Surface anatomy for clinical procedures US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Surface anatomy for clinical procedures. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Surface anatomy for clinical procedures US Medical PG Question 1: A 34-year-old patient presents with severe pain in the right upper quadrant that radiates to the right shoulder. During laparoscopic cholecystectomy, which of the following anatomical spaces must be carefully identified to prevent bile duct injury?
- A. Foramen of Winslow
- B. Lesser sac
- C. Calot's triangle (Correct Answer)
- D. Morrison's pouch
Surface anatomy for clinical procedures Explanation: ***Calot's triangle***
- **Calot's triangle** is the critical anatomical landmark containing the **cystic artery** and **cystic duct**, whose proper identification is essential to prevent injury to the hepatic artery or bile ducts during cholecystectomy.
- Its boundaries are the **cystic duct** (lateral), the **common hepatic duct** (medial), and the **inferior border of the liver** (superior, sometimes described as the cystic artery).
*Foramen of Winslow*
- The **Foramen of Winslow** (epiploic foramen) is an opening connecting the **greater and lesser sacs** of the peritoneal cavity.
- It is not directly relevant to identifying structures during cholecystectomy, but rather to accessing the lesser sac or for surgical procedures involving structures like the portal triad.
*Lesser sac*
- The **lesser sac** (omental bursa) is a peritoneal cavity posterior to the stomach and lesser omentum.
- It is explored in procedures involving the pancreas, posterior gastric wall, or for assessing fluid collections, but not for direct identification of cystic structures during standard cholecystectomy.
*Morrison's pouch*
- **Morrison's pouch** is the **hepatorenal recess**, a potential space between the posterior aspect of the liver and the right kidney and adrenal gland.
- It is a common site for **fluid accumulation** (e.g., ascites, blood) but is not directly incised or dissected for preventing bile duct injury during cholecystectomy.
Surface anatomy for clinical procedures US Medical PG Question 2: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Surface anatomy for clinical procedures Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
Surface anatomy for clinical procedures US Medical PG Question 3: During a thoracotomy procedure, a surgeon needs to access the posterior mediastinum. Which of the following structures forms the anterior boundary of the posterior mediastinum?
- A. Descending thoracic aorta
- B. Pericardial sac (Correct Answer)
- C. Azygos vein
- D. Thoracic vertebrae
- E. Sternum
Surface anatomy for clinical procedures Explanation: ***Pericardial sac***
- The **pericardial sac** (and the diaphragm, inferiorly) forms the anterior boundary of the **posterior mediastinum** [1].
- This anatomical relationship is crucial for surgeons during thoracotomy to distinguish between the middle and posterior mediastinal compartments [1].
*Descending thoracic aorta*
- The **descending thoracic aorta** is a large vessel located *within* the posterior mediastinum itself, typically running along its left side [2].
- Therefore, it is a content of the posterior mediastinum, not a boundary.
*Azygos vein*
- The **azygos vein** is also a major structure *within* the posterior mediastinum, running along the right side of the vertebral column.
- It is a content, not a boundary, of this compartment.
*Thoracic vertebrae*
- The **thoracic vertebrae** form the *posterior* boundary of the posterior mediastinum [1].
- This anatomical landmark gives the posterior mediastinum its name and defines its dorsal limit.
Surface anatomy for clinical procedures US Medical PG Question 4: A 27-year-old man presents to the emergency department for altered mental status. The patient was found napping in a local market and brought to the hospital. The patient has a past medical history of polysubstance abuse and is homeless. His temperature is 104°F (40.0°C), blood pressure is 100/52 mmHg, pulse is 133/min, respirations are 25/min, and oxygen saturation is 99% on room air. Physical exam is notable for an altered man. Cardiopulmonary exam reveals a murmur over the left lower sternal border. A bedside ultrasound reveals a vegetation on the tricuspid valve. The patient is ultimately started on IV fluids, norepinephrine, vasopressin, vancomycin, and piperacillin-tazobactam. A central line is immediately placed in the internal jugular vein and the femoral vein secondary to poor IV access. Cardiothoracic surgery subsequently intervenes to remove the vegetation. While recovering in the ICU, days 3-5 are notable for an improvement in the patient’s symptoms. Two additional peripheral IVs are placed while in the ICU on day 5, and the femoral line is removed. On day 6, the patient's fever and hemodynamic status worsen. Though he is currently responding and not complaining of any symptoms including headache, photophobia, neck stiffness, or pain, he states he is feeling weak. Jolt accentuation of headache is negative and his abdominal exam is benign. A chest radiograph, urinalysis, and echocardiogram are unremarkable though the patient’s blood cultures are positive when drawn. Which of the following is the best next step in management?
