Surface anatomy for nerve blocks US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Surface anatomy for nerve blocks. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Surface anatomy for nerve blocks US Medical PG Question 1: A 65-year-old man presents to the dermatology clinic to have a basal cell carcinoma excised from his upper back. The lesion measures 2.3 x 3.2 cm. He has a medical history significant for hypertension and diabetes mellitus type II, for which he takes lisinopril and metformin, respectively. He has had a basal cell carcinoma before which was excised in the clinic without complications. Which of the following modes of anesthesia should be used for this procedure?
- A. Moderate sedation
- B. Peripheral nerve block
- C. General anesthesia
- D. Spinal anesthesia
- E. Local anesthesia (Correct Answer)
Surface anatomy for nerve blocks Explanation: ***Local anesthesia***
- This is the preferred method for **basal cell carcinoma excisions**, especially for lesions of this size and location, as it provides adequate pain control with minimal systemic effects.
- The patient's prior uncomplicated excision under local anesthesia further supports its suitability and safety for this procedure.
*Moderate sedation*
- While it can provide comfort, it involves systemic medications that carry risks of **respiratory depression** and **hemodynamic instability**, which are generally unnecessary for a routine skin excision in a stable patient.
- It also requires more extensive monitoring and recovery time compared to local anesthesia.
*Peripheral nerve block*
- A peripheral nerve block might be considered for larger or deeper excisions in specific anatomical areas, but for a typical basal cell carcinoma on the back, **infiltration with local anesthetic** is usually sufficient and less invasive than a nerve block.
- It is not routinely necessary for superficial skin excisions of this nature.
*General anesthesia*
- This is **excessive and unnecessary** for a routine basal cell carcinoma excision, especially given the patient's comorbidities of hypertension and diabetes, which would increase the risks associated with general anesthesia.
- General anesthesia is reserved for very extensive resections, complex reconstructions, or patients unable to cooperate under local anesthesia.
*Spinal anesthesia*
- **Spinal anesthesia** is typically used for procedures involving the lower abdomen, perineum, or lower extremities, and it is **not indicated** for an excision on the upper back.
- It carries risks such as post-dural puncture headache and hypotension, which are unwarranted for this type of superficial surgery.
Surface anatomy for nerve blocks US Medical PG Question 2: A 20-year-old man comes to the clinic complaining of shoulder pain for the past week. He is a pitcher for the baseball team at his university and reports that the pain started shortly after a game. The pain is described as achy and dull, intermittent, 7/10, and is concentrated around the right shoulder area. He denies any significant medical history, trauma, fever, recent illness, or sensory changes but endorses some difficulty lifting his right arm. A physical examination demonstrates mild tenderness of the right shoulder. When the patient is instructed to resist arm depression when holding his arms parallel to the floor with the thumbs pointing down, he reports significant pain of the right shoulder. Strength is 4/5 on the right and 5/5 on the left with abduction of the upper extremities. What nerve innervates the injured muscle in this patient?
- A. Axillary nerve
- B. Long thoracic nerve
- C. Subscapular nerve
- D. Accessory nerve
- E. Suprascapular nerve (Correct Answer)
Surface anatomy for nerve blocks Explanation: ***Suprascapular nerve***
- The patient's symptoms, including shoulder pain exacerbated by the <b>"empty can" test</b> (resisted arm depression with thumbs down), are highly suggestive of a <b>rotator cuff injury</b>, specifically involving the <b>supraspinatus muscle</b>.
- The <b>suprascapular nerve</b> innervates both the <b>supraspinatus</b> and <b>infraspinatus muscles</b>, which are critical for shoulder abduction and external rotation.
*Axillary nerve*
- The <b>axillary nerve</b> innervates the <b>deltoid muscle</b> and the <b>teres minor muscle</b>.
- Injury to the axillary nerve or these muscles would primarily affect <b>shoulder abduction</b> beyond the initial 15 degrees and external rotation, but the "empty can" test specifically targets the supraspinatus.
*Long thoracic nerve*
- The <b>long thoracic nerve</b> innervates the <b>serratus anterior muscle</b>, which is responsible for scapular protraction and upward rotation.
- Damage to this nerve typically presents with "<b>winged scapula</b>," which is not indicated in this case.
*Subscapular nerve*
- The <b>subscapular nerve</b> innervates the <b>subscapularis muscle</b> (upper and lower subscapular nerves), which is a key internal rotator of the shoulder.
