Thoracic surface landmarks US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thoracic surface landmarks. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thoracic surface landmarks US Medical PG Question 1: A 24-year-old man is brought to the emergency department after being involved in a motor vehicle accident as an unrestrained driver. He was initially found unconscious at the scene but, after a few minutes, he regained consciousness. He says he is having difficulty breathing and has right-sided pleuritic chest pain. A primary trauma survey reveals multiple bruises and lacerations on the anterior chest wall. His temperature is 36.8°C (98.2°F), blood pressure is 100/60 mm Hg, pulse is 110/min, and respiratory rate is 28/min. Physical examination reveals a penetrating injury just below the right nipple. Cardiac examination is significant for jugular venous distention. There is also an absence of breath sounds on the right with hyperresonance to percussion. A bedside chest radiograph reveals evidence of a collapsed right lung with depression of the right hemidiaphragm and tracheal deviation to the left. Which of the following is the most appropriate next step in the management of this patient?
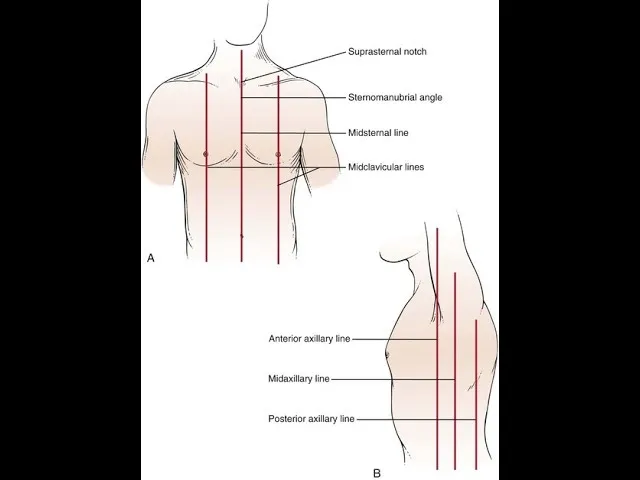
- A. Tube thoracostomy at the 2nd intercostal space, midclavicular line
- B. Tube thoracostomy at the 5th intercostal space, midclavicular line
- C. Tube thoracostomy at the 5th intercostal space, anterior axillary line
- D. Needle thoracostomy at the 5th intercostal space, midclavicular line
- E. Needle thoracostomy at the 2nd intercostal space, midclavicular line (Correct Answer)
Thoracic surface landmarks Explanation: **Needle thoracostomy at the 2nd intercostal space, midclavicular line**
- The patient presents with classic signs of **tension pneumothorax**, including respiratory distress, hypotension, tachycardia, jugular venous distention, absent breath sounds, hyperresonance to percussion, tracheal deviation away from the affected side, and mediastinal shift.
- **Needle thoracostomy** in the 2nd intercostal space at the midclavicular line is the most appropriate *initial* life-saving intervention for tension pneumothorax, as it rapidly decompresses the pleural space.
*Tube thoracostomy at the 2nd intercostal space, midclavicular line*
- While a **tube thoracostomy (chest tube insertion)** is the definitive treatment for pneumothorax, it is not the immediate first step for a **tension pneumothorax** due to the time constraint and the need for immediate decompression.
- The 2nd intercostal space, midclavicular line, is an appropriate site for needle decompression, but a chest tube is typically inserted at a different location (5th intercostal space, anterior axillary line).
*Tube thoracostomy at the 5th intercostal space, midclavicular line*
- This location is not the standard site for either needle decompression or definitive chest tube insertion. The **midaxillary or anterior axillary line** is preferred for chest tube placement to avoid neurovascular bundles.
- Again, while a chest tube is needed, it is not the *immediate* first step for a **tension pneumothorax**.
*Tube thoracostomy at the 5th intercostal space, anterior axillary line*
- This is the **correct anatomical location** for definitive chest tube insertion for a pneumothorax or hemothorax.
- However, in the setting of acute **tension pneumothorax**, **needle decompression** is required first to rapidly decompress the intrathoracic pressure and stabilize the patient before a chest tube can be placed.
*Needle thoracostomy at the 5th intercostal space, midclavicular line*
- The **5th intercostal space** is too low for an effective needle decompression of a tension pneumothorax.
