Vascular radiologic landmarks US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Vascular radiologic landmarks. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Vascular radiologic landmarks US Medical PG Question 1: A 3-year-old girl is brought to the emergency department by her parents with sudden onset shortness of breath. They tell the emergency physician that their daughter was lying on the bed watching television when she suddenly began gasping for air. They observed a bowl of peanuts lying next to her when they grabbed her up and brought her to the emergency department. Her respirations are 25/min, the pulse is 100/min and the blood pressure is 90/65 mm Hg. The physical findings as of now are apparently normal. She is started on oxygen and is sent in for a chest X-ray. Based on her history and physical exam findings, the cause of her current symptoms would be seen on the X-ray at which of the following sites?
- A. The superior segment of the right lower lobe
- B. The posterior segment of the right lower lobe (Correct Answer)
- C. The lingula of the left upper lobe
- D. The apical segment of the right upper lobe
- E. The apical segment of the left upper lobe
Vascular radiologic landmarks Explanation: ***The posterior segment of the right lower lobe***
- This is the **most common site for foreign body aspiration in a supine or lying down position** due to gravity and anatomical orientation.
- The history explicitly states the child was **"lying on the bed watching television"** when aspiration occurred, making the **posterior segment of the right lower lobe** the most gravity-dependent and therefore most likely location.
- The **right main bronchus** is wider, shorter, and more vertical than the left, making the right lung the predominant site for aspiration, and in supine position, the posterior segment is most dependent [1, 2].
*The superior segment of the right lower lobe*
- The **superior segment of the right lower lobe** is the most common site for aspiration in **upright, standing, or semi-upright positions**, not in a supine position.
- Since the child was lying down (supine), gravity would direct the aspirated peanut to the **posterior segment** rather than the superior segment.
- This would be correct if the child had aspirated while sitting upright.
*The lingula of the left upper lobe*
- The **lingula** is an uncommon site for aspiration because the **left main bronchus** has a sharper angle and smaller diameter compared to the right bronchus [2].
- The anatomical differences make aspiration into the right lung significantly more common than the left lung [2].
- The lingula is not a gravity-dependent area in the supine position.
*The apical segment of the right upper lobe*
- The **apical segment of the right upper lobe** is associated with aspiration when the patient is in **Trendelenburg position** (head lower than feet) or in extreme head-down positions.
- The described scenario of lying flat on the bed does not favor aspiration into apical segments, which are non-gravity-dependent in supine position.
- This location would be contra-gravity in the supine position.
*The apical segment of the left upper lobe*
- Aspiration into the **left upper lobe** is less frequent than the right lung due to the sharper angle of the left main bronchus [2].
- The **apical segment** would require head-down positioning (Trendelenburg) that is not described in this clinical scenario.
- This is the least likely location given both the supine position and left-sided anatomy.
Vascular radiologic landmarks US Medical PG Question 2: A 75-year-old man presents to the clinic for chronic fatigue of 3 months duration. Past medical history is significant for type 2 diabetes and hypertension, both of which are controlled with medications, as well as constipation. He denies any fever, weight loss, pain, or focal neurologic deficits. A complete blood count reveals microcytic anemia, and a stool guaiac test is positive for blood. He is subsequently evaluated with a colonoscopy. The physician notes some “small pouches” in the colon despite poor visualization due to inadequate bowel prep. What is the blood vessel that supplies the area with the above findings?
- A. Ileocolic artery
- B. Superior mesenteric artery
- C. Inferior mesenteric artery (Correct Answer)
- D. Middle colic artery
- E. Right colic artery
Vascular radiologic landmarks Explanation: ***Inferior mesenteric artery***
- The patient's **microcytic anemia** and **positive stool guaiac test** indicate chronic gastrointestinal blood loss, highly suggestive of **diverticulosis** presenting as "small pouches" in the colon.
- Diverticulosis commonly affects the **descending colon** and **sigmoid colon**, which are primarily supplied by branches of the **inferior mesenteric artery**.
*Ileocolic artery*
- The ileocolic artery is a branch of the **superior mesenteric artery** and supplies the **ileum**, **cecum**, and **ascending colon**.
- Diverticula are less commonly found in these regions compared to the left colon.
*Superior mesenteric artery*
- The superior mesenteric artery supplies the **midgut derivatives**, including the **small intestine** and the **right half of the large intestine** (up to the distal transverse colon).
- While it supplies a large portion of the GI tract, the typical location of diverticulosis (descending and sigmoid colon) is outside its primary distribution.