- While it's a rotator cuff muscle, injury to the subscapularis would primarily manifest as difficulty with internal rotation, not typically identified by the "empty can" test.
*Accessory nerve*
- The <b>accessory nerve (cranial nerve XI)</b> innervates the <b>sternocleidomastoid</b> and <b>trapezius muscles</b>.
- Injury to this nerve would result in difficulty shrugging the shoulders or turning the head, not pain related to rotator cuff function.
Surface anatomy for nerve blocks US Medical PG Question 3: A 31-year-old woman with multiple sclerosis comes to the physician because of a 4-day history of cramps in her left leg. Physical examination shows flexion of the left hip and increased tone in the thigh muscles. A local anesthetic block of which of the following nerves would most likely improve this patient's condition the most?
- A. Inferior gluteal nerve
- B. Superior gluteal nerve
- C. Femoral nerve (Correct Answer)
- D. Sciatic nerve
- E. Obturator nerve
Surface anatomy for nerve blocks Explanation: ***Femoral nerve***
- The **femoral nerve** innervates the **iliacus** (a primary hip flexor) and the **rectus femoris** (part of the quadriceps that assists in hip flexion), as well as the entire **quadriceps femoris group** (responsible for knee extension and contributing to increased thigh muscle tone).
- In this patient with spasticity, **hip flexion** is caused by hypertonicity of iliopsoas and rectus femoris, while **increased tone in thigh muscles** reflects quadriceps involvement.
- Blocking the femoral nerve would relax these muscles, thereby improving the **cramps, hip flexion, and increased thigh tone**.
*Inferior gluteal nerve*
- The **inferior gluteal nerve** primarily innervates the **gluteus maximus muscle**, which is involved in hip extension and external rotation, not hip flexion.
- Blocking this nerve would not directly address the symptoms of increased thigh muscle tone and hip flexion.
*Superior gluteal nerve*
- The **superior gluteal nerve** mainly innervates the **gluteus medius, gluteus minimus**, and **tensor fasciae latae muscles**, which are involved in hip abduction and internal rotation.
- Its blockade would not relieve hip flexion or thigh muscle cramps.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (hip extension, knee flexion) and all muscles below the knee.
- While it affects leg muscles, it does not directly control the muscles causing **hip flexion and increased thigh tone** in this context.
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles** of the thigh (adductor longus, brevis, magnus, gracilis), leading to hip adduction.
- Blocking this nerve would not address hip flexion or the increased tone in the quadriceps muscles described.
Surface anatomy for nerve blocks US Medical PG Question 4: A 14-year-old boy is brought to the emergency department because of acute left-sided chest pain and dyspnea following a motor vehicle accident. His pulse is 122/min and blood pressure is 85/45 mm Hg. Physical examination shows distended neck veins and tracheal displacement to the right side. The left chest is hyperresonant to percussion and there are decreased breath sounds. This patient would most benefit from needle insertion at which of the following anatomical sites?
- A. 5th left intercostal space along the midclavicular line
- B. 8th left intercostal space along the posterior axillary line
- C. 2nd left intercostal space along the midclavicular line (Correct Answer)
- D. Subxiphoid space in the left sternocostal margin
- E. 5th left intercostal space along the midaxillary line
Surface anatomy for nerve blocks Explanation: ***2nd left intercostal space along the midclavicular line***
- The patient's symptoms (chest pain, dyspnea, hypotension, distended neck veins, tracheal deviation, hyperresonance, and decreased breath sounds on the left) are classic signs of a **tension pneumothorax**.
- Immediate treatment for **tension pneumothorax** involves needle decompression at the **2nd intercostal space** in the midclavicular line to relieve pressure and restore hemodynamic stability.
*5th left intercostal space along the midclavicular line*
- This location is typically used for **chest tube insertion** in a more controlled setting, not for emergent needle decompression of a tension pneumothorax.
- While it's a safe location for pleural access, it is not the **first-line site** for immediate life-saving decompression.
*8th left intercostal space along the posterior axillary line*
- This site is too low and posterior for effective needle decompression of a tension pneumothorax, which requires rapid access to the **apex of the lung**.
- It is more commonly used for **thoracentesis** to drain fluid from the pleural cavity.
*Subxiphoid space in the left sternocostal margin*
- This location is primarily used for **pericardiocentesis** to drain fluid from the pericardial sac in cases of cardiac tamponade.