- The standard site for needle decompression of a tension pneumothorax is the **2nd intercostal space, midclavicular line**, due to its safety and effectiveness in accessing the pleural space.
Thoracic surface landmarks US Medical PG Question 2: An 18-year-old man is brought to the emergency department 30 minutes after being stabbed in the chest during a fight. He has no other injuries. His pulse is 120/min, blood pressure is 90/60 mm Hg, and respirations are 22/min. Examination shows a 4-cm deep, straight stab wound in the 4th intercostal space 2 cm medial to the right midclavicular line. The knife most likely passed through which of the following structures?
- A. Serratus anterior muscle, pleura, inferior vena cava
- B. External oblique muscle, superior epigastric artery, azygos vein
- C. Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver
- D. Intercostal muscles, internal thoracic artery, right heart
- E. Pectoral fascia, transversus thoracis muscle, right lung (Correct Answer)
Thoracic surface landmarks Explanation: ***Pectoral fascia, transversus thoracis muscle, right lung***
* The stab wound is in the **4th intercostal space**, 2 cm medial to the right midclavicular line, placing it over the anterior chest wall. This trajectory would first penetrate the **pectoral fascia**.
* Deeper structures in this region include the **transversus thoracis muscle** and, given the depth, the **right lung** as it extends superiorly behind the anterior chest wall.
* *Serratus anterior muscle, pleura, inferior vena cava*
* The **serratus anterior muscle** is more laterally positioned, typically covering the side of the rib cage.
* The **inferior vena cava** is located more medially and posteriorly within the mediastinum, deep to the diaphragm, making it an unlikely target for an anterior 4th intercostal stab.
* *External oblique muscle, superior epigastric artery, azygos vein*
* The **external oblique muscle** is part of the abdominal wall and would not be penetrated in the 4th intercostal space.
* The **superior epigastric artery** is lower, typically extending into the abdominal wall, and the **azygos vein** is in the posterior mediastinum, not in the path of this superficial anterior stab wound.
* *Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver*
* The **pectoralis minor muscle** is located deep to the pectoralis major, which would be penetrated. However, a stab at the 4th intercostal space would be too high to directly involve the **dome of the diaphragm** or the **right lobe of the liver**, which are typically below the 5th intercostal space, especially in forced expiration.
* *Intercostal muscles, internal thoracic artery, right heart*
* The **intercostal muscles** would certainly be traversed.
* However, the **internal thoracic artery** runs paramedially (about 1-2 cm from the sternum), and getting to the **right heart** would require a more medial and deeper trajectory, potentially causing immediate tamponade or severe hemorrhage.
Thoracic surface landmarks US Medical PG Question 3: A 33-year-old woman is brought to the emergency department 15 minutes after being stabbed in the chest with a screwdriver. Her pulse is 110/min, respirations are 22/min, and blood pressure is 90/65 mm Hg. Examination shows a 5-cm deep stab wound at the upper border of the 8th rib in the left midaxillary line. Which of the following structures is most likely to be injured in this patient?
- A. Left kidney
- B. Left ventricle
- C. Intercostal nerve
- D. Lower lung lobe (Correct Answer)
- E. Spleen
Thoracic surface landmarks Explanation: ***Lower lung lobe***
- A stab wound at the **8th rib in the left midaxillary line** is located within the anatomical boundaries of the **lower lobe of the left lung**. The diaphragm can rise to the level of the 5th intercostal space during expiration, and the lung extends into this region.
- The patient's **hypotension** and **tachycardia** are consistent with potential **hemorrhage** or **pneumothorax/hemothorax** due to lung injury.
*Left kidney*
- The left kidney is located retroperitoneally, typically at the level of the **T12 to L3 vertebrae**, making it less likely to be injured by a stab wound at the 8th rib in the midaxillary line of a standing or supine patient.
- Injury to the kidney would likely cause **hematuria**, which is not mentioned in the presentation as an immediate concern.
*Left ventricle*
- The left ventricle is located more medially and anteriorly within the chest, deep to the **sternum** and **costal cartilages**, making a stab wound at the 8th rib in the midaxillary line an unlikely entry point.
- Cardiac tamponade or severe hemorrhage from left ventricular injury would typically present with more rapid and profound hemodynamic collapse.
