract anatomy (esophagus to rectum) Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
GI tract anatomy (esophagus to rectum) US Medical PG Question 2: A 40-year-old man presents with severe fatigue, dyspnea on exertion, and weight loss. He reports a weight loss of 15 kg (33.0 lb) over the past 3 months and feels full almost immediately after starting to eat, often feeling nauseous and occasionally vomiting. Past medical history is not significant. However, the patient reports a 10-pack-year smoking history. His temperature is 37.0°C (98.6°F), respiratory rate is 15/min, pulse is 67/min, and blood pressure is 122/98 mm Hg. Physical examination reveals paleness and conjunctival pallor. Abdominal examination reveals an ill-defined nontender mass in the epigastric region along with significant hepatomegaly. Routine laboratory studies show a hemoglobin level of 7.2 g/dL. A contrast CT scan of the abdomen is presented below. Which of the following structures is most helpful in the anatomical classification of gastrointestinal bleeding in this patient?
- A. Ampulla of Vater
- B. Hepatoduodenal ligament
- C. Ligament of Treitz (Correct Answer)
- D. Portal vein
- E. Sphincter of Oddi
GI tract anatomy (esophagus to rectum) Explanation: ***Ligament of Treitz***
- The **ligament of Treitz** is a key anatomical landmark that divides the gastrointestinal tract into the upper and lower GI systems.
- Bleeding proximal to this ligament is considered **upper GI bleeding**, while bleeding distal to it is **lower GI bleeding**. This distinction helps narrow down potential causes and guide diagnostic procedures.
*Ampulla of Vater*
- The **Ampulla of Vater** is the junction of the common bile duct and pancreatic duct, emptying into the second part of the duodenum.
- While it can be a source of bleeding (e.g., from an eroded tumor or bleeding peptic ulcer), it is within the upper GI tract and does not serve as a primary dividing line for anatomical classification of GI bleeding as a whole.
*Hepatoduodenal ligament*
- The **hepatoduodenal ligament** contains the portal triad (hepatic artery, portal vein, and common bile duct).
- It does not serve as an anatomical landmark for classifying GI bleeding into upper and lower components.
*Portal vein*
- The **portal vein** carries blood from the GI tract and spleen to the liver.
- It is involved in conditions that can cause GI bleeding (e.g., portal hypertension leading to varices), but it is a blood vessel and not a structural landmark for classifying bleeding into upper vs. lower GI.
*Sphincter of Oddi*
- The **Sphincter of Oddi** controls the flow of bile and pancreatic secretions into the duodenum at the Ampulla of Vater.
- Like the Ampulla of Vater, it is an upper GI structure and does not provide an anatomical classification for differentiating between upper and lower GI bleeding.
GI tract anatomy (esophagus to rectum) US Medical PG Question 3: A 69-year-old man presents with progressive dysphagia and a 5-kg weight loss over 3 months. Initially, he had difficulty swallowing solids, which progressed to include liquids in the past week. Endoscopy reveals a mass 3 cm proximal to the esophagogastric junction. Biopsy shows significant distortion of glandular architecture, consistent with adenocarcinoma. Which of the following is the strongest risk factor for this patient's likely diagnosis?
- A. Chronic alcohol use
- B. Visceral obesity (Correct Answer)
- C. Consumption of hot liquids
- D. Chewing of betel nuts
- E. Consumption of cured meats
GI tract anatomy (esophagus to rectum) Explanation: ***Visceral obesity***
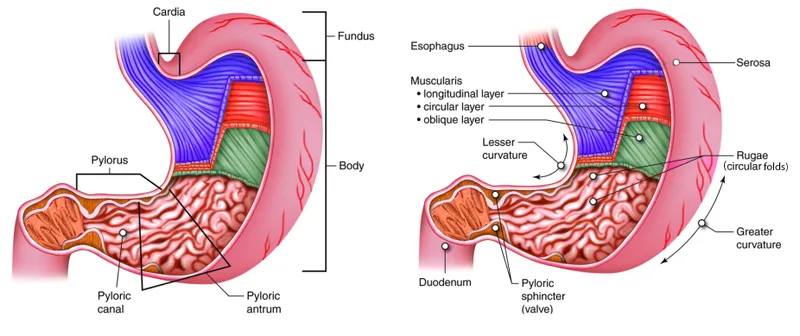
- The patient's presentation of dysphagia becoming progressively worse from solids to liquids, along with significant weight loss and an **esophagogastric junction (EGJ)** adenocarcinoma, strongly points to **esophageal adenocarcinoma**.
