Lower limb surface landmarks US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lower limb surface landmarks. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lower limb surface landmarks US Medical PG Question 1: A 19-year-old collegiate football player sustains an injury to his left knee during a game. He was running with the ball when he dodged a defensive player and fell, twisting his left knee. He felt a “pop” as he fell. When he attempts to bear weight on his left knee, it feels unstable, and "gives way." He needs assistance to walk off the field. The pain is localized diffusely over the knee and is non-radiating. His past medical history is notable for asthma. He uses an albuterol inhaler as needed. He does not smoke or drink alcohol. On exam, he has a notable suprapatellar effusion. Range of motion is limited in the extremes of flexion. When the proximal tibia is pulled anteriorly while the knee is flexed and the patient is supine, there is 1.5 centimeter of anterior translation. The contralateral knee translates 0.5 centimeters with a similar force. The injured structure in this patient originates on which of the following bony landmarks?
- A. Posteromedial aspect of the lateral femoral condyle (Correct Answer)
- B. Lateral aspect of the lateral femoral condyle
- C. Lateral aspect of the medial femoral condyle
- D. Tibial tubercle
- E. Medial aspect of the medial femoral condyle
Lower limb surface landmarks Explanation: ***Posteromedial aspect of the lateral femoral condyle***
- The patient's presentation of a **\"pop\"**, knee instability, and a **positive anterior drawer test** (excessive anterior translation of the tibia) strongly indicates an **anterior cruciate ligament (ACL) tear**.
- The **ACL originates** from the **posteromedial aspect of the lateral femoral condyle** and inserts onto the anterior intercondylar area of the tibia.
*Lateral aspect of the lateral femoral condyle*
- This area is typically associated with the origin of the **lateral collateral ligament (LCL)**, which would present with instability to **varus stress**, not anterior translation.
- Injuries to the LCL do not typically cause the described \"giving way\" sensation in the same manner as an ACL tear.
*Lateral aspect of the medial femoral condyle*
- The medial femoral condyle is primarily associated with the origin of the **medial collateral ligament (MCL)**.
- An MCL injury would typically present with **valgus instability** and pain on the medial side of the knee.
*Tibial tubercle*
- The tibial tubercle is the insertion point for the **patellar tendon**, which is the distal attachment of the quadriceps femoris muscle.
- Injuries here are more commonly associated with conditions like **Osgood-Schlatter disease** in adolescents or patellar tendon ruptures, not typically ACL-like instability.
*Medial aspect of the medial femoral condyle*
- This region is the primary origin for the **medial collateral ligament (MCL)**.
- MCL tears are often caused by **valgus stress** and would result in increased laxity to valgus forces, not anterior tibial translation.
Lower limb surface landmarks US Medical PG Question 2: A 65-year-old man comes to a follow-up appointment with his surgeon 2 months after undergoing hip replacement surgery. His major concern at this visit is that he is still limping since the surgery even after the post-operative pain has subsided. Specifically, when he stands on his right leg, he feels that he has to lean further to the right in order to maintain balance. When standing on his left leg, he feels that he is able to step normally. Damage to which of the following nerves would most likely present with this patient's symptoms?
- A. Common peroneal nerve
- B. Tibial nerve
- C. Femoral nerve
- D. Inferior gluteal nerve
- E. Superior gluteal nerve (Correct Answer)
Lower limb surface landmarks Explanation: ***Superior gluteal nerve***
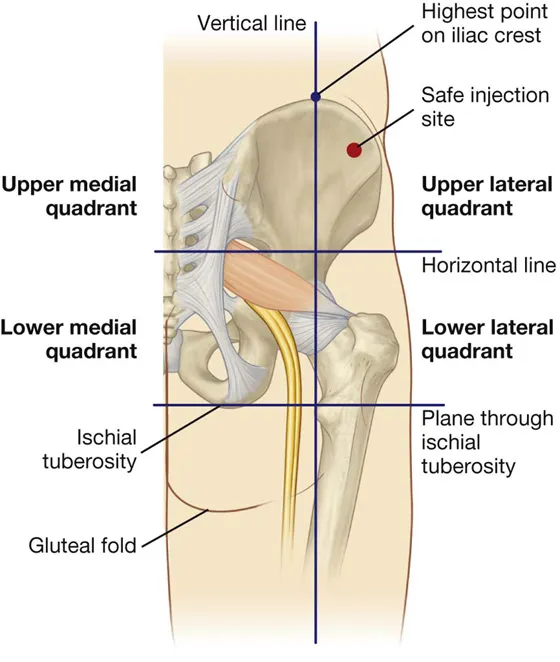
- The superior gluteal nerve innervates the **gluteus medius** and minimus muscles, which are crucial for **hip abduction** and stabilizing the pelvis during gait.