*Middle colic artery*
- The middle colic artery is a branch of the **superior mesenteric artery** and supplies the **transverse colon**.
- While diverticula can occur in the transverse colon, it is not the most common location, and the inferior mesenteric artery supplies the areas most frequently affected.
*Right colic artery*
- The right colic artery is a branch of the **superior mesenteric artery** and supplies the **ascending colon**.
- Diverticula are less frequently found in the ascending colon compared to the descending and sigmoid colon.
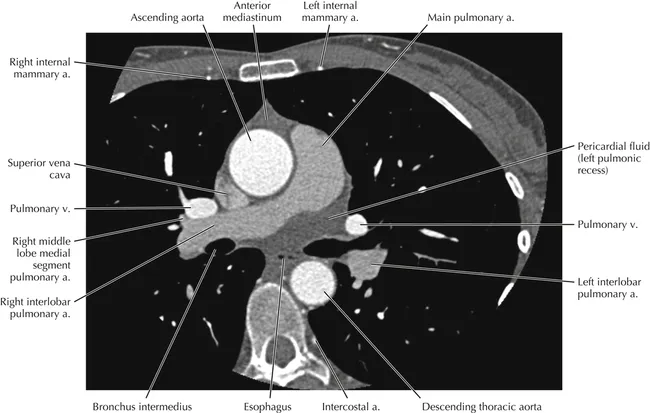
Vascular radiologic landmarks US Medical PG Question 3: A 56-year-old man is brought to the emergency department 25 minutes after the sudden onset of severe pain in the middle of his chest. He describes the pain as tearing in quality; it radiates to his jaw. He has hypertension. He has smoked one pack of cigarettes daily for the 25 years. Current medications include enalapril. His blood pressure is 154/95 mm Hg in his right arm and 181/105 mm Hg in his left arm. A CT scan of the chest is shown. The structure indicated by the arrow is a derivative of which of the following?
- A. Right horn of sinus venosus
- B. Primitive atrium
- C. Right common cardinal vein
- D. Truncus arteriosus (Correct Answer)
- E. Bulbus cordis
Vascular radiologic landmarks Explanation: ***Truncus arteriosus***
- This clinical scenario describes an **aortic dissection**, suggested by the sudden onset of **tearing chest pain radiating to the jaw**, significant **blood pressure differential** between arms, and presenting in a patient with **hypertension and smoking history**.
- The image likely shows a dilated aorta or an aortic dissection. The **truncus arteriosus** is the embryonic precursor to the **ascending aorta** and the **pulmonary trunk**, making it the correct derivative for the affected structure.
*Right horn of sinus venosus*
- The **right horn of the sinus venosus** primarily contributes to the formation of the **smooth-walled part of the right atrium** (sinus venarum).
- It does not give rise to the aorta, which is the structure involved in the described pathology.
*Primitive atrium*
- The **primitive atrium** develops into the **trabeculated parts** of both the **right and left atria** (atrial appendages).
- It is not involved in the formation of the great arteries like the aorta.
*Right common cardinal vein*
- The **right common cardinal vein** contributes to the formation of the **superior vena cava**.
- It is not a developmental source for the aorta.
*Bulbus cordis*
- The **bulbus cordis** gives rise to the **conus arteriosus** (infundibulum) of the right ventricle, the **aortic vestibule** of the left ventricle, and part of the **right ventricle**.
- While it is a component of the outflow tract, the primary structure from which the ascending aorta develops is the truncus arteriosus.
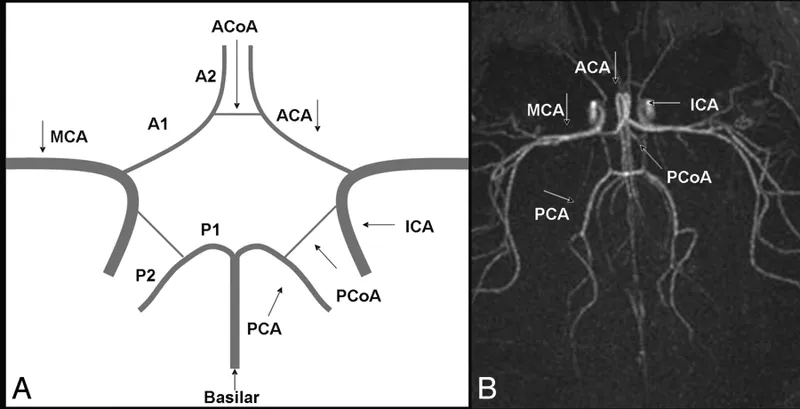
Vascular radiologic landmarks US Medical PG Question 4: A 76-year-old woman with hypertension and coronary artery disease is brought to the emergency department after the sudden onset of right-sided weakness. Her pulse is 83/min and blood pressure is 156/90 mm Hg. Neurological examination shows right-sided facial drooping and complete paralysis of the right upper and lower extremities. Tongue position is normal and she is able to swallow liquids without difficulty. Knee and ankle deep tendon reflexes are exaggerated on the right. Sensation to vibration, position, and light touch is normal bilaterally. She is oriented to person, place, and time, and is able to speak normally. Occlusion of which of the following vessels is the most likely cause of this patient's current symptoms?