- **Visceral obesity** is a major risk factor for gastroesophageal reflux disease (GERD) and **Barrett's esophagus**, which are precursors to **EGJ adenocarcinoma**.
*Chronic alcohol use*
- While chronic alcohol use is a significant risk factor for **squamous cell carcinoma** of the esophagus, it is not as strongly linked to **adenocarcinoma**, especially at the EGJ.
- The patient's cancer location (3 cm proximal to EGJ) and histological type (**adenocarcinoma**) make alcohol a less likely primary risk factor compared to other options.
*Consumption of hot liquids*
- Consumption of very **hot liquids** is a known risk factor for **squamous cell carcinoma** of the esophagus, particularly in the mid and upper esophagus.
- It is not a primary risk factor for **adenocarcinoma** occurring at the esophagogastric junction.
*Chewing of betel nuts*
- **Betel nut chewing** is strongly associated with an increased risk of **oral cancer** (squamous cell carcinoma of the oral cavity and pharynx) and to a lesser extent **esophageal squamous cell carcinoma**.
- It is not considered a significant risk factor for **esophageal adenocarcinoma**.
*Consumption of cured meats*
- High intake of **cured and processed meats** has been associated with an increased risk of several gastrointestinal cancers, particularly **gastric cancer** and **colorectal cancer**.
- Its association with **esophageal adenocarcinoma** is not as strong or direct as that of visceral obesity and GERD.
GI tract anatomy (esophagus to rectum) US Medical PG Question 4: A 24-year-old woman comes to the emergency department because of abdominal pain, fever, nausea, and vomiting for 12 hours. Her abdominal pain was initially dull and diffuse but has progressed to a sharp pain on the lower right side. Two years ago she had to undergo right salpingo-oophorectomy after an ectopic pregnancy. Her temperature is 38.7°C (101.7°F). Physical examination shows severe right lower quadrant tenderness with rebound tenderness; bowel sounds are decreased. Laboratory studies show leukocytosis with left shift. An abdominal CT scan shows a distended, edematous appendix. The patient is taken to the operating room for an appendectomy. During the surgery, the adhesions from the patient's previous surgery make it difficult for the resident physician to identify the appendix. Her attending mentions that she should use a certain structure for guidance to locate the appendix. The attending is most likely referring to which of the following structures?
- A. Epiploic appendages
- B. Right ureter
- C. Deep inguinal ring
- D. Ileocolic artery
- E. Teniae coli (Correct Answer)
GI tract anatomy (esophagus to rectum) Explanation: ***Teniae coli***
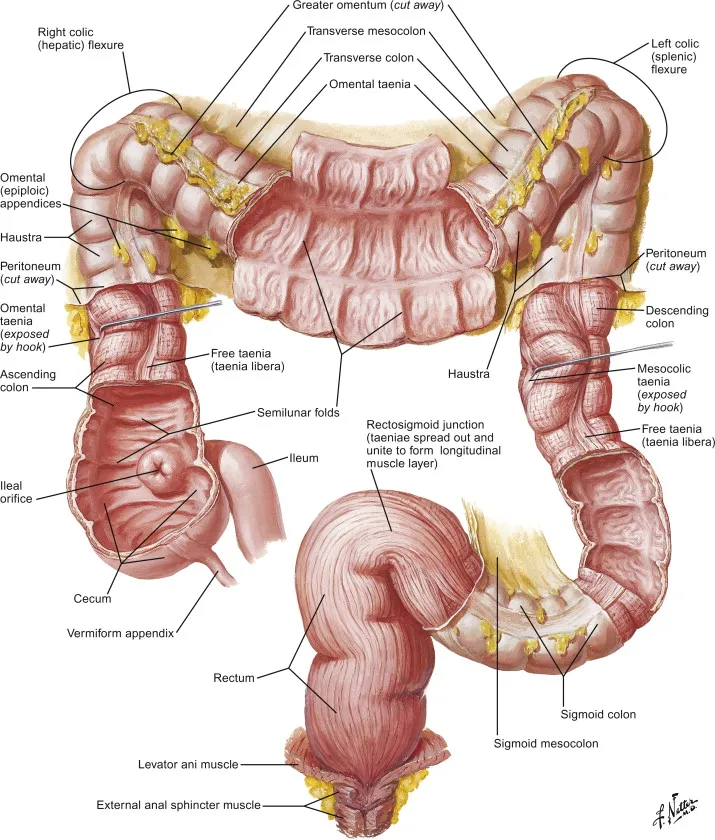
- The **teniae coli** are three distinct longitudinal bands of smooth muscle that run along the length of the cecum and colon, converging at the base of the **appendix**.