*Intercostal nerve*
- While an intercostal nerve would certainly be injured by a stab wound through the intercostal space, injury to the nerve alone would not explain the patient's **hemodynamic instability** (hypotension and tachycardia).
- Isolated intercostal nerve injury primarily causes **localized pain** and potentially some sensory or motor deficits in the distribution of that nerve.
*Spleen*
- The spleen is located in the left upper quadrant, typically lying beneath the **9th to 11th ribs**, making injury to the spleen possible with a deeper wound. However, it is situated more laterally and posteriorly than the lung at the 8th rib midaxillary line.
- While splenic injury can cause **hypotension** and **tachycardia**, the lung lies in a more superficial and posterior plane relative to the 8th rib in the midaxillary line, making it a more direct target for injury.
Thoracic surface landmarks US Medical PG Question 4: A 10-year-old boy is brought to the clinic by his mother with complaints of cough productive of yellow sputum for the past couple of weeks. This is the 4th episode the boy has had this year. He has had recurrent episodes of cough since childhood, and previous episodes have subsided with antibiotics. There is no family history of respiratory disorders. His vaccinations are up to date. He has a heart rate of 98/min, respiratory rate of 13/min, temperature of 37.6°C (99.7°F), and blood pressure of 102/70 mm Hg. Auscultation of the chest reveals an apex beat on the right side of the chest. A chest X-ray reveals that the cardiac apex is on the right. A high-resolution CT scan is performed which is suggestive of bronchiectasis. Which of the following structures is most likely impaired in this patient?
- A. Neurofilaments
- B. Dynein (Correct Answer)
- C. Kinesin
- D. Microvilli
- E. Microfilaments
Thoracic surface landmarks Explanation: ***Dynein***
- The combination of **recurrent respiratory infections** leading to **bronchiectasis** and **situs inversus** (apex beat on the right, cardiac apex on the right) is characteristic of **primary ciliary dyskinesia (PCD)**, also known as Kartagener syndrome.
- **Dynein arms** are crucial for the beating motion of cilia. An impairment in dynein function leads to ineffective ciliary clearance in the respiratory tract and defective embryonic rotation, causing situs inversus.
*Neurofilaments*
- **Neurofilaments** are intermediate filaments found in neurons, primarily providing structural support to axons.
- Their dysfunction is associated with various neurological disorders, but not with respiratory infections or situs inversus.
*Kinesin*
- **Kinesin** is a motor protein that moves along microtubules, typically transporting cargo away from the cell nucleus (anterograde transport).
- While important for intracellular transport, kinesin dysfunction does not explain the specific constellation of symptoms seen in primary ciliary dyskinesia.
*Microvilli*
- **Microvilli** are actin-filled projections on the surface of some epithelial cells, primarily increasing surface area for absorption.
- They are not involved in ciliary motility or mucociliary clearance, and their impairment would not lead to bronchiectasis or situs inversus.
*Microfilaments*
- **Microfilaments** (actin filaments) are involved in cell shape, motility, and cytokinesis, but are not the primary structural component responsible for ciliary beating.
- While integral to many cellular processes, their direct impairment does not cause the specific symptoms of primary ciliary dyskinesia.
Thoracic surface landmarks US Medical PG Question 5: A 31-year-old woman presents to the clinic with shortness of breath, palpitations, and fatigue. She has had these symptoms over the last several weeks. She had been tolerating these symptoms until last night when she could not fall asleep due to palpitations. She has a past medical history of infective endocarditis 6 months ago that was successfully treated with antibiotics. She does not smoke or drink alcohol. Her blood pressure is 138/89 mm Hg and her pulse is 76/min and regular. The cardiac exam reveals a soft S1, S3 gallop, a hyperdynamic apex beat, and a pansystolic murmur that radiates to the axilla on auscultation. Echocardiography reveals incompetence of one of the valves. Which of the following sites is the best position to auscultate this defect?