- A. Ipsilateral anterior cerebral artery
- B. Contralateral middle cerebral artery
- C. Anterior spinal artery
- D. Contralateral lenticulostriate artery (Correct Answer)
- E. Ipsilateral posterior inferior cerebellar artery
Vascular radiologic landmarks Explanation: ***Contralateral lenticulostriate artery***
- The patient presents with **pure motor hemiparesis** affecting the face, arm, and leg equally on the right side, with **no sensory deficits, aphasia, or cognitive impairment**.
- This clinical pattern is classic for a **lacunar stroke** affecting the **internal capsule**, which is supplied by the **lenticulostriate arteries** (branches of the middle cerebral artery).
- The internal capsule contains tightly packed corticospinal and corticobulbar fibers; a small infarct here causes complete contralateral motor deficits without cortical signs.
- The **absence of cortical findings** (normal speech, cognition, and sensation) distinguishes this from cortical MCA stroke.
*Contralateral middle cerebral artery*
- A **cortical MCA stroke** would typically present with **cortical signs** such as aphasia (if left hemisphere), neglect (if right hemisphere), sensory loss, and visual field defects.
- MCA strokes usually show **arm and face > leg** weakness (the leg area is supplied by ACA).
- This patient's **pure motor syndrome** without cortical signs points to a subcortical lesion, not cortical MCA occlusion.
*Ipsilateral anterior cerebral artery*
- First, the lateralization is incorrect - symptoms are right-sided, indicating left hemisphere pathology, so it would be **contralateral** ACA.
- ACA occlusion causes weakness predominantly in the **contralateral leg > arm**, with relative sparing of the face.
- This patient has equal involvement of face, arm, and leg, which is inconsistent with ACA territory.
*Anterior spinal artery*
- The **anterior spinal artery** supplies the anterior two-thirds of the spinal cord, including the corticospinal tracts and anterior horn cells.
- Occlusion causes **bilateral** motor weakness below the lesion level and bilateral loss of pain/temperature sensation.
- It does not cause **unilateral facial weakness** or the distribution of deficits seen in this patient.
*Ipsilateral posterior inferior cerebellar artery*
- Again, lateralization is incorrect - symptoms would be from **contralateral** PICA for motor findings, but PICA supplies the lateral medulla and inferior cerebellum.
- PICA occlusion causes **lateral medullary syndrome (Wallenberg syndrome)**: ataxia, vertigo, dysphagia, dysarthria, Horner syndrome, and contralateral pain/temperature loss.
- The patient's **pure motor hemiparesis** without cerebellar or brainstem signs is incompatible with PICA occlusion.
Vascular radiologic landmarks US Medical PG Question 5: A 28-year-old man is brought to the emergency department by ambulance after developing an altered mental state following blunt trauma to the head. The patient was competing at a local mixed martial arts competition when he was struck in the head and lost consciousness. A few minutes later, upon regaining consciousness, he had a progressive decline in mental status. Past medical history is noncontributory. Upon arrival at the hospital, the temperature is 37.0°C (98.6°F), the blood pressure is 145/89 mm Hg, the pulse is 66/min, the respiratory rate is 14/min, and the oxygen saturation is 99% on room air. He is alert now. A noncontrast CT scan is performed, and the result is provided in the image. Which of the following structures is most likely affected in this patient?
- A. Subarachnoid space
- B. Suprasellar cistern
- C. Middle Meningeal artery (Correct Answer)
- D. Ventricular system
- E. Bridging veins
Vascular radiologic landmarks Explanation: ***Middle Meningeal artery***
- The CT scan shows a **lenticular** or **biconvex** shaped hemorrhage, characteristic of an **epidural hematoma**. This type of hematoma is typically caused by trauma leading to rupture of the middle meningeal artery.