- Following these bands inferiorly from the ascending colon or cecum during surgery is a reliable method to locate the **vermiform appendix**, especially in the presence of adhesions.
*Epiploic appendages*
- These are small, fat-filled sacs that protrude from the surface of the **large intestine** but are not directly used as a reliable landmark for locating the appendix.
- While present in the vicinity, they do not consistently lead to the base of the appendix like the teniae coli.
*Right ureter*
- The **right ureter** is located retroperitoneally, deep to the cecum and appendix, and is not a direct anatomical landmark used for identifying the appendix during an appendectomy.
- Identifying the ureter is important to avoid injury, but not for localizing the appendix.
*Deep inguinal ring*
- The **deep inguinal ring** is an opening in the transversalis fascia, involved in the formation of the inguinal canal, and is located far anterior and inferior to the region of the appendix.
- It has no anatomical relationship that would guide a surgeon to locate the appendix.
*Ileocolic artery*
- The **ileocolic artery** branches from the superior mesenteric artery and supplies the terminal ileum, cecum, and appendix. While it provides blood supply to the appendix, it is not a direct or consistent surface landmark for locating the appendix itself, especially in complex cases with adhesions.
- Locating the artery would be more complex and less reliable for initial identification compared to the teniae coli.
GI tract anatomy (esophagus to rectum) US Medical PG Question 5: A 75-year-old man presents to the clinic for chronic fatigue of 3 months duration. Past medical history is significant for type 2 diabetes and hypertension, both of which are controlled with medications, as well as constipation. He denies any fever, weight loss, pain, or focal neurologic deficits. A complete blood count reveals microcytic anemia, and a stool guaiac test is positive for blood. He is subsequently evaluated with a colonoscopy. The physician notes some “small pouches” in the colon despite poor visualization due to inadequate bowel prep. What is the blood vessel that supplies the area with the above findings?
- A. Ileocolic artery
- B. Superior mesenteric artery
- C. Inferior mesenteric artery (Correct Answer)
- D. Middle colic artery
- E. Right colic artery
GI tract anatomy (esophagus to rectum) Explanation: ***Inferior mesenteric artery***
- The patient's **microcytic anemia** and **positive stool guaiac test** indicate chronic gastrointestinal blood loss, highly suggestive of **diverticulosis** presenting as "small pouches" in the colon.
- Diverticulosis commonly affects the **descending colon** and **sigmoid colon**, which are primarily supplied by branches of the **inferior mesenteric artery**.
*Ileocolic artery*
- The ileocolic artery is a branch of the **superior mesenteric artery** and supplies the **ileum**, **cecum**, and **ascending colon**.
- Diverticula are less commonly found in these regions compared to the left colon.
*Superior mesenteric artery*
- The superior mesenteric artery supplies the **midgut derivatives**, including the **small intestine** and the **right half of the large intestine** (up to the distal transverse colon).
- While it supplies a large portion of the GI tract, the typical location of diverticulosis (descending and sigmoid colon) is outside its primary distribution.
*Middle colic artery*
- The middle colic artery is a branch of the **superior mesenteric artery** and supplies the **transverse colon**.