- A. Medial end of the 2nd intercostal space on the right side
- B. 4th intercostal space at the midclavicular line on the left side
- C. 5th intercostal space at the midclavicular line on the left side (Correct Answer)
- D. Medial end of the 2nd intercostal space on the left side
- E. Right lower end of the body of the sternum
Thoracic surface landmarks Explanation: ***5th intercostal space at the midclavicular line on the left side***
- The patient's symptoms (shortness of breath, palpitations, fatigue, S3 gallop, hyperdynamic apex beat, and a pansystolic murmur radiating to the axilla) following infective endocarditis strongly suggest **mitral regurgitation**.
- The **mitral valve** is best auscultated at the **cardiac apex**, which is located at the **5th intercostal space at the midclavicular line on the left side**.
*Medial end of the 2nd intercostal space on the right side*
- This position is the **aortic area**, where murmurs related to the **aortic valve** (e.g., aortic stenosis or regurgitation) are best heard.
- An aortic murmur would not typically radiate to the axilla.
*4th intercostal space at the midclavicular line on the left side*
- This location is slightly above the typical apex beat and is not the primary auscultation site for any major cardiac valve.
- While close to the mitral area, it is not the optimal point for identifying mitral valve pathology.
*Medial end of the 2nd intercostal space on the left side*
- This position is the **pulmonic area**, where murmurs related to the **pulmonic valve** (e.g., pulmonary stenosis or regurgitation) are best heard.
- A pulmonic murmur would not cause a hyperdynamic apex beat or radiate to the axilla.
*Right lower end of the body of the sternum*
- This location corresponds to the **tricuspid area**, where murmurs related to the **tricuspid valve** (e.g., tricuspid regurgitation or stenosis) are best heard.
- Tricuspid murmurs are often amplified with inspiration and typically do not radiate to the axilla.
Thoracic surface landmarks US Medical PG Question 6: A 45-year-old male is brought into the emergency room by emergency medical services due to a stab wound in the chest. The wound is located superior and medial to the left nipple. Upon entry, the patient appears alert and is conversational, but soon becomes confused and loses consciousness. The patient's blood pressure is 80/40 mmHg, pulse 110/min, respirations 26/min, and temperature 97.0 deg F (36.1 deg C). On exam, the patient has distended neck veins with distant heart sounds. What is the next best step to increase this patient's survival?
- A. Heparin
- B. Intravenous fluids
- C. Aspirin
- D. Intravenous colloids
- E. Pericardiocentesis (Correct Answer)
Thoracic surface landmarks Explanation: ***Pericardiocentesis***
- The patient's presentation with **hypotension**, **tachycardia**, **distended neck veins**, and **distant heart sounds** after a chest stab wound is classic for **cardiac tamponade** (Beck's triad).
- **Pericardiocentesis** is the immediate life-saving procedure to drain the pericardial fluid and relieve pressure on the heart, improving cardiac output.
- In penetrating trauma, this serves as a **bridge to definitive surgical management** (thoracotomy or sternotomy).
*Heparin*
- **Heparin** is an anticoagulant and would worsen the situation by increasing bleeding into the pericardial space due to the stab wound.
- It is contraindicated in active bleeding and traumatic injury.
*Intravenous fluids*
- While **IV fluid resuscitation is recommended** in cardiac tamponade to maintain preload and support cardiac output, fluids alone **do not address the underlying mechanical obstruction**.
- The primary issue is **extrinsic compression of the heart** requiring drainage, not hypovolemia alone.
- Fluids are supportive but not definitive—**pericardiocentesis is the life-saving intervention**.
*Aspirin*
- **Aspirin** is an antiplatelet agent and would increase the risk of bleeding, exacerbating the patient's condition.
- It is used for conditions like myocardial infarction or stroke prevention, not for acute traumatic bleeding.
*Intravenous colloids*
- Similar to crystalloid fluids, **colloids** may provide temporary hemodynamic support but do not relieve the mechanical compression of the heart.
- They are supportive measures that **do not substitute for definitive pericardial drainage**.
Thoracic surface landmarks US Medical PG Question 7: A 23-year-old man is brought to the emergency department by a coworker for an injury sustained at work. He works in construction and accidentally shot himself in the chest with a nail gun. Physical examination shows a bleeding wound in the left hemithorax at the level of the 4th intercostal space at the midclavicular line. Which of the following structures is most likely injured in this patient?
