Spinal radiologic landmarks US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Spinal radiologic landmarks. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Spinal radiologic landmarks US Medical PG Question 1: A 23-year-old man complains of lower back pain that began approximately 6 months ago. He is unsure why he is experiencing this pain and notices that this pain is worse in the morning after waking up and improves with physical activity. Ibuprofen provides significant relief. He denies bowel and bladder incontinence or erectile dysfunction. Physical exam is notable for decreased chest expansion, decreased spinal range of motion, 5/5 strength in both lower extremities, 2+ patellar reflexes bilaterally, and an absence of saddle anesthesia. Which of the following is the most appropriate next test for this patient?
- A. HLA-B27
- B. Slit-lamp examination
- C. MRI sacroiliac joint
- D. Radiograph sacroiliac joint (Correct Answer)
- E. ESR
Spinal radiologic landmarks Explanation: **Radiograph sacroiliac joint**
- Plain **radiographs of the sacroiliac (SI) joints** are typically the **initial imaging modality** for suspected **ankylosing spondylitis** due to affordability and diagnostic value.
- They can reveal characteristic changes such as **sacroiliitis (joint erosion, sclerosis, fusion)**, which are common in early-stage disease.
*HLA-B27*
- While a **positive HLA-B27** is associated with ankylosing spondylitis, it is **not diagnostic** on its own, as many HLA-B27 positive individuals never develop the disease.
- Its use is more in **confirming suspicion** or in cases where imaging is equivocal, but it's not the primary diagnostic test.
*Slit-lamp examination*
- A slit-lamp examination is used to detect **uveitis**, which can be an **extra-articular manifestation** of ankylosing spondylitis.
- However, it is not a primary diagnostic test for the condition itself, and its utility arises once the diagnosis is strongly considered or established.
*MRI sacroiliac joint*
- **MRI of the sacroiliac (SI) joints** is more sensitive than radiographs for detecting **early inflammatory changes** (e.g., bone marrow edema) that may not be visible on plain films.
- However, given the duration of symptoms (6 months) and the characteristic inflammatory back pain, **radiographs are typically the first-line imaging** due to cost-effectiveness, reserving MRI for cases with normal radiographs but high clinical suspicion.
*ESR*
- **Erythrocyte sedimentation rate (ESR)** is a **non-specific marker of inflammation** and can be elevated in various inflammatory conditions, including ankylosing spondylitis.
- It is not diagnostic for ankylosing spondylitis and cannot differentiate it from other inflammatory or infectious conditions.
Spinal radiologic landmarks US Medical PG Question 2: A 36-year-old male is taken to the emergency room after jumping from a building. Bilateral fractures to the femur were stabilized at the scene by emergency medical technicians. The patient is lucid upon questioning and his vitals are stable. Pain only at his hips was elicited. Cervical exam was not performed. What is the best imaging study for this patient?
- A. AP and lateral radiographs of hips
- B. Lateral radiograph (x-ray) of hips
- C. Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area
- D. Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area
- E. Computed tomography (CT) scan of cervical spine, hips, and lumbar area (Correct Answer)
Spinal radiologic landmarks Explanation: ***Computed tomography (CT) scan of cervical spine, hips, and lumbar area***
- In **high-energy trauma** (fall from height), a CT scan is the **gold standard** for evaluating the **spine and pelvis**, providing detailed cross-sectional images superior to plain radiographs.
- Since the **cervical exam was not performed**, cervical spine imaging is **mandatory** per ATLS (Advanced Trauma Life Support) protocols. High-energy falls carry significant risk of **cervical spine injury** even without obvious neurological symptoms.
- CT allows comprehensive assessment of **hip fractures, pelvic injuries, and the entire spine** (cervical, thoracic, lumbar), identifying both obvious and **subtle fractures** that may be missed on plain films.
- This approach provides the most **efficient and thorough evaluation** in the acute trauma setting, allowing for appropriate surgical planning and ruling out life-threatening spinal instability.
*AP and lateral radiographs of hips*
- Plain radiographs provide **limited detail** and may **miss subtle fractures**, particularly in complex areas like the pelvis and acetabulum.
- This option **fails to address cervical spine clearance**, which is essential in all high-energy trauma patients, especially when cervical exam has not been performed.
- Radiographs are insufficient for **comprehensive trauma evaluation** after a fall from height.
