Head and neck surface landmarks US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Head and neck surface landmarks. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Head and neck surface landmarks US Medical PG Question 1: A 4-year-old girl is brought to the physician for a painless lump on her neck. She has no history of serious illness and her vital signs are within normal limits. On examination, there is a firm, 2-cm swelling at the midline just below the level of the hyoid bone. The mass moves cranially when she is asked to protrude her tongue. Which of the following is the most likely diagnosis?
- A. Cystic hygroma
- B. Thyroglossal cyst (Correct Answer)
- C. Ranula
- D. Dermoid cyst
Head and neck surface landmarks Explanation: Thyroglossal cyst
- A midline neck mass that moves cranially with tongue protrusion is the classic presentation of a thyroglossal duct cyst.
- These cysts arise from the remnant of the thyroglossal duct, the embryonic tract along which the thyroid gland descends from the foramen cecum to its final position [1].
Cystic hygroma
- This is a lymphatic malformation typically appearing as a soft, compressible, transilluminant mass, often in the posterior triangle of the neck.
- It does not move with tongue protrusion and is usually not midline.
Ranula
- A ranula is a mucocele that forms in the floor of the mouth, usually due to obstruction of a sublingual salivary gland.
- It presents as a swelling in the oral cavity, below the tongue, and not as an external neck mass.
Dermoid cyst
- A dermoid cyst in the neck is typically a painless, doughy, subcutaneous mass that is also usually midline but does not move with tongue protrusion.
- These cysts are often found above the hyoid bone, unlike the typical position of a thyroglossal cyst.
Head and neck surface landmarks US Medical PG Question 2: A 54-year-old man is brought to the emergency department 30 minutes after being hit by a car while crossing the street. He had a left-sided tonic-clonic seizure and one episode of vomiting while being transported to the hospital. On arrival, he is not oriented to person, place, or time. Physical examination shows flaccid paralysis of all extremities. A CT scan of the head is shown. This patient's symptoms are most likely the result of a hemorrhage in which of the following structures?
- A. Between the dura mater and the arachnoid mater
- B. Into the cerebral parenchyma
- C. Between the skull and the dura mater
- D. Between the arachnoid mater and the pia mater (Correct Answer)
- E. Into the ventricular system
Head and neck surface landmarks Explanation: ***Between the arachnoid mater and the pia mater (Correct)***
- The CT scan demonstrates diffuse high-density (white) material within the sulci and basal cisterns, indicative of a **subarachnoid hemorrhage**. This space is located between the arachnoid mater and the pia mater.
- The patient's presentation with altered mental status, seizures, vomiting, and flaccid paralysis following trauma is consistent with the severe neurological impact of a **traumatic subarachnoid hemorrhage**.
*Between the dura mater and the arachnoid mater (Incorrect)*
- Hemorrhage in this location is known as a **subdural hematoma**, which typically appears as a crescent-shaped collection of blood.
- While possible in trauma, the CT image shows blood primarily filling the sulci, not a subdural collection.
*Into the cerebral parenchyma (Incorrect)*
- This would be an **intraparenchymal hemorrhage**, appearing as a focal area of high density within the brain tissue itself.
- Although there might be some associated parenchymal injury in severe trauma, the predominant pattern seen on the CT is diffuse blood in the subarachnoid space.
*Between the skull and the dura mater (Incorrect)*
- This describes an **epidural hematoma**, often characterized by a lenticular (lens-shaped) collection of blood due to its confinement by dural attachments.
- The CT image does not show a lenticular collection of blood in this space.
*Into the ventricular system (Incorrect)*
- **Intraventricular hemorrhage** would show blood filling the cerebral ventricles.
- While subarachnoid hemorrhage can sometimes extend into the ventricles, the primary finding on this CT is diffuse blood in the subarachnoid space, not isolated ventricular blood.