- Damage to this nerve or its muscles on one side (e.g., right side) would lead to a **Trendelenburg gait**, where the pelvis drops on the unaffected side when standing on the affected leg, and the patient compensates by leaning towards the affected side.
*Common peroneal nerve*
- The common peroneal nerve primarily innervates muscles responsible for **dorsiflexion** and **eversion of the foot**.
- Damage to this nerve commonly results in **foot drop** and an inability to evert the foot, which is not the primary symptom described.
*Tibial nerve*
- The tibial nerve innervates muscles responsible for **plantarflexion** and **inversion of the foot**, as well as the intrinsic muscles of the sole.
- Injury typically presents with difficulty walking on tiptoes, toe curling, and sensory loss in the sole of the foot, not pelvic instability.
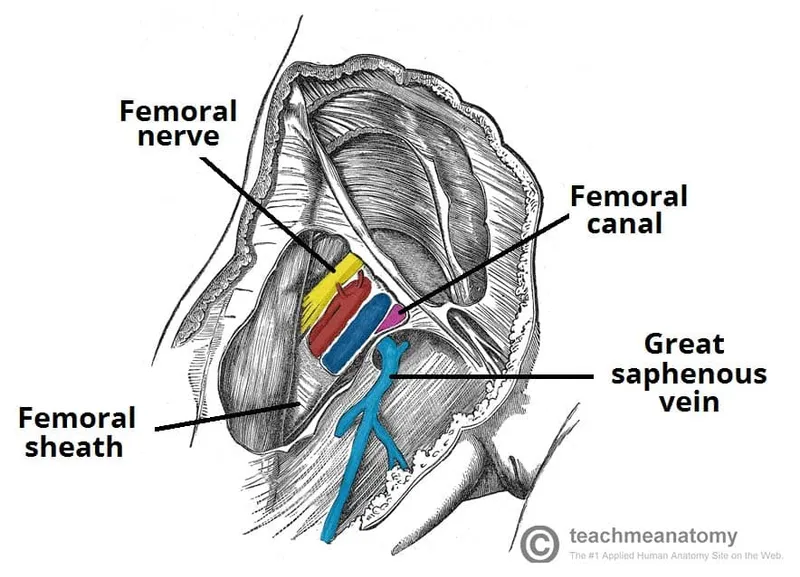
*Femoral nerve*
- The femoral nerve innervates the **quadriceps femoris** and sartorius muscles,
- Damage leads to weakness in **knee extension** and loss of sensation over the anterior thigh and medial leg.
*Inferior gluteal nerve*
- The inferior gluteal nerve innervates the **gluteus maximus** muscle, which is essential for **hip extension** and external rotation.
- Damage would primarily affect activities like climbing stairs or standing up from a seated position, rather than the specific lateral pelvic instability described.
Lower limb surface landmarks US Medical PG Question 3: A 31-year-old woman presents with difficulty walking and climbing stairs for the last 3 weeks. She has no history of trauma. The physical examination reveals a waddling gait with the trunk swaying from side-to-side towards the weight-bearing limb. When she stands on her right leg, the pelvis on the left side falls. When she stands on her left leg, the pelvis remains level. Which of the following nerves is most likely injured in this patient?
- A. Right inferior gluteal nerve
- B. Right obturator nerve
- C. Right superior gluteal nerve (Correct Answer)
- D. Right femoral nerve
- E. Left femoral nerve
Lower limb surface landmarks Explanation: ***Right superior gluteal nerve***
- The presentation of a **waddling gait** and the **Trendelenburg sign** (pelvis dropping on the unsupported side) is characteristic of **gluteus medius** and **minimus** weakness.
- These muscles are innervated by the **superior gluteal nerve**. In this case, when the patient stands on her right leg, the left pelvis falls, indicating weakness of the right gluteus medius/minimus.
*Right inferior gluteal nerve*
- The **inferior gluteal nerve** innervates the **gluteus maximus**, which is primarily responsible for hip extension.
- Damage to this nerve would primarily lead to difficulty with **climbing stairs** and rising from a seated position, but not typically the specific pelvic drop described.
*Right obturator nerve*
- The **obturator nerve** innervates the **adductor muscles** of the thigh.
- Damage would result in weakness of hip adduction and **medial thigh sensory deficits**, which are not the primary symptoms here.
*Right femoral nerve*
- The **femoral nerve** innervates the **quadriceps femoris** and the **sartorius**, responsible for knee extension and hip flexion.