*Lateral radiograph (x-ray) of hips*
- A single lateral view is **grossly insufficient** for evaluating hip and pelvic fractures, providing only a **two-dimensional perspective** that can miss significant injuries.
- This option **completely neglects spinal evaluation**, which is dangerous in an uncleared trauma patient with a high-energy mechanism.
*Magnetic resonance imaging (MRI) of hips, knees, lumbar, and cervical area*
- While MRI excels at evaluating **soft tissues, ligaments, and bone marrow**, it is **not the initial imaging modality** for acute bony trauma due to longer scan times and lower sensitivity for acute fractures compared to CT.
- MRI is **time-consuming and impractical** in the emergency setting for initial fracture assessment, potentially delaying definitive treatment.
- CT is superior for evaluating **acute skeletal injuries** in the trauma bay.
*Anterior-posterior (AP) and lateral radiographs of hips, knees, lumbar, and cervical area*
- Multiple plain radiographs have **limited sensitivity** for complex or non-displaced fractures, particularly in the **spine and pelvis**, making them inadequate for high-energy trauma evaluation.
- Obtaining multiple radiographic views requires **numerous patient repositionings**, which risks further injury if **spinal instability** is present.
- Plain films provide significantly **less diagnostic information** than CT scanning for trauma assessment.
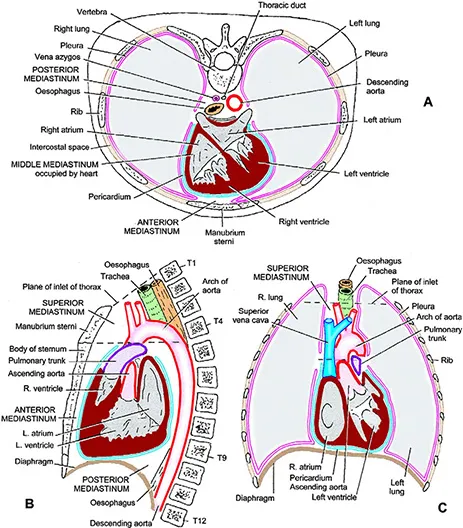
Spinal radiologic landmarks US Medical PG Question 3: During a thoracotomy procedure, a surgeon needs to access the posterior mediastinum. Which of the following structures forms the anterior boundary of the posterior mediastinum?
- A. Descending thoracic aorta
- B. Pericardial sac (Correct Answer)
- C. Azygos vein
- D. Thoracic vertebrae
- E. Sternum
Spinal radiologic landmarks Explanation: ***Pericardial sac***
- The **pericardial sac** (and the diaphragm, inferiorly) forms the anterior boundary of the **posterior mediastinum** [1].
- This anatomical relationship is crucial for surgeons during thoracotomy to distinguish between the middle and posterior mediastinal compartments [1].
*Descending thoracic aorta*
- The **descending thoracic aorta** is a large vessel located *within* the posterior mediastinum itself, typically running along its left side [2].
- Therefore, it is a content of the posterior mediastinum, not a boundary.
*Azygos vein*
- The **azygos vein** is also a major structure *within* the posterior mediastinum, running along the right side of the vertebral column.
- It is a content, not a boundary, of this compartment.
*Thoracic vertebrae*
- The **thoracic vertebrae** form the *posterior* boundary of the posterior mediastinum [1].
- This anatomical landmark gives the posterior mediastinum its name and defines its dorsal limit.
Spinal radiologic landmarks US Medical PG Question 4: A 54-year-old man presents to his primary care physician for back pain. His back pain worsens with standing for a prolonged period of time or climbing down the stairs and improves with sitting. Medical history is significant for hypertension, type II diabetes mellitus, and hypercholesterolemia. Neurologic exam demonstrates normal tone, 5/5 strength, and a normal sensory exam throughout the bilateral lower extremity. Skin exam is unremarkable and dorsalis pedis and posterior tibialis pulses are 3+. Which of the following is the best next step in management?
- A. Surgical spinal decompression
- B. MRI of the lumbosacral spine (Correct Answer)
- C. Ankle-brachial index
- D. Radiography of the lumbosacral spine
- E. Naproxen
Spinal radiologic landmarks Explanation: ***MRI of the lumbosacral spine***
- The patient's symptoms of back pain worsening with standing/climbing downstairs and improving with sitting are classic for **neurogenic claudication** due to **lumbar spinal stenosis**.