- While diverticula can occur in the transverse colon, it is not the most common location, and the inferior mesenteric artery supplies the areas most frequently affected.
*Right colic artery*
- The right colic artery is a branch of the **superior mesenteric artery** and supplies the **ascending colon**.
- Diverticula are less frequently found in the ascending colon compared to the descending and sigmoid colon.
GI tract anatomy (esophagus to rectum) US Medical PG Question 6: A 65-year-old woman with atrial fibrillation comes to the emergency department because of sudden-onset severe abdominal pain, nausea, and vomiting for the past 2 hours. She has smoked a pack of cigarettes daily for the past 25 years. Her pulse is 110/min and blood pressure is 141/98 mm Hg. Abdominal examination shows diffuse abdominal tenderness without guarding or rebound. A CT angiogram of the abdomen confirms an acute occlusion in the inferior mesenteric artery. Which of the following structures of the gastrointestinal tract is most likely to be affected in this patient?
- A. Hepatic flexure
- B. Rectosigmoid colon (Correct Answer)
- C. Ascending colon
- D. Transverse colon
- E. Lower rectum
GI tract anatomy (esophagus to rectum) Explanation: ***Rectosigmoid colon***
- The **inferior mesenteric artery (IMA)** supplies the distal third of the transverse colon, descending colon, sigmoid colon, and superior part of the rectum, which includes the **rectosigmoid colon**.
- The **rectosigmoid region** is entirely dependent on IMA branches (sigmoid arteries and superior rectal artery) and represents a classic watershed area vulnerable to ischemia.
- An occlusion in the IMA would compromise blood flow to these structures, leading to ischemia and symptoms like severe abdominal pain, bloody diarrhea, and peritoneal signs.
*Hepatic flexure*
- The **hepatic flexure** is primarily supplied by branches of the **superior mesenteric artery (SMA)**, specifically the middle colic artery.
- An occlusion in the IMA would generally spare the hepatic flexure, as its blood supply comes from a different major arterial system.
*Ascending colon*
- The **ascending colon** receives its blood supply from the **superior mesenteric artery (SMA)** via the ileocolic and right colic arteries.
- Therefore, an occlusion in the IMA would not directly affect the blood supply to the ascending colon.
*Transverse colon*
- While the **IMA** supplies the **distal one-third of the transverse colon** via the left colic artery, the term "transverse colon" as an anatomical structure includes both IMA and SMA territories.
- The proximal two-thirds are supplied by the **superior mesenteric artery (SMA)** via the middle colic artery, with robust collateral circulation through the marginal artery of Drummond.
- The rectosigmoid colon is the more specific and entirely IMA-dependent structure, making it the most likely to be affected.
*Lower rectum*
- The **lower rectum** receives its blood supply primarily from the **internal iliac arteries** via the middle and inferior rectal arteries.
- The IMA supplies the superior part of the rectum, but the lower rectum has a separate and robust blood supply, making it less likely to be affected by an isolated IMA occlusion.
GI tract anatomy (esophagus to rectum) US Medical PG Question 7: A 36-year-old man undergoes ileocecal resection after a gunshot injury. The resected ileocecal segment is sent for histological evaluation. One of the slides derived from the specimen is shown in the image. Which of the following statements regarding the structure marked within the red circle is correct?
- A. This structure can be only found in the colon.
- B. These structures mostly contain M-cells.
- C. This structure can become a site of entry of certain microorganisms including S. typhi. (Correct Answer)
- D. This structure only appears in case of bacterial infection.
- E. Infants have the largest amount of these structures within their intestinal wall.
GI tract anatomy (esophagus to rectum) Explanation: ***This structure can become a site of entry of certain microorganisms including S. typhi.***
- The image illustrates **Peyer's patches**, which are lymphoid follicles found primarily in the ileum. These structures are rich in **M-cells**, which sample antigens from the intestinal lumen.
- While M-cells are crucial for initiating immune responses, some pathogens like *Salmonella typhi* exploit them to **translocate across the intestinal barrier** and disseminate, leading to systemic infection.
*This structure can be only found in the colon.*
- The structure shown is a **Peyer's patch**, which is predominantly found in the **ileum** of the small intestine, not exclusively in the colon.