Head and neck surface landmarks US Medical PG Question 3: A 26-year-old woman presents to your clinic with complaints of increasing muscle fatigue that worsens after periods of sustained activity. She also reports both ptosis and diplopia that make reading in the late afternoon and evenings difficult. An edrophonium test is performed and is positive, demonstrating resolution of the patient's weakness. One organ in particular, when abnormal, is associated with this patient's condition. Which of the following embryologic structures gives rise to this organ?
- A. 3rd branchial arch
- B. 4th branchial pouch
- C. 1st branchial pouch
- D. 2nd branchial cleft
- E. 3rd branchial pouch (Correct Answer)
Head and neck surface landmarks Explanation: ***3rd branchial pouch***
- The clinical presentation (muscle fatigue worsening with activity, ptosis, diplopia, positive edrophonium test) indicates **myasthenia gravis**. Myasthenia gravis is commonly associated with **thymic abnormalities**, such as thymoma or thymic hyperplasia.
- The **thymus** develops from the **third pharyngeal (branchial) pouch**.
*3rd branchial arch*
- The 3rd branchial arch gives rise to structures such as the common **carotid artery**, proximal internal carotid artery, **stylopharyngeus muscle**, and **glossopharyngeal nerve (CN IX)**.
- It does not contribute to the development of the thymus or structures related to myasthenia gravis.
*4th branchial pouch*
- The 4th branchial pouch gives rise to the **superior parathyroid glands** and the **parafollicular C cells** of the thyroid gland.
- It is not involved in the embryological development of the thymus.
*1st branchial pouch*
- The 1st branchial pouch gives rise to the **eustachian tube**, **middle ear cavity**, and part of the mastoid air cells.
- These structures are unrelated to the thymus or myasthenia gravis.
*2nd branchial cleft*
- The 2nd, 3rd, and 4th branchial clefts typically merge and obliterate to form the **cervical sinus**.
- Persistence of these clefts or their incomplete obliteration can lead to **branchial cleft cysts or fistulas**, which are distinct from thymic development.
Head and neck surface landmarks US Medical PG Question 4: A 65-year-old male presents to the emergency room complaining of a severe headache. He developed a sudden-onset severe throbbing headache while watching a football game on television. His past medical history is significant for migraines and hypertension; however, he states that this headache is different from his normal migraine headaches. He has a 30 pack-year smoking history. His family history is notable for stroke in his mother and father. His temperature is 98.9°F (37.2°C), blood pressure is 150/90 mmHg, pulse is 100/min, and respirations are 14/min. On examination, he is oriented to person, place, and time. Neck motion is limited due to pain. Strength is 5/5 bilaterally in both the upper and the lower extremities and sensation is grossly intact across all the dermatomal distributions. Patellar, brachioradialis, and Achilles reflexes are 2+ bilaterally. The vessel that is most commonly involved in this patient's likely condition directly branches off which of the following vessels?
- A. Middle cerebral artery
- B. Maxillary artery
- C. Anterior cerebral artery
- D. Posterior cerebral artery
- E. Internal carotid artery (Correct Answer)
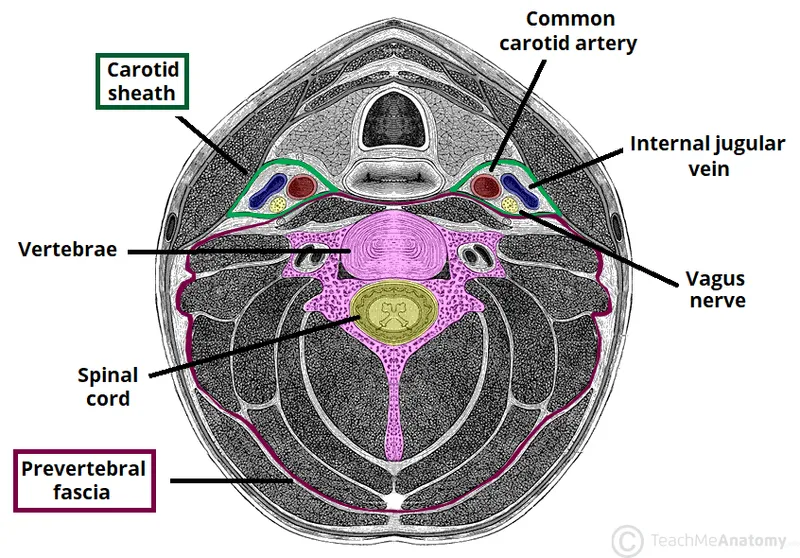
Head and neck surface landmarks Explanation: ***Internal carotid artery***
- The patient's presentation with a **sudden-onset, severe "thunderclap" headache**, cervical pain, and normal neurologic examination, particularly in the context of **hypertension and smoking history**, is highly suggestive of a **subarachnoid hemorrhage (SAH)**. SAH is most commonly caused by rupture of a **saccular (berry) aneurysm**.
