Upper limb surface landmarks US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Upper limb surface landmarks. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Upper limb surface landmarks US Medical PG Question 1: A 16-year-old boy is brought to the emergency department after being tackled at a football game. Per his mom, he is the quarterback of his team and was head-butted in the left shoulder region by the opposing team. Shortly after, the mother noticed that his left arm was hanging by his torso and his hand was “bent backwards and facing the sky.” The patient denies head trauma, loss of consciousness, sensory changes, or gross bleeding. A physical examination demonstrates weakness in abduction, lateral rotation, flexion, and supination of the left arm and tenderness of the left shoulder region with moderate bruising. Radiograph of the left shoulder and arm is unremarkable. Which of the following is most likely damaged in this patient?
- A. C5-C6 nerve roots (Correct Answer)
- B. Ulnar nerve
- C. C8-T1 nerve roots
- D. Long thoracic nerve
Upper limb surface landmarks Explanation: ***C5-C6 nerve roots***
- The "bent backwards and facing the sky" hand posture indicates **Waiter's tip position**, a classic sign of **Erb-Duchenne palsy**, caused by damage to the upper trunk of the brachial plexus (C5-C6 roots) [1].
- Weakness in **abduction** (deltoid, supraspinatus), **lateral rotation** (infraspinatus, teres minor), **flexion** (biceps, coracobrachialis), and **supination** (biceps, supinator) are all consistent with C5-C6 nerve root involvement.
*Ulnar nerve*
- Ulnar nerve damage would result in a **claw hand deformity** (hyperextension of MCP joints and flexion of DIP/PIP joints of 4th and 5th digits) and weakness in intrinsic hand muscles, not the observed upper arm weakness.
- Sensory loss involves the medial hand and little finger.
*C8-T1 nerve roots*
- Damage to the C8-T1 nerve roots (lower trunk) typically results in **Klumpke's palsy**, characterized by a more severe **claw hand** and paralysis of intrinsic hand muscles [1].
- This presentation does not match the observed functional deficits.
*Long thoracic nerve*
- Injury to the long thoracic nerve causes paralysis of the **serratus anterior muscle**, leading to **scapular winging**, especially when pushing against a wall.
- While possible in shoulder trauma, it does not explain the widespread weakness in abduction, rotation, flexion, and supination of the arm.
Upper limb surface landmarks US Medical PG Question 2: A 60-year-old woman is rushed to the emergency room after falling on her right elbow while walking down the stairs. She cannot raise her right arm. Her vital signs are stable, and the physical examination reveals loss of sensation over the upper lateral aspect of the right arm and shoulder. A radiologic evaluation shows a fracture of the surgical neck of the right humerus. Which of the following muscles is supplied by the nerve that is most likely damaged?
- A. Teres minor (Correct Answer)
- B. Teres major
- C. Subscapularis
- D. Infraspinatus
- E. Supraspinatus
Upper limb surface landmarks Explanation: ***Teres minor***
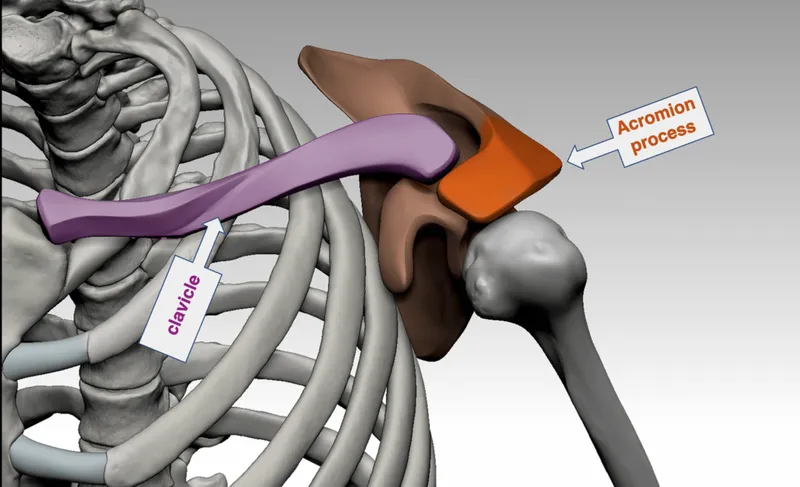
- A fracture of the **surgical neck of the humerus** often damages the **axillary nerve**, which innervates the **teres minor**.