- While lymphoid tissue is present throughout the GI tract, these large aggregated lymphoid nodules are characteristic of the ileum.
*These structures mostly contain M-cells.*
- While **M-cells (microfold cells)** are indeed present in the dome epithelium overlying Peyer's patches and are critical for antigen sampling, they constitute a minority of the cells within the entire structure.
- The bulk of Peyer's patches consists of **lymphocytes** (B cells, T cells), macrophages, and dendritic cells, forming lymphoid follicles and interfollicular areas.
*This structure only appears in case of bacterial infection.*
- **Peyer's patches** are a normal and permanent component of the gut-associated lymphoid tissue (GALT) and are present in healthy individuals.
- They serve as crucial sites for **immune surveillance** and the induction of adaptive immune responses to both commensal bacteria and pathogens, even in the absence of an active infection.
*Infants have the largest amount of these structures within their intestinal wall.*
- Peyer's patches are **well-developed at birth** and continue to increase in size and number during childhood and adolescence.
- They tend to **atrophy with age**, meaning that young adults and adolescents typically have the most prominent and numerous Peyer's patches, not infants.
GI tract anatomy (esophagus to rectum) US Medical PG Question 8: A researcher is investigating the blood supply of the adrenal gland. While performing an autopsy on a patient who died from unrelated causes, he identifies a vessel that supplies oxygenated blood to the inferior aspect of the right adrenal gland. Which of the following vessels most likely gave rise to the vessel in question?
- A. Inferior phrenic artery
- B. Abdominal aorta
- C. Renal artery (Correct Answer)
- D. Superior mesenteric artery
- E. Common iliac artery
GI tract anatomy (esophagus to rectum) Explanation: ***Renal artery***
- The **inferior suprarenal artery**, which supplies the inferior part of the adrenal gland, typically arises from the **renal artery**.
- The adrenal glands receive a rich blood supply from three main arterial sources: superior, middle, and inferior suprarenal arteries.
*Inferior phrenic artery*
- The **superior suprarenal arteries** typically arise from the **inferior phrenic arteries** and supply the superior aspect of the adrenal glands.
- While critical for adrenal blood supply, they do not typically contribute to the inferior aspect directly.
*Abdominal aorta*
- The **middle suprarenal artery** usually arises directly from the **abdominal aorta**.
- This vessel supplies the central part of the adrenal gland, but not primarily the inferior aspect.
*Superior mesenteric artery*
- The **superior mesenteric artery** primarily supplies structures of the midgut (e.g., small intestine, ascending colon) and does not typically give rise to vessels supplying the adrenal glands.
- It is located inferior to the origin of the renal arteries and the adrenal glands.
*Common iliac artery*
- The **common iliac arteries** supply the lower limbs and pelvic organs, originating from the abdominal aorta bifurcation.
- These arteries are located much too far inferior to supply the adrenal glands, which are retroperitoneal structures in the upper abdomen.
GI tract anatomy (esophagus to rectum) US Medical PG Question 9: A 48-year-old Caucasian woman presents to her primary care provider complaining about difficulties while swallowing with fatigability and occasional palpitations for the past few weeks. Her personal history is relevant for bariatric surgery a year ago and a long list of allergies which includes peanuts, penicillin, and milk protein. Physical examination is unremarkable except for pale skin and mucosal surfaces, koilonychia, and glossitis. Which of the following descriptions would you expect to find in an endoscopy?
- A. Luminal protruding concentric diaphragms (Correct Answer)
- B. Luminal eccentric membranes
- C. Changes in the epithelial lining of the esophagus
- D. Hiatus hernia
- E. Pharyngeal pouch
GI tract anatomy (esophagus to rectum) Explanation: The patient's symptoms (dysphagia, fatigue, palpitations, pallor, koilonychia, glossitis) and history of bariatric surgery strongly suggest iron deficiency anemia. In a subpopulation of patients with iron deficiency anemia, particularly women, a rare complication known as Plummer-Vinson syndrome (also known as Paterson-Kelly syndrome or sideropenic dysphagia) can develop, which is characterized by the presence of esophageal webs. These webs appear as concentric diaphragms on endoscopy.