- Approximately 85% of SAHs result from the rupture of an aneurysm in the **anterior circulation**. The most common site for these aneurysms is the **anterior communicating artery**, which directly branches off the **anterior cerebral artery**. However, the **anterior cerebral artery (ACA)**, the **middle cerebral artery (MCA)**, and the **posterior communicating artery (PCoA)** (which is commonly involved in berry aneurysms) all originate directly or indirectly, through the ACA, from the **internal carotid artery (ICA)**. Therefore, the ICA is the most encompassing and correct option from which the most common aneurysm sites ultimately branch.
*Middle cerebral artery*
- While the **middle cerebral artery (MCA)** is a common location for aneurysms, particularly at its bifurcation, it is generally less common than the anterior communicating artery or the posterior communicating artery.
- Aneurysms of the MCA are also branches of the internal carotid artery.
*Maxillary artery*
- The **maxillary artery** is primarily involved in supplying blood to structures in the deep face, maxilla, and mandible.
- It is not a significant location for intracranial berry aneurysms that lead to subarachnoid hemorrhage.
*Anterior cerebral artery*
- While the **anterior cerebral artery (ACA)** itself can be a site for aneurysms, particularly the **anterior communicating artery** (AComA) which connects the two ACAs, it is a branch off the internal carotid artery.
- The AComA is the single most common site for berry aneurysms; however, the question asks for the vessel from which the commonly involved vessel *directly branches off*. The ACA itself directly branches off the ICA.
*Posterior cerebral artery*
- The **posterior cerebral artery (PCA)** is part of the posterior circulation, originating from the basilar artery.
- Aneurysms in the posterior circulation (vertebrobasilar system) are less common causes of SAH than those in the anterior circulation.
Head and neck surface landmarks US Medical PG Question 5: A 47-year-old man presents to you with gradual loss of voice and difficulty swallowing for the past couple of months. The difficulty of swallowing is for both solid and liquid foods. His past medical history is insignificant except for occasional mild headaches. Physical exam also reveals loss of taste sensation on the posterior third of his tongue and palate, weakness in shrugging his shoulders, an absent gag reflex, and deviation of the uvula away from the midline. MRI scanning was suggested which revealed a meningioma that was compressing some cranial nerves leaving the skull. Which of the following openings in the skull transmit the affected cranial nerves?
- A. Jugular foramen (Correct Answer)
- B. Foramen rotundum
- C. Foramen spinosum
- D. Foramen ovale
- E. Foramen lacerum
Head and neck surface landmarks Explanation: ***Jugular foramen***
- The symptoms described—loss of voice, difficulty swallowing, loss of taste on the posterior third of the tongue, absent gag reflex, and uvula deviation—point to impairment of **cranial nerves IX (glossopharyngeal), X (vagus), XI (accessory)**, which all exit the skull via the **jugular foramen**.