- The axillary nerve also supplies the **deltoid muscle** and provides cutaneous sensation to the **upper lateral arm**, consistent with the patient's sensory loss.
*Teres major*
- This muscle is innervated by the **lower subscapular nerve**, which is less likely to be damaged in a surgical neck fracture.
- Its primary action is **adduction** and **internal rotation** of the arm.
*Subscapularis*
- The **subscapularis** is innervated by the **upper and lower subscapular nerves**.
- While it contributes to internal rotation, its nerve supply is typically protected in this type of fracture.
*Infraspinatus*
- The **infraspinatus** muscle is innervated by the **suprascapular nerve**.
- This nerve is generally not affected by a fracture of the surgical neck of the humerus.
*Supraspinatus*
- Similar to the infraspinatus, the **supraspinatus** is also innervated by the **suprascapular nerve**.
- Damage to this nerve due to a humeral surgical neck fracture is uncommon.
Upper limb surface landmarks US Medical PG Question 3: A 61-year-old woman comes to the physician for a follow-up examination 1 week after undergoing right-sided radical mastectomy and axillary lymph node dissection for breast cancer. She says that she has been unable to comb her hair with her right hand since the surgery. Physical examination shows shoulder asymmetry. She is unable to abduct her right arm above 90 degrees. When she pushes against a wall, there is protrusion of the medial aspect of the right scapula. Injury to which of the following nerves is the most likely cause of this patient's condition?
- A. Long thoracic nerve (Correct Answer)
- B. Thoracodorsal nerve
- C. Axillary nerve
- D. Suprascapular nerve
- E. Upper trunk of the brachial plexus
Upper limb surface landmarks Explanation: ***Long thoracic nerve***
- Injury to the **long thoracic nerve** leads to paralysis of the **serratus anterior muscle**, causing **scapular winging** (protrusion of the medial scapula) especially when pushing against a wall.
- The serratus anterior is crucial for **scapular protraction** and stabilizing the scapula during **abduction of the arm above 90 degrees**, explaining her inability to comb her hair.
*Thoracodorsal nerve*
- The **thoracodorsal nerve** innervates the **latissimus dorsi muscle**, which is responsible for **adduction**, extension, and internal rotation of the arm.
- Injury to this nerve would primarily affect these movements, not shoulder abduction above 90 degrees or scapular winging.
*Axillary nerve*
- The **axillary nerve** innervates the **deltoid muscle** and **teres minor**.
- Damage would primarily result in impaired **arm abduction up to 90 degrees** and loss of sensation over the lateral shoulder, but not scapular winging.
*Suprascapular nerve*
- The **suprascapular nerve** supplies the **supraspinatus** and **infraspinatus muscles**, which are involved in the initiation of arm abduction and external rotation, respectively.
- Injury would cause weakness in these movements and shoulder pain, but not scapular winging.
*Upper trunk of the brachial plexus*
- Injury to the **upper trunk of the brachial plexus** (C5-C6) affects several nerves and muscles, leading to conditions like **Erb's palsy**.
- While it can impair shoulder function and abduction, the specific finding of scapular winging points more directly to long thoracic nerve damage rather than a generalized upper trunk injury, as the long thoracic nerve (C5-C7) is often spared in classic Erb's palsy.
Upper limb surface landmarks US Medical PG Question 4: A 23-year-old college student was playing basketball when he fell directly onto his left elbow. He had sudden, intense pain and was unable to move his elbow. He was taken immediately to the emergency room by his teammates. He has no prior history of trauma or any chronic medical conditions. His blood pressure is 128/84 mm Hg, the heart rate is 92/min, and the respiratory rate is 14/min. He is in moderate distress and is holding onto his left elbow. On physical examination, pinprick sensation is absent in the left 5th digit and the medial aspect of the left 4th digit. Which of the following is the most likely etiology of this patient’s condition?
- A. Axillary neuropathy
- B. Median neuropathy
- C. Radial neuropathy
- D. Musculocutaneous neuropathy
- E. Ulnar neuropathy (Correct Answer)
Upper limb surface landmarks Explanation: ***Ulnar neuropathy***
- Direct trauma to the elbow, combined with **pinprick sensation loss** in the **5th digit** and the **medial aspect of the 4th digit**, is highly indicative of **ulnar nerve injury**.