*Luminal eccentric membranes*
- This typically refers to Schatzki rings, which are mucosal rings at the gastroesophageal junction. While they cause dysphagia, they are usually eccentric or asymmetric, and not typically described as concentric diaphragms. Schatzki rings are often associated with hiatal hernias and are not usually a direct sequela of iron deficiency anemia [1].
*Changes in the epithelial lining of the esophagus*
- This is a very general description and could refer to various conditions such as esophagitis, Barrett's esophagus, or Candida esophagitis.
*Hiatus hernia*
- A hiatus hernia involves the protrusion of the stomach into the thorax through the esophageal hiatus [1]. While it can cause dysphagia and is common, it does not directly explain the other specific symptoms like koilonychia and glossitis, nor is it a direct consequence of iron deficiency anemia in this clinical picture. Endoscopically, a hiatus hernia appears as a widening of the diaphragmatic hiatus and upward displacement of the gastric cardia, not luminal diaphragms.
*Pharyngeal pouch*
- A pharyngeal pouch (Zenker's diverticulum) is an outpouching of the posterior pharyngeal wall, typically causing dysphagia, regurgitation of undigested food, and halitosis [2]. It would be located higher in the pharynx, not in the esophagus, and would appear as a diverticulum, not a concentric diaphragm. It is not associated with the signs of iron deficiency noted.
GI tract anatomy (esophagus to rectum) US Medical PG Question 10: A 72-year-old male with a past medical history significant for aortic stenosis and hypertension presents to the emergency department complaining of weakness for the past 3 weeks. He states that, apart from feeling weaker, he also has noted lightheadedness, pallor, and blood-streaked stools. The patient's vital signs are stable, and he is in no acute distress. Laboratory workup reveals that the patient is anemic. Fecal occult blood test is positive for bleeding. EGD was performed and did not reveal upper GI bleeding. Suspecting a lower GI bleed, a colonoscopy is performed after prepping the patient, and it is unremarkable. What would be an appropriate next step for localizing a lower GI bleed in this patient?
- A. Technetium-99 labelled erythrocyte scintigraphy (Correct Answer)
- B. Flexible sigmoidoscopy
- C. Nasogastric tube lavage
- D. Ultrasound of the abdomen
- E. CT of the abdomen
GI tract anatomy (esophagus to rectum) Explanation: ***Technetium-99 labelled erythrocyte scintigraphy***
- This test can detect **slow-rate lower GI bleeds** (as low as 0.2-0.5 mL/min) that may be missed by endoscopy or colonoscopy, especially when the bleeding is intermittent or subtle.
- Given the **negative EGD** and **unremarkable colonoscopy** despite evidence of an ongoing lower GI bleed, this nuclear medicine study is appropriate for localization.
- Particularly useful in this patient with **aortic stenosis**, where angiodysplasia (vascular malformations, often in the small bowel) is a common cause of obscure GI bleeding (Heyde's syndrome).
*Flexible sigmoidoscopy*
- This procedure only visualizes the **rectum and a portion of the sigmoid colon**, which is insufficient given the negative full colonoscopy.
- It would not provide any new information for localizing a bleed that has already been ruled out from the accessible colon.
*Nasogastric tube lavage*
- This procedure is used to assess for **upper GI bleeding** by checking for blood in the gastric contents.
- The EGD already ruled out an upper GI bleed, making this step unnecessary and unhelpful for a suspected lower GI source.
*Ultrasound of the abdomen*
- Abdominal ultrasound is primarily used to evaluate **solid organs** (e.g., liver, gallbladder, kidneys) and potential fluid collections.
- It is generally **not effective** for localizing or diagnosing the source of active GI bleeding.
*CT of the abdomen*
- A standard CT abdomen without specialized imaging protocol has **limited sensitivity** for detecting the source of GI bleeding.
- While **CT angiography** (a different test with IV contrast timed to arterial phase) can detect active bleeding at rates >0.3-0.5 mL/min, a routine "CT of the abdomen" as listed in this option would not be adequate for localizing occult GI bleeding.
More GI tract anatomy (esophagus to rectum) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.