- Injury would cause difficulty with **knee extension** and **hip flexion**, potentially leading to knee buckling or instability, which is not consistent with the Trendelenburg sign observed.
*Left femoral nerve*
- Injury to the left femoral nerve would affect the **left quadriceps** and **sartorius** muscles.
- This would cause weakness in extending the left knee and flexing the left hip, which is not consistent with the observed **right-sided gluteal weakness** indicated by the Trendelenburg sign on the right.
Lower limb surface landmarks US Medical PG Question 4: A 56-year-old man presents to the emergency room after being in a motor vehicle accident. He was driving on an icy road when his car swerved off the road and ran head on into a tree. He complains of severe pain in his right lower extremity. He denies loss of consciousness during the accident. His past medical history is notable for poorly controlled hypertension, hyperlipidemia, and major depressive disorder. He takes enalapril, atorvastatin, and sertraline. His temperature is 99.1°F (37.3°C), blood pressure is 155/85 mmHg, pulse is 110/min, and respirations are 20/min. On exam, he is alert and fully oriented. He is unable to move his right leg due to pain. Sensation is intact to light touch in the sural, saphenous, tibial, deep peroneal, and superficial peroneal distributions. His leg appears adducted, flexed, and internally rotated. An anteroposterior radiograph of his pelvis would most likely demonstrate which of the following findings?
- A. Fracture line extending between the greater and lesser trochanters
- B. Femoral head larger than contralateral side and inferior to acetabulum
- C. Fracture line extending through the femoral neck
- D. Fracture line extending through the subtrochanteric region of the femur
- E. Femoral head smaller than contralateral side and posterior to acetabulum (Correct Answer)
Lower limb surface landmarks Explanation: ***Femoral head smaller than contralateral side and posterior to acetabulum***
- This presentation is consistent with a **posterior hip dislocation**, which typically occurs with an **axial load** on a flexed hip, common in head-on collisions.
- On radiographs, the femoral head appears **smaller** due to magnification differences and is displaced **posteriorly** relative to the acetabulum. The affected leg is classically **shortened, adducted, and internally rotated**.
*Fracture line extending between the greater and lesser trochanters*
- This describes an **intertrochanteric hip fracture**, which typically presents with the leg **externally rotated** and **abducted**, not internally rotated and adducted.
- While caused by trauma, the clinical presentation does not align with the patient's physical exam findings.
*Femoral head larger than contralateral side and inferior to acetabulum*
- This describes an **anterior hip dislocation**, which is far less common and would present with the leg typically held in **abduction** and **external rotation**. The femoral head would also appear **larger** due to magnification from being anteriorly displaced.
- The patient's presentation of adduction and internal rotation is inconsistent with an anterior dislocation.
*Fracture line extending through the femoral neck*
- A **femoral neck fracture** usually presents with the leg in **external rotation** and **shortening**, and often involves older patients with osteoporosis after falls.
- While a severe impact could cause this, the characteristic adduction and internal rotation point more strongly to a dislocation.
*Fracture line extending through the subtrochanteric region of the femur*
- A **subtrochanteric fracture** involves the shaft of the femur just below the trochanters and commonly presents with significant pain and inability to bear weight.
- This type of fracture does not typically result in the specific adducted and internally rotated leg position seen with hip dislocations.
Lower limb surface landmarks US Medical PG Question 5: An 80-year-old woman is brought to the emergency department for left hip pain 30 minutes after she fell while walking around in her room. Examination shows left groin tenderness. The range of motion of the left hip is limited because of pain. An x-ray of the hip shows a linear fracture of the left femoral neck with slight posterior displacement of the femur. Which of the following arteries was most likely damaged in the patient's fall?
- A. Superior gluteal artery
- B. Deep circumflex iliac
- C. Deep femoral artery
- D. Obturator
- E. Medial circumflex femoral (Correct Answer)
Lower limb surface landmarks Explanation: ***Medial circumflex femoral***
- This artery is the **primary blood supply** to the femoral head and neck, making it highly vulnerable to injury in cases of femoral neck fractures.
- Damage to the medial circumflex femoral artery significantly increases the risk of **avascular necrosis** of the femoral head.
*Superior gluteal artery*
- The superior gluteal artery primarily supplies the **gluteus medius** and **minimus muscles**.
- It is **not directly involved** in the primary blood supply to the femoral head and neck.
*Deep circumflex iliac*
- This artery mainly supplies the **iliac fossa** and the **abdominal wall muscles**.
- It does not contribute significantly to the blood supply of the femoral neck.
*Deep femoral artery*
- The deep femoral artery, also known as the **profunda femoris artery**, is the main supply to the **thigh muscles**.