- It is not appropriate for addressing a **pneumothorax**, which involves air in the pleural space.
*5th left intercostal space along the midaxillary line*
- This site is a common alternative for **chest tube insertion** but is not the preferred or most immediate site for needle decompression of a tension pneumothorax.
- While it offers pleural access, the **2nd intercostal space** anteriorly is chosen for expediency and safety in an emergency.
Surface anatomy for nerve blocks US Medical PG Question 5: A 61-year-old woman comes to the physician for a follow-up examination 1 week after undergoing right-sided radical mastectomy and axillary lymph node dissection for breast cancer. She says that she has been unable to comb her hair with her right hand since the surgery. Physical examination shows shoulder asymmetry. She is unable to abduct her right arm above 90 degrees. When she pushes against a wall, there is protrusion of the medial aspect of the right scapula. Injury to which of the following nerves is the most likely cause of this patient's condition?
- A. Long thoracic nerve (Correct Answer)
- B. Thoracodorsal nerve
- C. Axillary nerve
- D. Suprascapular nerve
- E. Upper trunk of the brachial plexus
Surface anatomy for nerve blocks Explanation: ***Long thoracic nerve***
- Injury to the **long thoracic nerve** leads to paralysis of the **serratus anterior muscle**, causing **scapular winging** (protrusion of the medial scapula) especially when pushing against a wall.
- The serratus anterior is crucial for **scapular protraction** and stabilizing the scapula during **abduction of the arm above 90 degrees**, explaining her inability to comb her hair.
*Thoracodorsal nerve*
- The **thoracodorsal nerve** innervates the **latissimus dorsi muscle**, which is responsible for **adduction**, extension, and internal rotation of the arm.
- Injury to this nerve would primarily affect these movements, not shoulder abduction above 90 degrees or scapular winging.
*Axillary nerve*
- The **axillary nerve** innervates the **deltoid muscle** and **teres minor**.
- Damage would primarily result in impaired **arm abduction up to 90 degrees** and loss of sensation over the lateral shoulder, but not scapular winging.
*Suprascapular nerve*
- The **suprascapular nerve** supplies the **supraspinatus** and **infraspinatus muscles**, which are involved in the initiation of arm abduction and external rotation, respectively.
- Injury would cause weakness in these movements and shoulder pain, but not scapular winging.
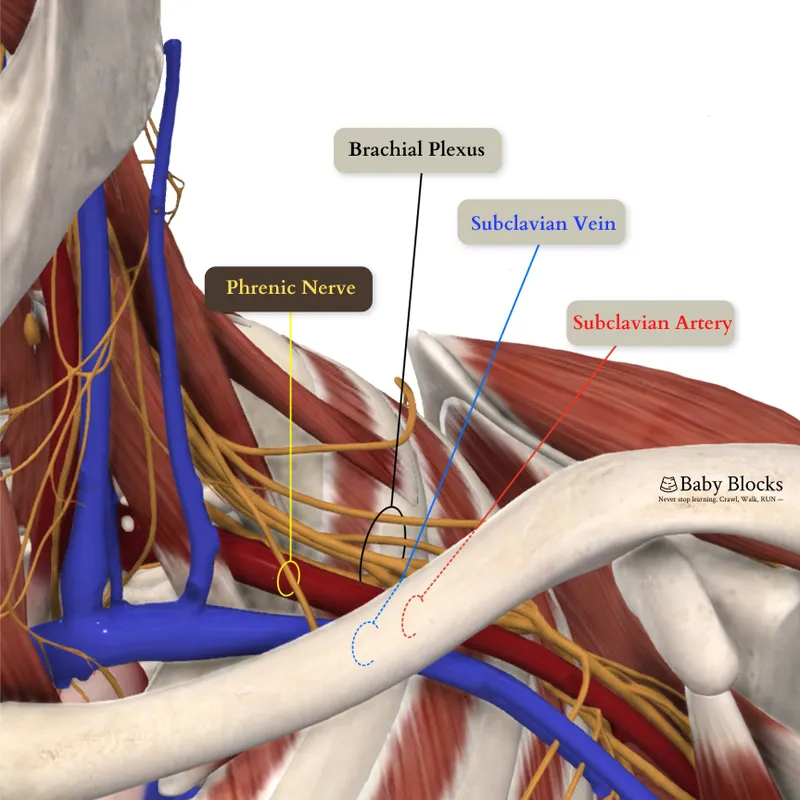
*Upper trunk of the brachial plexus*
- Injury to the **upper trunk of the brachial plexus** (C5-C6) affects several nerves and muscles, leading to conditions like **Erb's palsy**.