- A. Right atrium of the heart
- B. Inferior vena cava
- C. Left upper lobe of the lung (Correct Answer)
- D. Left atrium of the heart
- E. Superior vena cava
Thoracic surface landmarks Explanation: ***Left upper lobe of the lung***
- The **left upper lobe of the lung** extends to the 4th intercostal space at the midclavicular line, making it the most probable structure to be traversed by a penetrating injury at this location.
- The **pleural cavity** and lung tissue are superficially located in this region, making them highly susceptible to injury from a nail gun.
*Right atrium of the heart*
- The **right atrium** is located predominantly on the right side of the sternum, more centrally, and slightly to the right of the midclavicular line.
- An injury at the **left 4th intercostal space at the midclavicular line** would typically be too lateral and superior to directly injure the right atrium.
*Inferior vena cava*
- The **inferior vena cava (IVC)** enters the right atrium from below, primarily located within the abdomen and passing through the diaphragm at the level of T8.
- Its position is far too **inferior and posterior** relative to the 4th intercostal space to be directly injured by this wound.
*Left atrium of the heart*
- The **left atrium** is the most posterior chamber of the heart and is largely covered by the left ventricle.
- Although part of the heart is on the left, an injury at the **4th intercostal space, midclavicular line**, would likely impact the left ventricle or lung tissue before reaching the left atrium, which is located more posteriorly and medially.
*Superior vena cava*
- The **superior vena cava (SVC)** is located to the right of the midline, formed by the brachiocephalic veins behind the right first costal cartilage.
- Its position is too **medial and superior**, on the right side, to be directly injured by a nail penetrating the left 4th intercostal space at the midclavicular line.
Thoracic surface landmarks US Medical PG Question 8: A 33-year-old pregnant woman at 38 weeks gestation requires emergency cesarean section. The obstetrician must perform a perimortem procedure due to maternal cardiac arrest. She makes a Pfannenstiel incision but encounters significant bleeding. The patient has a history of previous cesarean section with documented bladder injury. Considering the surface anatomy and previous surgery, evaluate the most likely source of bleeding and the anatomical relationship that increases risk in this scenario.
- A. External iliac vessels exposed due to loss of normal tissue planes from adhesions
- B. Superficial epigastric vessels in the subcutaneous tissue
- C. Inferior epigastric vessels injured due to lateral extension of the incision (Correct Answer)
- D. Uterine vessels injured due to lower segment extension
- E. Superior vesical arteries injured due to abnormal bladder position from scarring
Thoracic surface landmarks Explanation: ***Inferior epigastric vessels injured due to lateral extension of the incision***
- A **Pfannenstiel incision** is a transverse incision performed 2-3 cm above the symphysis pubis; extending this incision too far laterally increases the risk of transecting the **inferior epigastric vessels**.
- These vessels are located deep to the **rectus abdominis** muscle but lateral to its midline, making them susceptible during emergency procedures where rapid extension of the surgical field is required.
*Uterine vessels injured due to lower segment extension*
- The **uterine vessels** are located within the **broad ligament** and are typically injured during the hysterotomy (uterine incision) phase rather than the initial abdominal wall approach.
- While heavy bleeding occurs if the uterine incision extends laterally into the **vascular pedicle**, it does not correlate with superficial anatomical landmarks of a Pfannenstiel incision.
*External iliac vessels exposed due to loss of normal tissue planes from adhesions*
- The **external iliac vessels** are retroperitoneal structures and are generally too deep and lateral to be the primary source of bleeding in a standard **Pfannenstiel incision**.
- Although **adhesions** can distort anatomy, injury to these vessels is more common in extensive pelvic lymphadenectomy or oncological surgeries rather than a perimortem C-section.
*Superficial epigastric vessels in the subcutaneous tissue*
- The **superficial epigastric vessels** run in the **Camper's fascia** and are commonly transected during the initial skin incision, but they rarely cause "significant" or life-threatening bleeding compared to deeper vessels.
- Bleeding from these vessels is usually easily controlled with cautery or pressure and does not represent the primary anatomical risk of lateral **Pfannenstiel extension**.
*Superior vesical arteries injured due to abnormal bladder position from scarring*
- The **superior vesical arteries** supply the upper portion of the bladder; while at risk during dissection of a **scarred bladder flap**, they are not the source encountered during the abdominal wall incision.