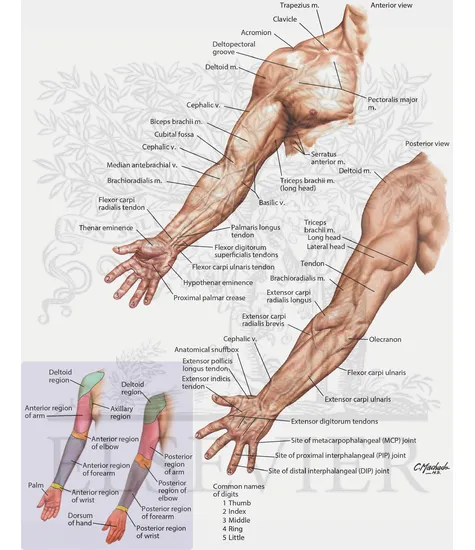
- The ulnar nerve passes through the **cubital tunnel** at the elbow, making it vulnerable to compression or trauma from direct falls.
*Axillary neuropathy*
- An **axillary nerve injury** typically presents with weakness in **shoulder abduction** (deltoid muscle) and sensory loss over the **lateral aspect of the shoulder**.
- This clinical picture does not match the patient's sensory deficits in the fingers.
*Median neuropathy*
- **Median nerve injury** at the elbow would typically cause sensory loss in the **first three fingers and the lateral half of the fourth finger**, along with **weakness in thumb opposition** and **flexion of the index and middle fingers**.
- The sensory loss described in the patient does not align with median nerve distribution.
*Radial neuropathy*
- **Radial nerve injury** at the elbow level would primarily result in **wrist drop** and sensory loss over the **dorsal aspect of the hand**, particularly the **first three and a half digits**.
- These are not the clinical findings presented by the patient.
*Musculocutaneous neuropathy*
- **Musculocutaneous nerve injury** would cause weakness in **elbow flexion** (biceps and brachialis muscles) and sensory loss over the **lateral forearm**.
- The patient's reported sensory loss is in a different distribution and no specific motor deficits of elbow flexion are mentioned.
Upper limb surface landmarks US Medical PG Question 5: A 25-year-old man comes to the physician because of right wrist pain after a fall from a ladder. Physical examination shows decreased grip strength and tenderness between the tendons of extensor pollicis longus and extensor pollicis brevis. X-ray of the right wrist shows no abnormalities. This patient is at increased risk for which of the following complications?
- A. Hypesthesia of the hypothenar eminence
- B. Paralysis of the abductor pollicis brevis muscle
- C. Contracture of the palmar aponeurosis
- D. Avascular necrosis of the scaphoid bone (Correct Answer)
- E. Osteoarthritis of the radiocarpal joint
Upper limb surface landmarks Explanation: ***Avascular necrosis of the scaphoid bone***
- The patient's symptoms (wrist pain after a fall, decreased grip strength, and tenderness in the anatomical snuffbox—between the **extensor pollicis longus** and **extensor pollicis brevis** tendons) are classic for a **scaphoid fracture**.
- X-rays may initially be normal, and the **scaphoid's tenuous blood supply**, primarily from its distal pole, makes its proximal pole particularly vulnerable to **avascular necrosis** following a fracture.
*Hypesthesia of the hypothenar eminence*
- This symptom is related to injury to the **ulnar nerve**, which typically affects the little finger and ulnar half of the ring finger, as well as the hypothenar eminence.
- A scaphoid fracture does not directly impact the **ulnar nerve** distribution in this manner.
*Paralysis of the abductor pollicis brevis muscle*
- The **abductor pollicis brevis** muscle is innervated by the **median nerve**.
- Injury to the median nerve would be required for its paralysis, which is not directly associated with a scaphoid fracture.
*Contracture of the palmar aponeurosis*
- This condition is known as **Dupuytren's contracture**, a painless progressive fibrosis of the **palmar aponeurosis**.
- It results in flexion deformities of the digits and is not caused by acute trauma like a fall, nor is it a complication of a scaphoid fracture.
*Osteoarthritis of the radiocarpal joint*
- While wrist trauma can predispose to **osteoarthritis** in the long term, it typically develops over many years.