- While it can impair shoulder function and abduction, the specific finding of scapular winging points more directly to long thoracic nerve damage rather than a generalized upper trunk injury, as the long thoracic nerve (C5-C7) is often spared in classic Erb's palsy.
Surface anatomy for nerve blocks US Medical PG Question 6: A 41-year-old woman presents with back pain for the past 2 days. She says that the pain radiates down along the posterior right thigh and leg. She says the pain started suddenly after lifting a heavy box 2 days ago. Past medical history is irrelevant. Physical examination reveals a straight leg raise (SLR) test restricted to 30°, inability to walk on her toes, decreased sensation along the lateral border of her right foot, and diminished ankle jerk on the same side. Which of the following nerve roots is most likely compressed?
- A. Fourth lumbar nerve root (L4)
- B. Second sacral nerve root (S2)
- C. Third sacral nerve root (S3)
- D. Fifth lumbar nerve root (L5)
- E. First sacral nerve root (S1) (Correct Answer)
Surface anatomy for nerve blocks Explanation: ***First sacral nerve root (S1)***
- **Inability to walk on toes** (weakness of gastrocnemius and soleus), **decreased sensation along the lateral border of the foot**, and a **diminished ankle jerk** are classic signs of S1 radiculopathy.
- The radiating pain down the posterior leg, restricted straight leg raise due to a sudden onset after lifting, points towards a **disc herniation** compressing the S1 nerve root.
*Fourth lumbar nerve root (L4)*
- Compression of L4 typically causes **weakness in knee extension** (quadriceps), diminished patellar reflex, and sensory loss over the medial aspect of the shin.
- The patient's symptoms (inability to walk on toes, diminished ankle jerk) are not consistent with L4 nerve root involvement.
*Second sacral nerve root (S2)*
- S2 radiculopathy primarily affects sensation in the posterior thigh and calf and can cause **weakness in knee flexion** and **plantarflexion**, but the complete constellation of symptoms (especially ankle jerk reflex) is more indicative of S1.
- Isolated S2 compression without S1 involvement is less common with these specific signs.
*Third sacral nerve root (S3)*
- S3 nerve root compression typically presents with **perineal numbness** and issues with bowel or bladder function due to its involvement in these functions.
- The described motor and sensory deficits are not characteristic of S3 radiculopathy.
*Fifth lumbar nerve root (L5)*
- L5 radiculopathy is characterized by **weakness in foot dorsiflexion** (foot drop) and toe extension, leading to inability to walk on heels, and sensory loss on the dorsum of the foot.
- While L5 compression can cause radiating pain and a restricted straight leg raise, the specific deficit of **inability to walk on toes** and a **diminished ankle jerk** are not typical of L5 involvement.
Surface anatomy for nerve blocks US Medical PG Question 7: A 23-year-old man is brought to the emergency department by ambulance following a motor vehicle accident. He was pinned between 2 cars for several hours. The patient has a history of asthma. He uses an albuterol inhaler intermittently. The patient was not the driver, and admits to having a few beers at a party prior to the accident. His vitals in the ambulance are stable. Upon presentation to the emergency department, the patient is immediately brought to the operating room for evaluation and surgical intervention. It is determined that the patient’s right leg has a Gustilo IIIC injury in the mid-shaft of the tibia with a severely comminuted fracture. The patient’s left leg suffered a similar injury but with damage to the peroneal nerve. The anesthesiologist begins to induce anesthesia. Which of the following agents would be contraindicated in this patient?
- A. Halothane
- B. Propofol
- C. Etomidate
- D. Succinylcholine (Correct Answer)
- E. Neostigmine
Surface anatomy for nerve blocks Explanation: ***Succinylcholine***
- Given the history of the patient being pinned between two cars for several hours, there is a significant risk of **rhabdomyolysis** and subsequent hyperkalemia.
- **Succinylcholine**, a depolarizing neuromuscular blocker, can cause a sudden and significant release of potassium from muscle cells, leading to **life-threatening hyperkalemia** in patients with rhabdomyolysis or crush injuries.
*Halothane*
- While **halothane** has been associated with **malignant hyperthermia**, the patient's history does not directly suggest an increased risk for this condition here.