- While it gives rise to the circumflex arteries, it is not the artery directly compromised in a femoral neck fracture.
*Obturator*
- The obturator artery primarily supplies the **adductor muscles** of the thigh and contributes a small branch to the femoral head via the **ligamentum teres**.
- This contribution is **insufficient** to maintain viability of the femoral head, especially in trauma to the femoral neck.
Lower limb surface landmarks US Medical PG Question 6: Three hours after undergoing left hip arthroplasty for chronic hip pain, a 62-year-old man complains of a prickling sensation in his left anteromedial thigh and lower leg. He has never had these symptoms before. He has hyperlipidemia and coronary artery disease. He has had recent right-sided gluteal and thigh pain with ambulation. Vital signs are within normal limits. Sensation to pinprick and light touch are decreased on the anteromedial left thigh as well as medial lower leg. Neurologic exam shows left leg strength 3/5 on hip flexion and 2/5 on knee extension. Patellar reflex is decreased on the left. The remainder of neurologic exam is normal. Dorsalis pedis, popliteal, and femoral pulses are 2+ bilaterally. The surgical incision is without erythema or drainage. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Surgical site infection
- B. Obturator nerve injury
- C. Sural nerve injury
- D. Femoral nerve injury (Correct Answer)
- E. Femoral artery occlusion
Lower limb surface landmarks Explanation: ***Femoral nerve injury***
- The patient's symptoms of **prickling sensation (paresthesia)** in the anterior-medial thigh and medial lower leg, **decreased sensation to pinprick and light touch** in these areas, and **weakness in hip flexion (iliopsoas)** and **knee extension (quadriceps)**, along with a **decreased patellar reflex**, are all classic signs of **femoral nerve dysfunction**.
- The femoral nerve can be susceptible to injury during **hip arthroplasty** due to retraction, direct trauma, or hematoma formation, especially if the patient is slim or has anatomical variations.
*Surgical site infection*
- This typically presents with signs of **inflammation** such as erythema, warmth, severe pain, and sometimes drainage from the incision site, which are absent here.
- Neurological deficits like specific motor weakness and sensory loss in a nerve distribution are *not* primary features of a surgical site infection.
*Obturator nerve injury*
- An obturator nerve injury would primarily affect **adduction of the thigh** and might cause sensory changes in the medial thigh, but would *not* cause weakness in hip flexion or knee extension, nor would it affect the patellar reflex.
- The sensory distribution described (anteromedial thigh and medial lower leg) is more consistent with femoral nerve involvement than obturator nerve.
*Sural nerve injury*
- **Sural nerve injury** primarily causes sensory deficits along the **posterolateral aspect of the lower leg and ankle**, and the lateral aspect of the foot.
- It would *not* cause motor weakness in hip flexion or knee extension, nor would it affect the patellar reflex.
*Femoral artery occlusion*
- **Femoral artery occlusion** would cause symptoms of **acute limb ischemia**, including severe pain, pallor, pulselessness, poikilothermia (coldness), paresthesias, and paralysis (the "6 Ps").
- While paresthesias are present, the patient has **intact distal pulses (2+ bilaterally)** and no signs of pallor or coldness, ruling out significant arterial occlusion.
Lower limb surface landmarks US Medical PG Question 7: A 24-year-old professional soccer player presents to the clinic with discomfort and pain while walking. He says that he has an unstable knee joint that started after an injury during a match last week. He adds that he heard a popping sound at the time of the injury. Physical examination of the knee reveals swelling of the knee joint with a positive anterior drawer test. Which of the following structures is most likely damaged in this patient?
- A. Lateral collateral ligament
- B. Ligamentum patellae
- C. Anterior cruciate ligament (Correct Answer)
- D. Medial collateral ligament
- E. Posterior cruciate ligament
Lower limb surface landmarks Explanation: ***Anterior cruciate ligament***
- The **"popping sound"** at the time of injury, associated with knee **instability** and a **positive anterior drawer test**, are classic signs of an **ACL tear**.
- The **anterior drawer test** specifically assesses the integrity of the ACL by checking for excessive anterior translation of the tibia relative to the femur.
*Lateral collateral ligament*
- Injury to the LCL typically results from a **varus stress** to the knee and is less commonly associated with a distinct "popping" sound or significant instability.
- While it causes pain and instability, the **anterior drawer test** would likely be negative, and a **varus stress test** would be more indicative.
*Ligamentum patellae*
- Damage to the patellar ligament usually presents as pain and difficulty with knee extension, often following a forceful quadriceps contraction.
- It does not typically cause the described popping sensation or knee instability assessed by the anterior drawer test.