- Avascular necrosis is a more immediate and severe complication following a **scaphoid fracture**, and is a distinct pathology from general osteoarthritis of the radiocarpal joint.
Upper limb surface landmarks US Medical PG Question 6: A 32-year-old man comes to the physician because of a 1-month history of intermittent tingling of his hand. He is an avid cyclist and has recently started training for a cycle marathon. Physical examination shows decreased grip strength in the right hand and wasting of the hypothenar eminence. On asking the patient to grasp a piece of paper between his right thumb and right index finger in the first web space, there is hyperflexion of the right thumb interphalangeal joint. Which of the following additional findings is most likely in this patient?
- A. Loss of sensation over the dorsum of the medial half of the hand
- B. Inability to extend the ring finger at the metacarpophalangeal joint
- C. Inability to flex the index finger at the interphalangeal joints
- D. Loss of sensation over the palmar aspect of the middle finger
- E. Inability to extend the little finger at the proximal interphalangeal joints (Correct Answer)
Upper limb surface landmarks Explanation: ***Inability to extend the little finger at the proximal interphalangeal joints***
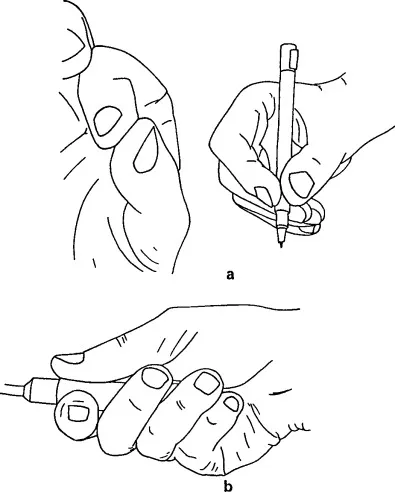
- The patient's symptoms (tingling, decreased grip strength, hypothenar eminence wasting, and **Froment's sign**) indicate **ulnar nerve compression at Guyon's canal** (handlebar palsy) from cycling.
- The ulnar nerve innervates the **3rd and 4th lumbricals** (medial two), which extend the PIP and DIP joints of the ring and little fingers.
- The ulnar nerve also innervates the **interossei muscles**, which assist in MCP flexion and IP extension.
- Loss of these intrinsic muscles results in **claw hand deformity** affecting the 4th and 5th digits, with hyperextension at MCP joints and flexion (inability to extend) at PIP and DIP joints.
- This is a classic finding in ulnar nerve palsy.
*Inability to extend the ring finger at the metacarpophalangeal joint*
- Extension at the MCP joint is primarily performed by the **extensor digitorum** (innervated by the **radial nerve**).
- The patient's findings indicate ulnar nerve compression, not radial nerve injury.
- In ulnar nerve palsy, the unopposed extensor digitorum actually causes MCP **hyperextension**, not inability to extend.
*Inability to flex the index finger at the interphalangeal joints*
- Flexion of the index finger IP joints is controlled by **flexor digitorum superficialis** (FDS) and **flexor digitorum profundus** (FDP).
- Both muscles to the index finger are innervated by the **median nerve**, not the ulnar nerve.
- This finding would indicate median nerve injury (e.g., carpal tunnel syndrome or anterior interosseous syndrome).
*Loss of sensation over the palmar aspect of the middle finger*
- Palmar sensation of the middle finger is supplied by the **median nerve**.
- The ulnar nerve supplies sensation to the medial 1.5 digits (little finger and medial half of ring finger).
- This finding would indicate median nerve pathology, not ulnar nerve compression.
*Loss of sensation over the dorsum of the medial half of the hand*
- The **dorsal cutaneous branch of the ulnar nerve** branches approximately 5-8 cm proximal to the wrist and passes **superficially**, NOT through Guyon's canal.
- In **Guyon's canal compression** (handlebar palsy), the dorsal cutaneous branch is **SPARED**, so dorsal sensation remains intact.
- The patient would have palmar sensory loss over the medial 1.5 digits but **preserved dorsal sensation**.
- Loss of dorsal sensation would suggest a more proximal ulnar nerve lesion (at the elbow or forearm), not at the wrist.
Upper limb surface landmarks US Medical PG Question 7: A 25-year-old man was referred to a neurologist for right-hand weakness. He was involved in a motor vehicle accident 2 months ago in which his right hand was injured. On examination, his grip is weak, especially in fingers 2, 4, and 5 and he is unable to adduct these fingers. Which of the following groups of muscles is most likely affected?