- It also has a bronchodilating effect, which could be beneficial for a patient with a history of **asthma**.
*Propofol*
- **Propofol** is a commonly used intravenous anesthetic for induction and maintenance, providing rapid onset and recovery.
- There are generally no specific contraindications for propofol in a patient with a crush injury or asthma.
*Etomidate*
- **Etomidate** is an intravenous anesthetic agent known for its **cardiovascular stability**, making it a good choice for hemodynamically unstable patients.
- It can cause adrenal suppression, but this is usually a concern with prolonged infusions, not a single induction dose.
*Neostigmine*
- **Neostigmine** is an acetylcholinesterase inhibitor used to reverse the effects of non-depolarizing neuromuscular blockers.
- It is not an induction agent and would not be used at the beginning of anesthesia induction.
Surface anatomy for nerve blocks US Medical PG Question 8: A previously healthy 33-year-old woman comes to the physician because of pain and sometimes numbness in her right thigh for the past 2 months. She reports that her symptoms are worse when walking or standing and are better while sitting. Three months ago, she started going to a fitness class a couple times a week. She is 163 cm (5 ft 4 in) tall and weighs 88 kg (194 lb); BMI is 33.1 kg/m2. Her vital signs are within normal limits. Examination of the skin shows no abnormalities. Sensation to light touch is decreased over the lateral aspect of the right anterior thigh. Muscle strength is normal. Tapping the right inguinal ligament leads to increased numbness of the affected thigh. The straight leg test is negative. Which of the following is the most appropriate next step in management of this patient?
- A. Advise patient to wear looser pants (Correct Answer)
- B. Reduction of physical activity
- C. MRI of the lumbar spine
- D. X-ray of the hip
- E. Blood work for inflammatory markers
Surface anatomy for nerve blocks Explanation: ***Advise patient to wear looser pants***
- This patient presents with symptoms consistent with **meralgia paresthetica**, a condition caused by compression of the **lateral femoral cutaneous nerve (LFCN)**. Modifying clothing or belts that compress the inguinal ligament can relieve pressure on the nerve.
- Her increased weight, a recent increase in physical activity, and a positive Tinel's sign at the inguinal ligament (tapping leads to increased numbness) support this diagnosis.
*Reduction of physical activity*
- While excessive physical activity can contribute to meralgia paresthetica, simply reducing it without addressing the underlying compression might not fully resolve symptoms.
- The patient has recently increased physical activity, which could be a contributing factor, but it's not the primary or most direct intervention for nerve compression.
*MRI of the lumbar spine*
- An MRI of the lumbar spine would be considered if there were signs of **radiculopathy** or other spinal pathology, such as weakness, reflex changes, or a positive straight leg test, which are absent here.
- The symptoms are localized to the distribution of the LFCN, and the physical exam points away from a central spinal cause.
*X-ray of the hip*
- An X-ray of the hip would be indicated for suspected **hip joint pathology** or **bony abnormalities**, which are not suggested by the patient's symptoms (pain and numbness in the thigh, not hip joint pain).
- Meralgia paresthetica is a nerve entrapment syndrome, not a structural issue of the hip joint.
*Blood work for inflammatory markers*
- Inflammatory markers like **ESR** or **CRP** would be relevant if an **inflammatory arthritis**, infection, or systemic inflammatory condition was suspected, but the patient's symptoms are purely neurological and localized.
- There is no clinical evidence of inflammation, fever, or joint swelling to suggest an underlying inflammatory process.
Surface anatomy for nerve blocks US Medical PG Question 9: Where does the only cranial nerve without a thalamic relay nucleus enter the skull?
- A. Superior orbital fissure
- B. Internal auditory meatus
- C. Foramen rotundum
- D. Jugular foramen
- E. Cribriform plate (Correct Answer)
Surface anatomy for nerve blocks Explanation: ***Cribriform plate***
- The **olfactory nerve (CN I)** is the only cranial nerve that does not have a thalamic relay nucleus before reaching the cerebral cortex.
- It passes through the **cribriform plate** of the ethmoid bone to reach the olfactory bulbs.
*Superior orbital fissure*
- This opening transmits the **oculomotor (CN III), trochlear (CN IV), ophthalmic division of trigeminal (CN V1)**, and **abducens (CN VI)** nerves.
- These nerves all have sensory or motor components that relay through the thalamus, directly or indirectly.