- The history of blunt head trauma followed by a **lucid interval** and then progressive neurological decline strongly points to an epidural hematoma, which results from arterial bleeding.
*Subarachnoid space*
- Hemorrhage in the subarachnoid space (subarachnoid hemorrhage) typically appears as **blood filling the sulci and basal cisterns** on CT, not a localized collection like seen in the image.
- While subarachnoid hemorrhage can be traumatic, the classic presentation of an epidural hematoma (lucid interval, lenticular shape) is not consistent with primary subarachnoid bleeding.
*Suprasellar cistern*
- The suprasellar cistern is located at the base of the brain, superior to the sella turcica, and typically contains cerebrospinal fluid.
- While it can be affected by subarachnoid hemorrhage, the image clearly shows a hematoma in the temporal-parietal region, not specifically within the suprasellar cistern.
*Ventricular system*
- The ventricular system contains CSF and is an internal structure of the brain. Hemorrhage within the ventricles (intraventricular hemorrhage) would appear as blood filling the ventricular spaces.
- The image shows an extra-axial hematoma, meaning outside the brain parenchyma and ventricles.
*Bridging veins*
- Rupture of bridging veins typically causes a **subdural hematoma**, which appears as a **crescent-shaped** collection of blood along the surface of the brain, conforming to the contours of the cerebral hemisphere.
- The hematoma in the image has a **lenticular (biconvex)** shape, which is characteristic of an epidural hematoma, not a subdural hematoma.
Vascular radiologic landmarks US Medical PG Question 6: A 65-year-old man presents to the emergency department with vague, constant abdominal pain, and worsening shortness of breath for the past several hours. He has baseline shortness of breath and requires 2–3 pillows to sleep at night. He often wakes up because of shortness of breath. Past medical history includes congestive heart failure, diabetes, hypertension, and hyperlipidemia. He regularly takes lisinopril, metoprolol, atorvastatin, and metformin. His temperature is 37.0°C (98.6°F), respiratory rate 25/min, pulse 67/min, and blood pressure 98/82 mm Hg. On physical examination, he has bilateral crackles over both lung bases and a diffusely tender abdomen. His subjective complaint of abdominal pain is more severe than the observed tenderness on examination. Which of the following vessels is involved in the disease affecting this patient?
- A. Left anterior descending
- B. Celiac artery and superior mesenteric artery (Correct Answer)
- C. Left colic artery
- D. Right coronary artery
- E. Meandering mesenteric artery
Vascular radiologic landmarks Explanation: **Celiac artery and superior mesenteric artery**
- The patient's presentation with **vague, constant abdominal pain** out of proportion to physical exam findings (**abdominal pain more severe than tenderness**) in the setting of **congestive heart failure** and **hypotension** is highly suggestive of **non-occlusive mesenteric ischemia (NOMI)**.
- NOMI results from **splanchnic vasoconstriction** leading to hypoperfusion of the bowel, primarily affecting the territories supplied by the **celiac artery** and **superior mesenteric artery**, which supply the foregut and midgut, respectively.
*Left anterior descending*
- The left anterior descending (LAD) artery primarily supplies the **left ventricle** and interventricular septum.
- Occlusion of the LAD typically causes a **myocardial infarction** with chest pain, EKG changes, and elevated cardiac enzymes, which is not the primary presentation here, although a degree of cardiac compromise exacerbates the NOMI.
*Left colic artery*
- The left colic artery is a branch of the **inferior mesenteric artery** and supplies portions of the **descending colon**.
- While bowel ischemia can affect this region, NOMI, a more widespread condition, is unlikely to be isolated to the left colic artery distribution, and the patient's symptoms are more consistent with multi-vessel involvement.
*Right coronary artery*
- The right coronary artery (RCA) supplies the **right ventricle**, inferior wall of the left ventricle, and often the **SA and AV nodes**.
- RCA occlusion typically leads to **inferior wall myocardial infarction** and can cause bradyarrhythmias, but it would not directly cause the described abdominal pain and out-of-proportion findings.
*Meandering mesenteric artery*
- The meandering mesenteric artery is an anatomical variant, an **anastomotic connection** between the superior and inferior mesenteric arteries.
- While it can be a source of collateral flow, it is not a primary vessel targeted in the pathogenesis of NOMI, which affects the main mesenteric arteries due to global hypoperfusion.