- The **vagus nerve** (CN X) is responsible for voice and swallowing (via innervation of the pharynx and larynx), the **glossopharyngeal nerve** (CN IX) for taste from the posterior third of the tongue and the gag reflex, and the **accessory nerve** (CN XI) for shoulder shrugging (trapezius and sternocleidomastoid muscles).
- Note: Loss of taste on the palate may involve CN VII (facial nerve) fibers, but the dominant clinical picture with absent gag reflex, uvula deviation, dysphagia, and dysphonia clearly indicates jugular foramen pathology.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, a branch of the trigeminal nerve.
- Damage to V2 would primarily cause sensory deficits in the midface and upper teeth, which are not described in this patient.
*Foramen spinosum*
- The **foramen spinosum** transmits the **middle meningeal artery** and the **meningeal branch of the mandibular nerve (V3)**.
- Injury here would not explain the constellation of symptoms related to voice, swallowing, taste, or shoulder movement.
*Foramen ovale*
- The **foramen ovale** transmits the **mandibular nerve (V3)**, the **accessory meningeal artery**, and occasionally the superficial petrosal nerve.
- Damage to V3 would result in sensory loss to the lower face and motor deficits in the muscles of mastication, which are not reported.
*Foramen lacerum*
- The **foramen lacerum** is filled with cartilage in vivo and does not typically transmit major neurovascular structures directly through its aperture.
- The **internal carotid artery** passes superior to it, and some small nerves may traverse its vicinity, but not the specific cranial nerves indicated by the patient's symptoms.
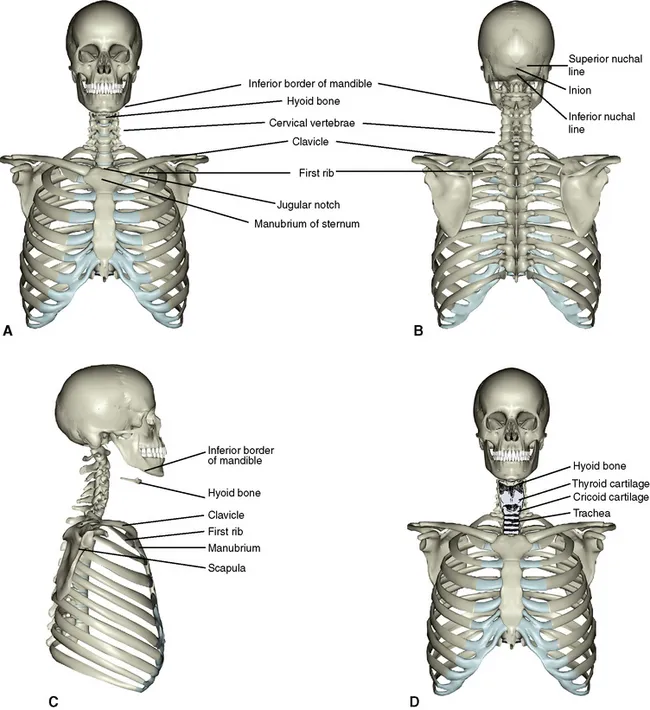
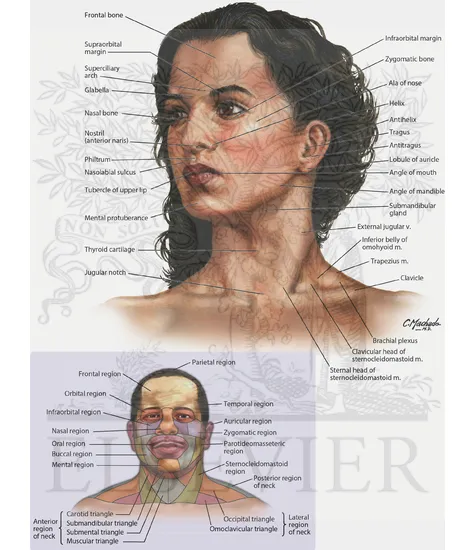
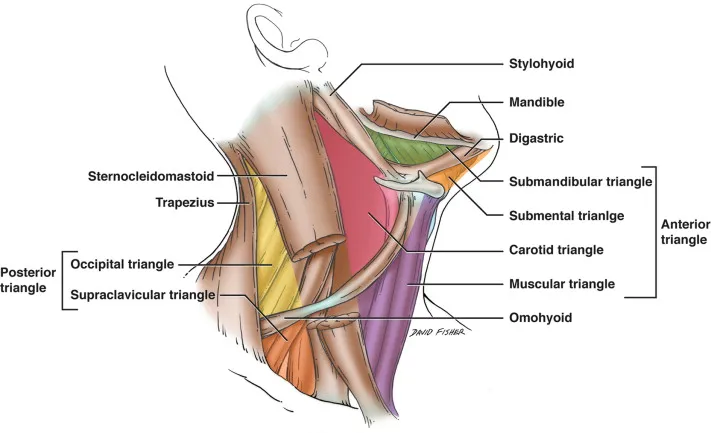
Head and neck surface landmarks US Medical PG Question 6: During a surgical procedure involving the posterior triangle of the neck, which of the following muscles forms its anterior boundary?
- A. Scalene anterior
- B. Trapezius
- C. Sternocleidomastoid (Correct Answer)
- D. Omohyoid
Head and neck surface landmarks Explanation: ***Sternocleidomastoid***
- The **sternocleidomastoid muscle** forms the **anterior boundary** of the **posterior triangle of the neck**.
- Its broad origin on the sternum and clavicle and insertion on the mastoid process help define this triangular region.
*Scalene anterior*