- Previous **bladder injury** increases the risk of cystotomy, but the vascular supply to the bladder is located deep within the pelvic cavity, not at the level of the **rectus sheath**.
Thoracic surface landmarks US Medical PG Question 9: A 71-year-old man with atrial fibrillation presents with sudden onset of severe abdominal pain out of proportion to physical findings. He has mild diffuse tenderness but no peritoneal signs. His lactate is 4.5 mmol/L. CT angiography shows occlusion of a major mesenteric vessel. The surgeon explains that the occluded vessel supplies the midgut from just distal to the second part of the duodenum to the proximal two-thirds of the transverse colon. Based on surface anatomy, at what vertebral level does this vessel originate?
- A. L3
- B. T12
- C. L1 (Correct Answer)
- D. L2
- E. T10
Thoracic surface landmarks Explanation: ***L1***
- The clinical presentation describes **acute mesenteric ischemia** involving the **Superior Mesenteric Artery (SMA)**, which supplies the embryologic **midgut**.
- The SMA originates from the **abdominal aorta** behind the neck of the pancreas at the level of the **L1 vertebra**.
*T10*
- The **esophagus** passes through the diaphragm at the **T10 level** via the esophageal hiatus.
- No major abdominal vascular branches supplying the gastrointestinal tract originate at this specific thoracic level.
*T12*
- This is the level of the **celiac trunk**, which supplies the **foregut** structures including the stomach, liver, and spleen.
- It also marks the **aortic hiatus** where the aorta enters the abdominal cavity from the thorax.
*L2*
- This level corresponds to the origin of the **renal arteries** and the site where the **duodenojejunal flexure** is suspended by the ligament of Treitz.
- While the SMA is in close proximity, its distinct origin from the aorta is characteristically at the **L1 level**.
*L3*
- This is the level of origin for the **Inferior Mesenteric Artery (IMA)**, which supplies the **hindgut** including the distal third of the transverse colon.
- Clinical findings in this case point to midgut ischemia, which is associated with the **Superior Mesenteric Artery** rather than the IMA.
Thoracic surface landmarks US Medical PG Question 10: A 25-year-old motorcyclist presents after a high-speed collision with facial trauma. Clinical examination reveals cerebrospinal fluid rhinorrhea, periorbital ecchymosis, and numbness over the cheek and upper teeth. CT shows a fracture extending through a foramen at the apex of the orbit. Based on the clinical presentation and surface anatomy, which foramen is most likely involved?
- A. Foramen rotundum (Correct Answer)
- B. Superior orbital fissure
- C. Infraorbital foramen
- D. Inferior orbital fissure
- E. Optic canal
Thoracic surface landmarks Explanation: ***Foramen rotundum***
- The **foramen rotundum** transmits the **maxillary nerve (V2)**; trauma here explains the **numbness over the cheek** and **upper teeth** as these are within the V2 sensory distribution.
- Located at the **apex of the orbit**, this foramen communicates with the pterygopalatine fossa and is frequently involved in high-velocity fractures causing **middle cranial fossa** disruption and CSF rhinorrhea.
*Optic canal*
- The **optic canal** transmits the **optic nerve (CN II)** and the **ophthalmic artery**.
- Damage would result in **visual field defects** or blindness and an abnormal **pupillary light reflex**, rather than facial sensory loss.
*Superior orbital fissure*
- This fissure transmits **CN III, IV, VI** and the **ophthalmic nerve (V1)**; damage would cause **ophthalmoplegia** and forehead numbness.
- It does not carry the **V2 branch**, thus it cannot account for the loss of sensation in the **cheek and upper teeth**.
*Infraorbital foramen*
- While the **infraorbital nerve** (a branch of V2) passes here to supply the cheek, this foramen is on the **anterior surface of the maxilla**, not at the **apex of the orbit**.
- Trauma at this superficial site would not typically present with **CSF rhinorrhea**, which indicates a more deep-seated skull base fracture.
*Inferior orbital fissure*
- This fissure is located between the floor and lateral wall of the orbit but is not situated at the **apex** where the injury is described.
- While it transmits the **infraorbital nerve**, it is not a pathway through which a skull base injury leads to **CSF leakage** into the nasal cavity.
More Thoracic surface landmarks US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.