- A. Flexor digitorum profundus
- B. Palmar interossei muscles (Correct Answer)
- C. Lumbrical muscles
- D. Dorsal interossei muscles
- E. Extensor digitorum
Upper limb surface landmarks Explanation: ***Palmar interossei muscles***
- The inability to **adduct fingers 2, 4, and 5** (index, ring, and pinky fingers) is the key finding. The **palmar interossei** are responsible for adduction of these fingers towards the middle finger.
- Weak grip in these specific fingers indicates impairment of the muscles controlling their movement and adduction, which are primarily the palmar interossei.
*Flexor digitorum profundus*
- The **flexor digitorum profundus** primarily **flexes the distal interphalangeal (DIP) joints** of the fingers, as well as assists in flexing the proximal interphalangeal (PIP) and metacarpophalangeal (MCP) joints.
- While it contributes to grip strength, its primary role is flexion, not adduction, and weakness would typically present as difficulty with deep finger flexion rather than specific adduction issues.
*Lumbrical muscles*
- The **lumbrical muscles** **flex the metacarpophalangeal (MCP) joints** and **extend the interphalangeal (IP) joints**. This action is characteristic of the "lumbrical grip" or "writing position."
- Their primary function does not involve adduction of the fingers, and their weakness would manifest differently.
*Dorsal interossei muscles*
- The **dorsal interossei muscles** are responsible for **abduction of the fingers** (spreading them apart).
- The patient's inability to adduct fingers rules out the dorsal interossei as the primary affected group, as these muscles perform the opposite action.
*Extensor digitorum*
- The **extensor digitorum** primarily **extends the metacarpophalangeal (MCP) and interphalangeal (IP) joints** of the medial four fingers.
- Weakness in this muscle would result in difficulty extending the fingers, leading to a "dropped finger" appearance or inability to straighten the fingers, which is contrary to the described adduction deficit.
Upper limb surface landmarks US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Upper limb surface landmarks Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Upper limb surface landmarks US Medical PG Question 9: A 67-year-old male presents to his primary care physician for evaluation of fever and an unintended weight loss of 25 pounds over the last 4 months. He also has decreased appetite and complains of abdominal pain located in the right upper quadrant. The patient has not noticed any changes in stool or urine. He emigrated from Malaysia to the United States one year prior. Social history reveals that he smokes half a pack per day and has 5-7 drinks of alcohol per day. The patient is up to date on all of his vaccinations. Physical exam findings include mild jaundice as well as an enlarged liver edge that is tender to palpation. Based on clinical suspicion, biomarker labs are sent and show polycythemia and an elevated alpha fetoprotein level but a normal CA 19-9 level. Surface antigen for hepatitis B is negative. Ultrasound reveals a normal sized gallbladder. Given this presentation, which of the following organisms was most likely associated with the development of disease in this patient?
- A. Naked DNA virus
- B. Enveloped DNA virus
- C. Curved gram-negative bacteria
- D. Acute angle branching fungus
- E. Trematode from undercooked fish (Correct Answer)
Upper limb surface landmarks Explanation: ***Trematode from undercooked fish***
- The patient's symptoms (fever, RUQ pain, weight loss, jaundice, hepatomegaly, elevated **AFP**, and normal CA 19-9) point strongly towards **hepatocellular carcinoma (HCC)**.
- The history of emigration from Malaysia and the elevated **alpha-fetoprotein (AFP)** despite negative hepatitis B antigen, suggest a parasitic infection, specifically a liver fluke (trematode), as a risk factor for HCC. **Clonorchis sinensis** and **Opisthorchis viverrini** are trematodes acquired from undercooked freshwater fish, endemic to Southeast Asia, and are known to cause cholangiocarcinoma and, less commonly, HCC.
*Naked DNA virus*
- This typically refers to viruses like **human papillomavirus (HPV)** or **adenovirus**, which are not primary causes of the described liver pathology or HCC with this specific presentation.
- While some naked DNA viruses can cause human disease, they are not typically linked to the patient's specific symptoms and lab findings (elevated AFP) in the context of liver cancer from a Southeast Asian background.