*Medial collateral ligament*
- MCL injuries commonly result from a **valgus stress** (force to the outside of the knee) and are diagnosed with a **valgus stress test**, not the anterior drawer test.
- While it can cause instability, the "popping" sound and specific findings of the anterior drawer test point away from an isolated MCL injury.
*Posterior cruciate ligament*
- A PCL injury is often associated with a **posteriorly directed force** to the tibia, such as a dashboard injury, and would present with a **positive posterior drawer test**.
- The clinical presentation of a **positive anterior drawer test** and significant anterior instability rules out isolated PCL damage.
Lower limb surface landmarks US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Lower limb surface landmarks Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Lower limb surface landmarks US Medical PG Question 9: An MRI of a patient with low back pain reveals compression of the L5 nerve root. Which of the following muscles would most likely show weakness during physical examination?
- A. Tibialis posterior
- B. Tibialis anterior (Correct Answer)
- C. Gastrocnemius
- D. Quadriceps femoris
Lower limb surface landmarks Explanation: ***Tibialis anterior***
- The **L5 nerve root** primarily innervates muscles responsible for **dorsiflexion** of the foot, with the **tibialis anterior** being the primary dorsiflexor.
- Weakness of the tibialis anterior would manifest as difficulty lifting the front of the foot, potentially leading to a **foot drop** gait.
*Tibialis posterior*
- The **tibialis posterior** is primarily innervated by the **tibial nerve** (S1-S2) and is responsible for **plantarflexion** and **inversion** of the foot.
- Weakness in this muscle would not be the most likely presentation of L5 nerve root compression.
*Gastrocnemius*
- The **gastrocnemius** muscle is primarily innervated by the **tibial nerve** (S1-S2) and is a powerful **plantarflexor** of the foot.
- Weakness in this muscle would indicate an S1 or S2 nerve root issue, not typically L5.
*Quadriceps femoris*
- The **quadriceps femoris** is innervated by the **femoral nerve**, predominantly originating from the **L2, L3, and L4 nerve roots**.
- Weakness would manifest as difficulty extending the knee, which is not characteristic of L5 compression.
Lower limb surface landmarks US Medical PG Question 10: A 35-year-old man comes to the physician because of a 3-month history of intermittent right lateral hip pain that radiates to the thigh. Climbing stairs and lying on his right side aggravates the pain. Examination shows tenderness to palpation over the upper lateral part of the right thigh. There is no swelling. When the patient is asked to abduct the right leg against resistance, tenderness is noted. An x-ray of the pelvis shows no abnormalities. Which of the following structures is the most likely source of this patient's pain?
- A. Femoral head
- B. Greater trochanter (Correct Answer)
- C. Iliotibial band
- D. Acetabulum
- E. Lateral femoral cutaneous nerve
Lower limb surface landmarks Explanation: ***Greater trochanter***
- The patient's symptoms of **intermittent right lateral hip pain** radiating to the thigh, aggravated by climbing stairs and lying on the affected side, and tenderness over the **upper lateral part of the right thigh** are classic signs of **trochanteric bursitis**.
- Pain with **resisted abduction** further points to inflammation of the **gluteus medius** or its associated bursa at the greater trochanter.
*Femoral head*
- Pain originating from the **femoral head** typically presents as deep, generalized groin or hip joint pain, often exacerbated by weight-bearing activities, and may be associated with limited range of motion in multiple planes.
- An **x-ray showing no abnormalities** makes femoral head issues like avascular necrosis or significant arthritis less likely.
*Iliotibial band*
- **Iliotibial band (ITB) syndrome** usually causes pain along the **lateral aspect of the knee**, particularly in runners or cyclists, due to friction over the lateral femoral epicondyle.
- While the ITB traverses the lateral thigh, the primary point of tenderness and mechanism of pain in this case (tenderness over the upper lateral thigh, pain with resisted abduction) is not typical for ITB syndrome affecting the knee.
*Acetabulum*
- Pain from the **acetabulum** would generally be deep within the hip joint, similar to femoral head issues, and often accompanied by a **limited range of motion** or clicking/locking sensations, and would be associated with intra-articular pathology.
- An **unremarkable X-ray** and the specific finding of **tenderness over the lateral thigh** make acetabular pathology less likely.
*Lateral femoral cutaneous nerve*
- Entrapment of the **lateral femoral cutaneous nerve** (meralgia paresthetica) typically causes **numbness, burning, or tingling** on the anterolateral thigh, not primarily sharp, intermittent pain aggravated by movement and palpation in the manner described.
- While pain can be present, the absence of **paresthesias** and the mechanical nature of the pain (aggravated by resisted abduction) make nerve entrapment less probable.
More Lower limb surface landmarks US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.