- A. Add micafungin to the patient’s antibiotics
- B. Perform a lumbar puncture
- C. Remove all peripheral IV’s and send for cultures
- D. Add cefepime to the patient’s antibiotics
- E. Remove the central line and send for cultures (Correct Answer)
Surface anatomy for clinical procedures Explanation: **Correct: Remove the central line and send for cultures**
- The patient's worsening fever and hemodynamic instability on day 6, despite initial improvement, raise suspicion for a **catheter-related bloodstream infection (CRBSI)**, especially given the history of central line placement.
- **Prompt removal of the catheter** and sending the tip for culture is crucial for diagnosis and treatment of potential CRBSI, as the source of infection often resides within the biofilm on the catheter.
*Incorrect: Remove all peripheral IV's and send for cultures*
- While **peripheral IVs** can be a source of infection, the central line was placed earlier and is associated with a much higher risk of serious infection, especially in a critically ill patient.
- The patient's initial improvement followed by deterioration points more towards a **central line-associated infection** rather than new peripheral IVs placed only on day 5.
*Incorrect: Perform a lumbar puncture*
- Although the patient has altered mental status, the absence of focal neurological deficits, headache, photophobia, and neck stiffness, along with a negative **Jolt accentuation of headache**, makes **meningitis** less likely as the primary cause of deterioration.
- The more immediate and likely cause of worsening sepsis in this context is a **catheter-related infection**.
*Incorrect: Add micafungin to the patient's antibiotics*
- Adding an antifungal agent such as **micafungin** would be considered if there was a strong suspicion of a fungal infection, which is not indicated by the current blood cultures or clinical picture.
- Empiric antifungal therapy is typically reserved for patients with persistent fever refractory to broad-spectrum antibiotics, known fungal exposure, or specific risk factors.
*Incorrect: Add cefepime to the patient's antibiotics*
- The patient is already on **vancomycin and piperacillin-tazobactam**, which provides broad-spectrum coverage for both gram-positive and gram-negative bacteria, including *Pseudomonas aeruginosa*.
- Adding **cefepime** would broaden gram-negative coverage further but is usually unnecessary unless the current regimen is failing due to specific resistant organisms, and the more likely source of infection should be addressed first.
Surface anatomy for clinical procedures US Medical PG Question 5: A 60-year-old woman is rushed to the emergency room after falling on her right elbow while walking down the stairs. She cannot raise her right arm. Her vital signs are stable, and the physical examination reveals loss of sensation over the upper lateral aspect of the right arm and shoulder. A radiologic evaluation shows a fracture of the surgical neck of the right humerus. Which of the following muscles is supplied by the nerve that is most likely damaged?
- A. Teres minor (Correct Answer)
- B. Teres major
- C. Subscapularis
- D. Infraspinatus
- E. Supraspinatus
Surface anatomy for clinical procedures Explanation: ***Teres minor***
- A fracture of the **surgical neck of the humerus** often damages the **axillary nerve**, which innervates the **teres minor**.
- The axillary nerve also supplies the **deltoid muscle** and provides cutaneous sensation to the **upper lateral arm**, consistent with the patient's sensory loss.
*Teres major*
- This muscle is innervated by the **lower subscapular nerve**, which is less likely to be damaged in a surgical neck fracture.
- Its primary action is **adduction** and **internal rotation** of the arm.
*Subscapularis*
- The **subscapularis** is innervated by the **upper and lower subscapular nerves**.
- While it contributes to internal rotation, its nerve supply is typically protected in this type of fracture.
*Infraspinatus*
- The **infraspinatus** muscle is innervated by the **suprascapular nerve**.
- This nerve is generally not affected by a fracture of the surgical neck of the humerus.