*Enveloped DNA virus*
- This category includes viruses like **Herpesviruses** and **Hepatitis B virus (HBV)**. While HBV is a major cause of HCC, the patient's hepatitis B surface antigen is negative, ruling out active or chronic HBV infection as the direct cause in this case.
- Other enveloped DNA viruses do not commonly cause this specific cluster of symptoms and risk factors for HCC.
*Curved gram-negative bacteria*
- This description often refers to bacteria like **Campylobacter** or **Helicobacter pylori**. These can cause gastrointestinal issues but are not typically associated with liver masses, jaundice, and elevated AFP in the context of HCC.
- They do not explain the patient's risk factors or presentation that strongly suggests chronic liver inflammation leading to cancer.
*Acute angle branching fungus*
- This refers to fungi like **Aspergillus**, which can cause invasive infections, particularly in immunocompromised individuals.
- While Aspergillus can cause pulmonary infections and, less commonly, disseminate to other organs including the liver, it does not typically present with the described risk factors (Southeast Asian origin, undercooked fish consumption) or lab findings (elevated AFP) for HCC, nor does it fit the general clinical picture.
Upper limb surface landmarks US Medical PG Question 10: A 45-year-old woman presents to her primary care provider for wrist pain. She reports a 4-month history of gradually worsening pain localized to the radial side of her right wrist. The pain is dull, non-radiating, and intermittent. Her past medical history is notable for rheumatoid arthritis and von Willebrand disease. She does not smoke and drinks alcohol socially. She is active in her neighborhood’s local badminton league. Her temperature is 98.6°F (37°C), blood pressure is 125/75 mmHg, pulse is 80/min, and respirations are 18/min. On exam, she has mild tenderness to palpation in her thenar snuffbox. Nodules are located on the proximal interphalangeal joints of both hands. Ulnar deviation of the hand with her thumb clenched in her palm produces pain. Which of the following muscles in most likely affected in this patient?
- A. Abductor pollicis longus (Correct Answer)
- B. Extensor pollicis brevis
- C. Flexor pollicis longus
- D. Opponens pollicis
- E. Adductor pollicis
Upper limb surface landmarks Explanation: ***Abductor pollicis longus***
- The symptoms, particularly **pain in the radial wrist** exacerbated by **ulnar deviation of the hand with the thumb clenched in the palm** (a positive **Finkelstein's test**), are classic for **De Quervain's tenosynovitis**.
- **De Quervain's tenosynovitis** specifically affects the tendons within the **first dorsal compartment of the wrist**, which contains the **abductor pollicis longus** and **extensor pollicis brevis** tendons.
- The **abductor pollicis longus is the PRIMARY and MOST COMMONLY affected muscle** in De Quervain's tenosynovitis, as it is the larger tendon and bears greater mechanical stress from repetitive thumb and wrist movements (such as in badminton).
- While both tendons share the same synovial sheath and can be inflamed, **APL is considered the principal muscle affected** in this condition.
*Extensor pollicis brevis*
- This muscle is also involved in **De Quervain's tenosynovitis** alongside the **abductor pollicis longus**, as both tendons share the same synovial sheath in the first dorsal compartment.
- However, the **abductor pollicis longus is more commonly and primarily affected**, making it the better answer when asked which muscle is "most likely" involved.
- In some cases, EPB may not be involved at all, whereas APL is consistently affected.
*Flexor pollicis longus*
- This muscle is located on the **volar (palm side)** aspect of the forearm and hand and is primarily responsible for **flexion of the thumb's interphalangeal joint**.
- Involvement of this muscle would present with pain on the palmar side of the wrist or thumb, and potentially **trigger thumb**, not radial-sided wrist pain with positive Finkelstein's test.
*Opponens pollicis*
- This muscle is located deep in the thenar eminence and is responsible for **opposition of the thumb**, bringing it across the palm to touch other fingers.
- Isolated injury or inflammation of the **opponens pollicis** would typically cause pain and weakness with thumb opposition, not the characteristic radial wrist pain with positive Finkelstein's test.
*Adductor pollicis*
- This muscle is responsible for **adduction of the thumb**, pulling it towards the palm, and is located in the intrinsic muscles of the hand.
- Pain related to the **adductor pollicis** would be felt more deeply in the thenar web space or palm, and would not be exacerbated by the Finkelstein maneuver eliciting radial wrist pain.
More Upper limb surface landmarks US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.