- The **scalene anterior muscle** is located deeper in the neck and is not a direct boundary of the posterior triangle.
- This muscle is part of the **floor** of the posterior triangle, along with other prevertebral muscles, but does not form its anterior border.
*Trapezius*
- The **trapezius muscle** forms the **posterior boundary** of the posterior triangle of the neck, running from the nuchal line and thoracic vertebrae to the clavicle and scapula.
- It would be incorrect to identify it as the anterior boundary.
*Omohyoid*
- The **inferior belly of the omohyoid muscle** crosses the posterior triangle, subdividing it into occipital and supraclavicular triangles.
- It does not form one of the main borders of the entire posterior triangle.
Head and neck surface landmarks US Medical PG Question 7: A 27-year-old man presents to a physician for evaluation of 3 months of increased vertigo. He says that occasionally he will experience several seconds of intense vertigo that makes him lose his balance. He came in for evaluation because this symptom is affecting his ability to drive to work. He has also been occasionally experiencing tinnitus. Physical exam reveals rotatory nystagmus that is delayed in onset and stops with visual fixation. The nerve that is most likely causing these symptoms exits the skull at which of the following locations?
- A. Internal auditory meatus (Correct Answer)
- B. Cribriform plate
- C. Foramen ovale
- D. Jugular foramen
- E. Foramen rotundum
Head and neck surface landmarks Explanation: ***Internal auditory meatus***
- The symptoms described, particularly **vertigo** and **tinnitus**, are indicative of an issue with the **vestibulocochlear nerve (CN VIII)**.
- The **vestibulocochlear nerve** exits the skull through the **internal auditory meatus**, which is also the pathway for the **facial nerve (CN VII)**.
*Cribriform plate*
- The **cribriform plate** is associated with the passage of the **olfactory nerves (CN I)**, which are responsible for the sense of smell.
- Damage to this area would typically cause **anosmia**, not vertigo or tinnitus.
*Foramen ovale*
- The **foramen ovale** is the exit point for the **mandibular nerve (V3)**, a branch of the trigeminal nerve.
- Dysfunction here would lead to problems with **mastication** or altered sensation in the lower face, not vertigo.
*Jugular foramen*
- The **jugular foramen** transmits several cranial nerves: the **glossopharyngeal (CN IX)**, **vagus (CN X)**, and **accessory (CN XI)** nerves.