*Supraspinatus*
- Similar to the infraspinatus, the **supraspinatus** is also innervated by the **suprascapular nerve**.
- Damage to this nerve due to a humeral surgical neck fracture is uncommon.
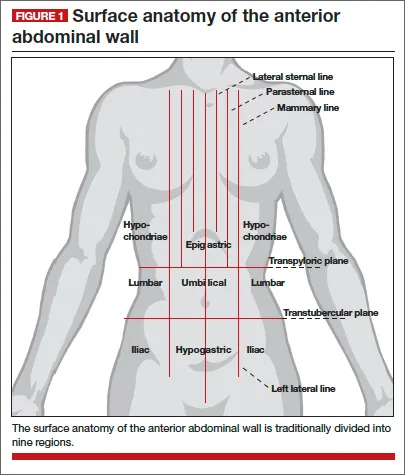
Surface anatomy for clinical procedures US Medical PG Question 6: A 27-year-old woman presents with acute abdominal pain in her right upper quadrant. The pain came on suddenly while she was eating dinner. After this pain she began feeling dizzy and came to the emergency department. In the ED, her blood pressure is 75/40 mmHg, pulse is 100/minute, and she is afebrile. On physical exam, she feels too light-headed to ambulate. She demonstrates normal bowel sounds with tenderness upon palpation in the right upper quadrant. The patient is deemed too unstable for imaging. An abdominal radiograph and CT are reviewed from a recent previous visit to the ED for mild abdominal pain, and are shown in Figures A and B, respectively. Which of the following specific additional findings in her history supports the most likely diagnosis?
- A. Symptoms that began after a fatty meal
- B. Use of oral contraceptives (OCPs) for birth control (Correct Answer)
- C. A 15 pack/year history of smoking
- D. A history of Epstein-Barr virus and participation in rugby
- E. An extensive history of sexually transmitted diseases (STDs) and pelvic inflammatory disease (PID)
Surface anatomy for clinical procedures Explanation: ***Use of oral contraceptives (OCPs) for birth control***
- The patient's presentation with acute right upper quadrant pain, **hemodynamic instability** (BP 75/40 mmHg, pulse 100/minute, dizziness), and previous imaging showing a hepatic lesion (implied by the question context though images aren't provided) strongly suggests a ruptured **hepatic adenoma**.
- **Oral contraceptive pill (OCP) use** is a well-established risk factor for the development and rupture of hepatic adenomas due to their estrogen content, which promotes growth.
*Symptoms that began after a fatty meal*
- Acute right upper quadrant pain exacerbated by a **fatty meal** is classic for **cholecystitis** or **biliary colic**.
- However, the patient's **hemodynamic instability** is not typical for uncomplicated cholecystitis, and hepatic adenoma rupture is a more fitting explanation for the sudden onset of profound shock.
*A 15 pack/year history of smoking*
- Smoking is a risk factor for various abdominal conditions, including **peptic ulcer disease** and certain **malignancies**.
- It is not a direct risk factor for **hepatic adenoma rupture** and does not explain the acute, life-threatening presentation in this young woman as well as OCP use.
*A history of Epstein-Barr virus and participation in rugby*
- A history of Epstein-Barr virus (EBV) and contact sports like rugby is associated with an increased risk of **splenic rupture**, especially if splenomegaly is present.
- While splenic rupture can cause acute abdominal pain and hypovolemic shock, the pain would typically be in the **left upper quadrant**, not the right.
*An extensive history of sexually transmitted diseases (STDs) and pelvic inflammatory disease (PID)*
- STDs and PID are risk factors for **ectopic pregnancy** (which can cause acute abdominal pain and rupture, leading to shock) and **Fitz-Hugh-Curtis syndrome** (perihepatitis causing RUQ pain).
- However, the patient's age and sex would make these considerations relevant, but the specific localization of pain to the right upper quadrant and the strong association with OCPs point more directly to a hepatic pathology.