Vascular radiologic landmarks US Medical PG Question 7: A 78-year-old left-handed woman with hypertension and hyperlipidemia is brought to the emergency room because of sudden-onset right leg weakness and urinary incontinence. Neurologic examination shows decreased sensation over the right thigh. Muscle strength is 2/5 in the right lower extremity and 4/5 in the right upper extremity. Strength and sensation in the face are normal but she has difficulty initiating sentences and she is unable to write her name. The most likely cause of this patient’s condition is an occlusion of which of the following vessels?
- A. Right vertebrobasilar artery
- B. Right middle cerebral artery
- C. Left posterior cerebral artery
- D. Left anterior cerebral artery (Correct Answer)
- E. Right anterior cerebral artery
Vascular radiologic landmarks Explanation: ***Left anterior cerebral artery***
- Stroke in the **left anterior cerebral artery (ACA)** territory typically causes **contralateral leg weakness** (right leg in this case) and **urinary incontinence** due to involvement of the paracentral lobule.
- The patient's difficulty writing her name (agraphia) and initiating sentences (transcortical motor aphasia, which can manifest as difficulty initiating speech) is consistent with damage to the supplemental motor area in the dominant (left) hemisphere, provided by the ACA.
*Right vertebrobasilar artery*
- Occlusion of the vertebrobasilar artery typically presents with a wide range of symptoms including **vertigo**, **ataxia**, **dysarthria**, and bilateral or alternating sensory/motor deficits.
- It would not selectively cause isolated right leg weakness, urinary incontinence, and dominant hemisphere language difficulties without other brainstem or cerebellar signs.
*Right middle cerebral artery*
- A stroke in the **right middle cerebral artery (MCA)** would cause **left-sided deficit**, not right-sided.
- Although it can cause motor and sensory deficits, it typically affects the arm and face more than the leg, and would not cause the specific language deficits of the dominant hemisphere seen here.
*Left posterior cerebral artery*
- Occlusion of the **left posterior cerebral artery (PCA)** typically leads to issues like **contralateral homonymous hemianopia**, visual field defects, and potentially memory impairment or alexia without agraphia if the splenium of the corpus callosum is involved.
- It directly affects posterior brain regions, so it would not cause the anterior cerebral artery specific symptoms such as prominent contralateral leg weakness, urinary incontinence, or the described language difficulties.
*Right anterior cerebral artery*
- Occlusion of the **right anterior cerebral artery (ACA)** would cause **left leg weakness** and **left-sided sensory deficits**, not the right-sided deficits observed in this patient.
- While it could cause urinary incontinence, the combination of right-sided weakness and dominant hemisphere language deficits points against a right ACA occlusion.
Vascular radiologic landmarks US Medical PG Question 8: A 3175-g (7-lb) male newborn is delivered at 39 weeks' gestation to a 29-year-old primigravid woman following a spontaneous vaginal delivery. Apgar scores are 8 and 9 at 1 and 5 minutes, respectively. Cardiac examination in the delivery room shows a continuous machine-like murmur. An echocardiogram shows a structure with blood flow between the pulmonary artery and the aorta. This structure is most likely a derivate of which of the following?
- A. 4th aortic arch
- B. 1st aortic arch
- C. 6th aortic arch (Correct Answer)
- D. 2nd aortic arch
- E. 3rd aortic arch
Vascular radiologic landmarks Explanation: ***6th aortic arch***
- The description of a "continuous machine-like murmur" and a structure with blood flow between the pulmonary artery and the aorta is characteristic of a **patent ductus arteriosus (PDA)**.
- The **ductus arteriosus** is a remnant of the **6th aortic arch**, connecting the pulmonary artery to the aorta in fetal life.
*4th aortic arch*
- The **4th aortic arch** contributes to the formation of the **aortic arch** itself on the left side and the proximal **right subclavian artery** on the right.
- Abnormalities of the 4th arch can lead to conditions like **coarctation of the aorta** or **vascular rings**, which do not typically present as a PDA.
*1st aortic arch*
- The **1st aortic arch** largely disappears, but its remnants contribute to the formation of the **maxillary artery** and the **external carotid artery**.
- It is not involved in developmental anomalies of the major vessels between the pulmonary artery and aorta.
*2nd aortic arch*
- The **2nd aortic arch** also largely regresses, but its remnants contribute to the **stapedial artery** and part of the **hyoid artery**.
- It does not play a role in the formation of the ductus arteriosus or other major arteries of the heart.
*3rd aortic arch*
- The **3rd aortic arch** develops into the common carotid arteries and the proximal internal carotid arteries.