*Internal auditory meatus*
- This canal transmits the **facial (CN VII)** and **vestibulocochlear (CN VIII)** nerves.
- The vestibulocochlear nerve's auditory pathway involves a thalamic relay in the **medial geniculate nucleus**.
*Foramen rotundum*
- The **maxillary division of the trigeminal nerve (CN V2)** passes through the foramen rotundum.
- Sensory information carried by CN V2 relays through the **thalamus**.
*Jugular foramen*
- This opening transmits the **glossopharyngeal (CN IX), vagus (CN X)**, and **accessory (CN XI)** nerves.
- Sensory components of these nerves, particularly taste and visceral sensation, involve thalamic nuclei.
Surface anatomy for nerve blocks US Medical PG Question 10: A 72-year-old male presents to a cardiac surgeon for evaluation of severe aortic stenosis. He has experienced worsening dyspnea with exertion over the past year. The patient also has a history of poorly controlled hypertension, diabetes mellitus, and hyperlipidemia. An echocardiogram revealed a thickened calcified aortic valve. The surgeon is worried that the patient will be a poor candidate for open heart surgery and decides to perform a less invasive transcatheter aortic valve replacement. In order to perform this procedure, the surgeon must first identify the femoral pulse just inferior to the inguinal ligament and insert a catheter into the vessel in order to gain access to the arterial system. Which of the following structures is immediately lateral to this structure?
- A. Lymphatic vessels
- B. Femoral vein
- C. Sartorius muscle
- D. Pectineus muscle
- E. Femoral nerve (Correct Answer)
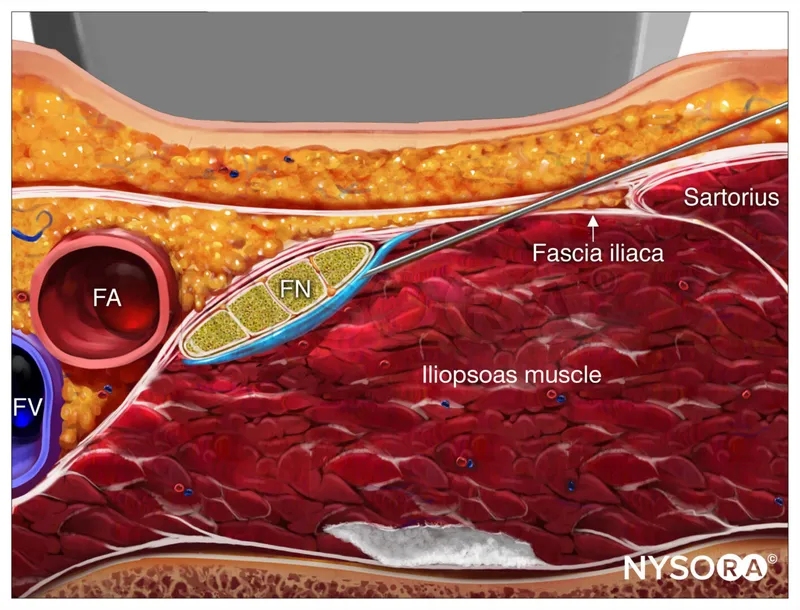
Surface anatomy for nerve blocks Explanation: ***Femoral nerve***
- The **femoral nerve** lies lateral to the **femoral artery** within the **femoral triangle**.
- The order of structures from **lateral to medial** under the inguinal ligament is remembered by the mnemonic **NAVEL**: **N**erve, **A**rtery, **V**ein, **E**mpty space, **L**ymphatics.
*Lymphatic vessels*
- **Lymphatic vessels** and nodes are located most medially within the femoral triangle, medial to the femoral vein.
- This position is not immediately lateral to the femoral artery.
*Femoral vein*
- The **femoral vein** is located immediately medial to the **femoral artery**.
- It would not be found immediately lateral to the femoral artery.
*Sartorius muscle*
- The **sartorius muscle** forms the lateral boundary of the **femoral triangle** but is not immediately adjacent and lateral to the femoral artery within the triangle itself.
- The femoral nerve is enclosed within the iliopsoas fascial compartment, which runs deep to the sartorius.
*Pectineus muscle*
- The **pectineus muscle** forms part of the floor of the **femoral triangle**, but it is deep to the neurovascular structures.
- It is not immediately lateral to the femoral artery.
More Surface anatomy for nerve blocks US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.