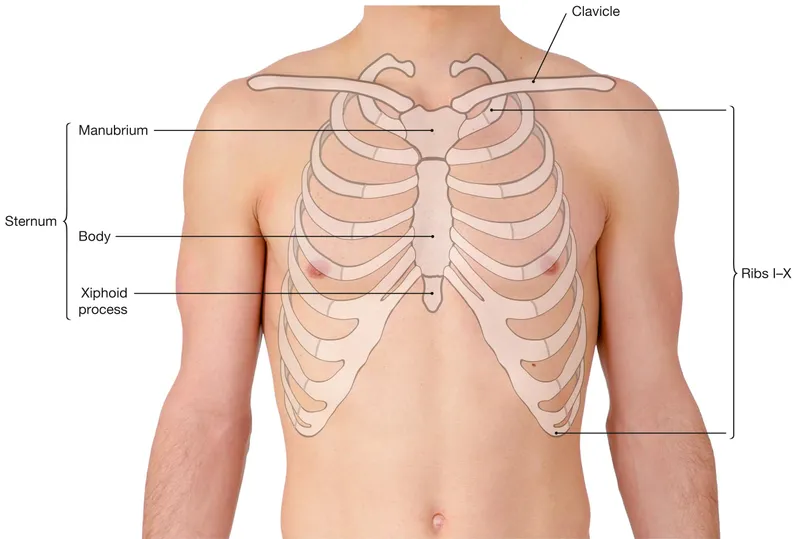
Surface anatomy for clinical procedures US Medical PG Question 7: A 50-year-old man presents with severe chest pain for a week. His pain increases with breathing and is localized to the right. He has tried over-the-counter medications at home, but they did not help. The patient has a 20-pack-year smoking history and currently smokes 2 packs of cigarettes daily, and he drinks 3 to 4 cans of beer daily before dinner. His temperature is 39.1°C (102.3°F), blood pressure is 127/85 mm Hg, pulse is 109/min, and respirations are 20/min. Respiratory examination shows dullness to percussion from the 7th rib inferiorly at the right midaxillary line, decreased vocal tactile fremitus, and diminished breath sounds in the same area. Chest radiograph is shown in the image. The patient is prepared for thoracocentesis. Which of the following locations would be the most appropriate for insertion of a chest tube?
- A. Below the inferior border of the 7th rib in the midaxillary line
- B. Above the superior border of the 8th rib in the midaxillary line (Correct Answer)
- C. Above the superior border of the 5th rib in the midclavicular line
- D. Below the inferior border of the 5th rib in the midaxillary line
- E. Above the superior border of the 7th rib in the midclavicular line
Surface anatomy for clinical procedures Explanation: ***Above the superior border of the 8th rib in the midaxillary line***
- The patient presents with symptoms and signs suggestive of a **pleural effusion** (dullness to percussion, decreased fremitus, diminished breath sounds) and potentially an **empyema** given the fever and lung consolidation on the radiograph.
- Thoracocentesis should be performed in the **midaxillary line** between the 6th and 9th ribs to avoid injuring the **diaphragm and abdominal organs**, which can rise as high as the 5th intercostal space during expiration. To prevent damage to the neurovascular bundle that runs along the inferior border of the ribs, the needle should be inserted just **above the superior border** of the rib below the chosen intercostal space.
*Below the inferior border of the 7th rib in the midaxillary line*
- Inserting below the inferior border of the 7th rib increases the risk of injuring the **neurovascular bundle** that runs along the inferior rib margin.
- Such placement might also be too low, increasing the risk of penetrating the **diaphragm** or **abdominal organs**. This location would correspond to the 8th intercostal space, but the 'below inferior border' part is incorrect.
*Above the superior border of the 5th rib in the midclavicular line*
- The **midclavicular line** is typically used for needle decompression of a tension pneumothorax (2nd intercostal space) but is not the preferred site for thoracocentesis due to the risk of striking the lung parenchyma or internal mammary artery.
- Even if considering a pneumothorax, the 5th intercostal space in the midclavicular line is not the standard site, and an effusion is indicated here.
*Below the inferior border of the 5th rib in the midaxillary line*
- Inserting below the inferior border of the 5th rib, similar to option A, risks injury to the **neurovascular bundle**.
- While in the midaxillary line, the 5th rib might be too high for an effusion, and the technique of inserting below the inferior border is incorrect.
*Above the superior border of the 7th rib in the midclavicular line*
- The **midclavicular line** is generally avoided for thoracocentesis of effusions due to the risks mentioned previously and poor drainage if the effusion is posterior.