- Issues in this region would manifest as difficulties with **swallowing**, **speech**, or **shoulder/neck movement**, not balance or hearing.
*Foramen rotundum*
- The **foramen rotundum** transmits the **maxillary nerve (V2)**, another branch of the trigeminal nerve.
- Damage to this nerve would primarily affect **sensation in the middle third of the face**, not balance or hearing.
Head and neck surface landmarks US Medical PG Question 8: A 40-year-old woman is brought to the emergency department by a paramedic team from the scene of a motor vehicle accident where she was the driver. The patient was restrained by a seat belt and was unconscious at the scene. On physical examination, the patient appears to have multiple injuries involving the trunk and extremities. There are no penetrating injuries to the chest. As part of her trauma workup, a CT scan of the chest is ordered. At what vertebral level of the thorax is this image from?
- A. T1
- B. T6
- C. T4
- D. T5
- E. T8 (Correct Answer)
Head and neck surface landmarks Explanation: ***T8***
- The CT image shows the **inferior vena cava (IVC)** located anterior and to the right of the aorta, and the **esophagus** located posterior to the aorta and slightly to the left. The **azygos vein** is seen to the right of the vertebral body and posterior to the esophagus.
- The **mainstem bronchi** are no longer visible, indicating a level below the carina. The presence of the IVC, aorta, esophagus, and azygos vein with the absence of mainstem bronchi is characteristic of the **T8 vertebral level**.
*T1*
- At the T1 level, the structures would primarily be the **trachea** anterior to the esophagus, with the main great vessels (e.g., brachiocephalic veins and arteries) visible, not the IVC.
- The mainstem bronchi would not yet be visualized at this higher level.
*T6*
- At the T6 level, the **trachea would have already bifurcated into the mainstem bronchi**, which would be prominent structures visible on the CT scan.
- While the aorta and esophagus would be present, the specific arrangement relative to the mainstem bronchi would differentiate it from T8.
*T4*
- The T4 level is typically associated with the **carina**, where the trachea bifurcates into the mainstem bronchi.
- The great vessels would be prominent, but the IVC in its more inferior course would not be as distinctly visualized in this configuration compared to T8.
*T5*
- At the T5 level, the **mainstem bronchi** would still be clearly visible, having just diverged from the trachea.
- While vessels like the aorta are present, the key differentiating factor from T8 is the presence of the mainstem bronchi.
Head and neck surface landmarks US Medical PG Question 9: A 35-year-old woman, gravida 2, para 1, at 40 weeks' gestation, presents to the hospital with contractions spaced 2 minutes apart. Her past medical history is significant for diabetes, which she has controlled with insulin during this pregnancy. Her pregnancy has otherwise been unremarkable. A baby boy is born via a spontaneous vaginal delivery. Physical examination shows he weighs 4.5 kg (9 lb), the pulse is 140/min, the respirations are 40/min, and he has good oxygen saturation on room air. His left arm is pronated and medially rotated. He is unable to move it away from his body. The infant’s right arm functions normally and he is able to move his wrists and all 10 digits. Which of the following nerve roots were most likely damaged during delivery?
- A. C4 and C5
- B. C7 and C8
- C. C5 and C6 (Correct Answer)
- D. C8 and T1
- E. C6 and C7
Head and neck surface landmarks Explanation: ***C5 and C6***
- The presentation of the infant's left arm being **pronated**, **medially rotated**, and unable to be moved away from the body is characteristic of **Erb-Duchenne palsy** (also called "waiter's tip" deformity).
- This condition results from damage to the **upper trunk of the brachial plexus**, specifically involving the **C5 and C6 nerve roots**.
- These roots innervate muscles responsible for **shoulder abduction** (deltoid, supraspinatus), **external rotation** (infraspinatus), and **elbow flexion/supination** (biceps brachii).