- Genetic disorders and malformations involving this arch typically affect the carotid system, not the connection between the pulmonary artery and aorta.
Vascular radiologic landmarks US Medical PG Question 9: A young researcher is responsible for graphing laboratory data involving pulmonary blood flow and ventilation pattern obtained from a healthy volunteer who was standing in an upright position. After plotting the following graph, the researcher realizes he forgot to label the curves and the x-axis (which represents the position in the lung). Which of the following is the appropriate label for each point on the graph?
- A. A: Ventilation B: Blood flow C: Base of the lung D: Apex of the lung (Correct Answer)
- B. A: Ventilation B: Blood flow C: Mid-portion of the lung D: Apex of the lung
- C. A: Dead Space B: Shunt C: Base of the lung D: Apex of the lung
- D. A: Blood flow B: Ventilation C: Base of the lung D: Lung hilum
- E. A: Blood flow B: Ventilation C: Apex of the lung D: Lung hilum
Vascular radiologic landmarks Explanation: ***A: Ventilation B: Blood flow C: Base of the lung D: Apex of the lung***
- In an upright individual, both **ventilation** and **blood flow** are greater at the **base of the lung** than at the apex due to gravity.
- However, the increase in **perfusion** from apex to base (curve B) is proportionally much greater than the increase in **ventilation** (curve A), leading to a higher V/Q ratio at the apex and a lower V/Q ratio at the base.
*A: Ventilation B: Blood flow C: Mid-portion of the lung D: Apex of the lung*
- This option correctly identifies curves A and B but incorrectly labels C as the **mid-portion of the lung** instead of the base.
- The x-axis represents the lung from base to apex or vice-versa, and the curve indicates the highest values at C.
*A: Dead Space B: Shunt C: Base of the lung D: Apex of the lung*
- This option incorrectly identifies curves A and B; they represent **ventilation** and **blood flow**, not dead space and shunt, which are concepts related to V/Q mismatch.
- **Dead space** refers to ventilated but unperfused areas, while a **shunt** is perfused but unventilated.
*A: Blood flow B: Ventilation C: Base of the lung D: Lung hilum*
- This option incorrectly reverses the labels for curves A and B, as **blood flow** increases more steeply than **ventilation** towards the base.
- The x-axis represents the lung position from base to apex, not the **hilum**, which is a specific anatomical region.
*A: Blood flow B: Ventilation C: Apex of the lung D: Lung hilum*
- This option incorrectly reverses the labels for curves A and B, in addition to mislabeling C as the **apex of the lung**, where values are lowest, not highest.
- The X-axis represents the lung position from base to apex, not focusing on the **hilum**.
Vascular radiologic landmarks US Medical PG Question 10: A researcher is investigating the blood supply of the adrenal gland. While performing an autopsy on a patient who died from unrelated causes, he identifies a vessel that supplies oxygenated blood to the inferior aspect of the right adrenal gland. Which of the following vessels most likely gave rise to the vessel in question?
- A. Inferior phrenic artery
- B. Abdominal aorta
- C. Renal artery (Correct Answer)
- D. Superior mesenteric artery
- E. Common iliac artery
Vascular radiologic landmarks Explanation: ***Renal artery***
- The **inferior suprarenal artery**, which supplies the inferior part of the adrenal gland, typically arises from the **renal artery**.
- The adrenal glands receive a rich blood supply from three main arterial sources: superior, middle, and inferior suprarenal arteries.
*Inferior phrenic artery*
- The **superior suprarenal arteries** typically arise from the **inferior phrenic arteries** and supply the superior aspect of the adrenal glands.
- While critical for adrenal blood supply, they do not typically contribute to the inferior aspect directly.
*Abdominal aorta*
- The **middle suprarenal artery** usually arises directly from the **abdominal aorta**.
- This vessel supplies the central part of the adrenal gland, but not primarily the inferior aspect.
*Superior mesenteric artery*
- The **superior mesenteric artery** primarily supplies structures of the midgut (e.g., small intestine, ascending colon) and does not typically give rise to vessels supplying the adrenal glands.
- It is located inferior to the origin of the renal arteries and the adrenal glands.
*Common iliac artery*
- The **common iliac arteries** supply the lower limbs and pelvic organs, originating from the abdominal aorta bifurcation.
- These arteries are located much too far inferior to supply the adrenal glands, which are retroperitoneal structures in the upper abdomen.
More Vascular radiologic landmarks US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.