- The 7th intercostal space in the midclavicular line is also a non-standard and less safe location for this procedure.
Surface anatomy for clinical procedures US Medical PG Question 8: A 68-year-old man comes to the physician because of a 4-month history of difficulty swallowing. During this time, he has also had a 7-kg (15-lb) weight loss. Esophagogastroduodenoscopy shows an exophytic mass in the distal third of the esophagus. Histological examination of a biopsy specimen shows a well-differentiated adenocarcinoma. The patient is scheduled for surgical resection of the tumor. During the procedure, the surgeon damages a structure that passes through the diaphragm along with the esophagus at the level of the tenth thoracic vertebra (T10). Which of the following structures was most likely damaged?
- A. Azygos vein
- B. Vagus nerve (Correct Answer)
- C. Right phrenic nerve
- D. Inferior vena cava
- E. Thoracic duct
Surface anatomy for clinical procedures Explanation: ***Vagus nerve***
- The **esophagus** passes through the diaphragm at the level of the **T10 vertebra**, accompanied by the **anterior and posterior vagal trunks**. Damage to these nerves is a known complication of esophageal surgery.
- The vagus nerves provide **parasympathetic innervation** to the gastrointestinal tract, and their close proximity to the esophagus makes them vulnerable during tumor resection.
*Azygos vein*
- The **azygos vein** typically passes through the diaphragm at the level of **T12** through the **aortic hiatus**, not with the esophagus at T10.
- It drains into the superior vena cava and is located more posteriorly in the mediastinum.
*Right phrenic nerve*
- The **right phrenic nerve** passes through the diaphragm with the **inferior vena cava** at the level of **T8**, innervating the diaphragm.
- It is located more anteriorly and laterally to the esophagus, making direct damage during esophageal surgery less likely than the vagus nerves.
*Inferior vena cava*
- The **inferior vena cava (IVC)** passes through its own opening in the central tendon of the diaphragm at the level of **T8**, not with the esophagus at T10.
- Damage to the IVC would result in significant hemorrhage and is typically a separate surgical concern.
*Thoracic duct*
- The **thoracic duct** passes through the **aortic hiatus** at the level of **T12** along with the aorta, collecting lymph from most of the body.
- Its location makes it less likely to be damaged during a standard esophageal resection at T10 compared to the vagus nerves.
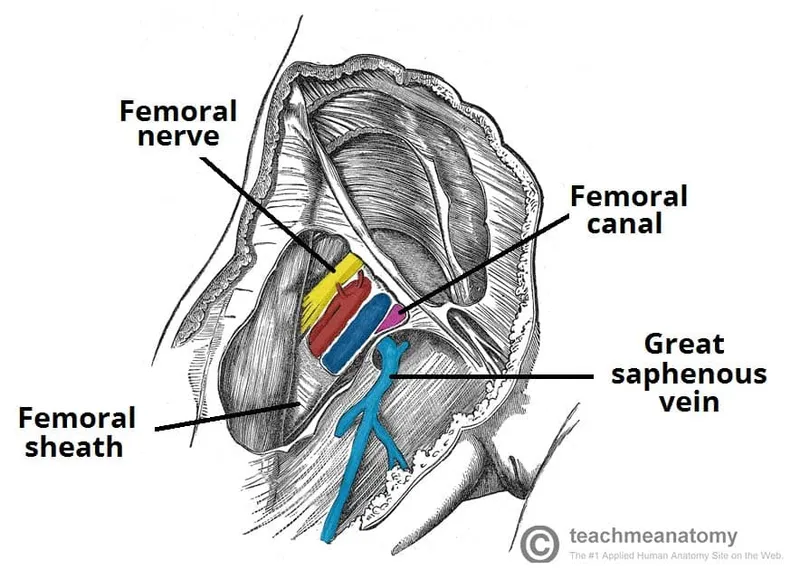
Surface anatomy for clinical procedures US Medical PG Question 9: A 72-year-old male presents to a cardiac surgeon for evaluation of severe aortic stenosis. He has experienced worsening dyspnea with exertion over the past year. The patient also has a history of poorly controlled hypertension, diabetes mellitus, and hyperlipidemia. An echocardiogram revealed a thickened calcified aortic valve. The surgeon is worried that the patient will be a poor candidate for open heart surgery and decides to perform a less invasive transcatheter aortic valve replacement. In order to perform this procedure, the surgeon must first identify the femoral pulse just inferior to the inguinal ligament and insert a catheter into the vessel in order to gain access to the arterial system. Which of the following structures is immediately lateral to this structure?