- The preserved wrist and digit function confirms the injury is limited to the upper trunk, sparing C7-T1.
*C4 and C5*
- While C5 is involved in Erb's palsy, the **C4 root** primarily contributes to the **phrenic nerve** (diaphragm innervation) and provides sensation to the neck and shoulder region.
- C4 does not significantly contribute to the brachial plexus motor function, so damage to C4 would not explain the shoulder and elbow deficits observed.
*C7 and C8*
- Damage to **C7 and C8** would primarily affect **wrist extension** (C7) and **finger flexion** (C8), not the shoulder abduction and elbow flexion deficits seen here.
- This pattern would be inconsistent with Erb's palsy and more suggestive of middle-to-lower trunk injury.
*C8 and T1*
- Injury to **C8 and T1** nerve roots causes **Klumpke's palsy**, affecting the **intrinsic hand muscles** and wrist flexors, leading to a "claw hand" deformity.
- The infant's preserved ability to move all wrists and digits rules out C8-T1 injury, as this would severely impair hand function and potentially cause **Horner's syndrome** (if T1 is involved).
*C6 and C7*
- While **C6** is involved in Erb's palsy, adding **C7** damage would extend the injury to affect **wrist extensors** (extensor carpi radialis) and **triceps** (elbow extension).
- The clinical presentation described is most consistent with isolated upper trunk (C5-C6) injury, not extended involvement of C7.
Head and neck surface landmarks US Medical PG Question 10: A 3629-g (8-lb) newborn is examined shortly after spontaneous vaginal delivery. She was delivered at 40 weeks' gestation and pregnancy was uncomplicated. Her mother is concerned because she is not moving her left arm as much as her right arm. Physical examination shows her left arm to be adducted and internally rotated, with the forearm extended and pronated, and the wrist flexed. The Moro reflex is present on the right side but absent on the left side. Which of the following brachial plexus structures is most likely injured in this infant?
- A. Upper trunk (Correct Answer)
- B. Axillary nerve
- C. Lower trunk
- D. Long thoracic nerve
- E. Posterior cord
Head and neck surface landmarks Explanation: ***Upper trunk***
- The symptoms described, including the arm being **adducted, internally rotated**, with the forearm extended and pronated, and a **flexed wrist**, are characteristic of **Erb-Duchenne palsy**, an injury to the **upper trunk** of the brachial plexus (C5-C6 nerve roots).
- The absence of the **Moro reflex** on the affected side further indicates an injury to the **upper brachial plexus**, as these roots contribute to the reflex arc.
*Axillary nerve*
- An injury to the **axillary nerve** would primarily affect the **deltoid** and **teres minor muscles**, leading to weakness in **shoulder abduction** and external rotation.
- While shoulder abduction is impaired in this case, the more widespread deficits affecting multiple arm movements point to a more proximal brachial plexus injury rather than an isolated axillary nerve lesion.
*Lower trunk*
- Injury to the **lower trunk** (C8-T1 nerve roots) typically results in **Klumpke's palsy**, characterized by weakness or paralysis of the **intrinsic hand muscles** and **flexors of the wrist and fingers**, leading to a "claw hand" deformity.
- The described presentation does not align with the classic features of Klumpke's palsy.
*Long thoracic nerve*
- An injury to the **long thoracic nerve** would cause **paralysis of the serratus anterior muscle**, leading to **scapular winging** (the medial border of the scapula protruding posteriorly, especially when pushing against a wall).
- This symptom is not described in the patient's presentation.
*Posterior cord*
- The **posterior cord** gives rise to the axillary and radial nerves. Injury to the posterior cord would affect muscles innervated by these nerves, including the **deltoid, triceps**, and **extensors of the wrist and fingers**.
- While some of these movements (e.g., forearm extension) are affected, the specific "waiter's tip" posture strongly points to an upper trunk injury, which involves a broader distribution of muscles than just those supplied by the posterior cord.
More Head and neck surface landmarks US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.