- A. Lymphatic vessels
- B. Femoral vein
- C. Sartorius muscle
- D. Pectineus muscle
- E. Femoral nerve (Correct Answer)
Surface anatomy for clinical procedures Explanation: ***Femoral nerve***
- The **femoral nerve** lies lateral to the **femoral artery** within the **femoral triangle**.
- The order of structures from **lateral to medial** under the inguinal ligament is remembered by the mnemonic **NAVEL**: **N**erve, **A**rtery, **V**ein, **E**mpty space, **L**ymphatics.
*Lymphatic vessels*
- **Lymphatic vessels** and nodes are located most medially within the femoral triangle, medial to the femoral vein.
- This position is not immediately lateral to the femoral artery.
*Femoral vein*
- The **femoral vein** is located immediately medial to the **femoral artery**.
- It would not be found immediately lateral to the femoral artery.
*Sartorius muscle*
- The **sartorius muscle** forms the lateral boundary of the **femoral triangle** but is not immediately adjacent and lateral to the femoral artery within the triangle itself.
- The femoral nerve is enclosed within the iliopsoas fascial compartment, which runs deep to the sartorius.
*Pectineus muscle*
- The **pectineus muscle** forms part of the floor of the **femoral triangle**, but it is deep to the neurovascular structures.
- It is not immediately lateral to the femoral artery.
Surface anatomy for clinical procedures US Medical PG Question 10: An 18-year-old man is brought to the emergency department 30 minutes after being stabbed in the chest during a fight. He has no other injuries. His pulse is 120/min, blood pressure is 90/60 mm Hg, and respirations are 22/min. Examination shows a 4-cm deep, straight stab wound in the 4th intercostal space 2 cm medial to the right midclavicular line. The knife most likely passed through which of the following structures?
- A. Serratus anterior muscle, pleura, inferior vena cava
- B. External oblique muscle, superior epigastric artery, azygos vein
- C. Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver
- D. Intercostal muscles, internal thoracic artery, right heart
- E. Pectoral fascia, transversus thoracis muscle, right lung (Correct Answer)
Surface anatomy for clinical procedures Explanation: ***Pectoral fascia, transversus thoracis muscle, right lung***
* The stab wound is in the **4th intercostal space**, 2 cm medial to the right midclavicular line, placing it over the anterior chest wall. This trajectory would first penetrate the **pectoral fascia**.
* Deeper structures in this region include the **transversus thoracis muscle** and, given the depth, the **right lung** as it extends superiorly behind the anterior chest wall.
* *Serratus anterior muscle, pleura, inferior vena cava*
* The **serratus anterior muscle** is more laterally positioned, typically covering the side of the rib cage.
* The **inferior vena cava** is located more medially and posteriorly within the mediastinum, deep to the diaphragm, making it an unlikely target for an anterior 4th intercostal stab.
* *External oblique muscle, superior epigastric artery, azygos vein*
* The **external oblique muscle** is part of the abdominal wall and would not be penetrated in the 4th intercostal space.
* The **superior epigastric artery** is lower, typically extending into the abdominal wall, and the **azygos vein** is in the posterior mediastinum, not in the path of this superficial anterior stab wound.
* *Pectoralis minor muscle, dome of the diaphragm, right lobe of the liver*
* The **pectoralis minor muscle** is located deep to the pectoralis major, which would be penetrated. However, a stab at the 4th intercostal space would be too high to directly involve the **dome of the diaphragm** or the **right lobe of the liver**, which are typically below the 5th intercostal space, especially in forced expiration.
* *Intercostal muscles, internal thoracic artery, right heart*
* The **intercostal muscles** would certainly be traversed.
* However, the **internal thoracic artery** runs paramedially (about 1-2 cm from the sternum), and getting to the **right heart** would require a more medial and deeper trajectory, potentially causing immediate tamponade or severe hemorrhage.
More Surface anatomy for clinical procedures US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.