- An **MRI** is the gold standard for visualizing the spinal canal, nerve roots, and any potential compression, providing the most detailed imaging to confirm the diagnosis and guide further management.
*Surgical spinal decompression*
- This is a definitive treatment option for severe **spinal stenosis** but should only be considered after a confirmed diagnosis and failed conservative management.
- Jumping straight to surgery without proper imaging and assessment of the severity would be premature and potentially unnecessary.
*Ankle-brachial index*
- This test is primarily used to diagnose **peripheral artery disease (PAD)**, which causes **vascular claudication**.
- While it's important to differentiate vascular from neurogenic claudication, the patient's symptoms (pain relief with sitting, no mention of exertional leg pain specifically) and normal pulses make vascular claudication less likely, and an MRI is more directly indicated for the suspected neurogenic cause.
*Radiography of the lumbosacral spine*
- While X-rays can show bone anomalies and degenerative changes like **osteophytes** and decreased disc space, they do not visualize soft tissues (spinal cord, nerve roots) or the extent of spinal canal narrowing.
- Therefore, X-rays are insufficient for diagnosing **spinal stenosis** and its impact on neural structures.
*Naproxen*
- **Naproxen**, an NSAID, can provide symptomatic relief for musculoskeletal pain but does not address the underlying structural issue of **spinal stenosis**.
- It would be a component of conservative management but not the definitive "next step" for diagnosing the cause of neurogenic claudication as described.
Spinal radiologic landmarks US Medical PG Question 5: A 14-year-old boy is brought to the emergency department because of acute left-sided chest pain and dyspnea following a motor vehicle accident. His pulse is 122/min and blood pressure is 85/45 mm Hg. Physical examination shows distended neck veins and tracheal displacement to the right side. The left chest is hyperresonant to percussion and there are decreased breath sounds. This patient would most benefit from needle insertion at which of the following anatomical sites?
- A. 5th left intercostal space along the midclavicular line
- B. 8th left intercostal space along the posterior axillary line
- C. 2nd left intercostal space along the midclavicular line (Correct Answer)
- D. Subxiphoid space in the left sternocostal margin
- E. 5th left intercostal space along the midaxillary line
Spinal radiologic landmarks Explanation: ***2nd left intercostal space along the midclavicular line***
- The patient's symptoms (chest pain, dyspnea, hypotension, distended neck veins, tracheal deviation, hyperresonance, and decreased breath sounds on the left) are classic signs of a **tension pneumothorax**.
- Immediate treatment for **tension pneumothorax** involves needle decompression at the **2nd intercostal space** in the midclavicular line to relieve pressure and restore hemodynamic stability.
*5th left intercostal space along the midclavicular line*
- This location is typically used for **chest tube insertion** in a more controlled setting, not for emergent needle decompression of a tension pneumothorax.
- While it's a safe location for pleural access, it is not the **first-line site** for immediate life-saving decompression.
*8th left intercostal space along the posterior axillary line*
- This site is too low and posterior for effective needle decompression of a tension pneumothorax, which requires rapid access to the **apex of the lung**.
- It is more commonly used for **thoracentesis** to drain fluid from the pleural cavity.
*Subxiphoid space in the left sternocostal margin*
- This location is primarily used for **pericardiocentesis** to drain fluid from the pericardial sac in cases of cardiac tamponade.
- It is not appropriate for addressing a **pneumothorax**, which involves air in the pleural space.
*5th left intercostal space along the midaxillary line*
- This site is a common alternative for **chest tube insertion** but is not the preferred or most immediate site for needle decompression of a tension pneumothorax.
- While it offers pleural access, the **2nd intercostal space** anteriorly is chosen for expediency and safety in an emergency.
Spinal radiologic landmarks US Medical PG Question 6: A patient undergoes spinal surgery at the L4-L5 level. During the procedure, which of the following ligaments must be divided first to access the spinal canal?
- A. Nuchal ligament
- B. Anterior longitudinal ligament
- C. Supraspinous ligament
- D. Ligamentum flavum (Correct Answer)
Spinal radiologic landmarks Explanation: ***Ligamentum flavum***
- The **ligamentum flavum** connects the laminae of adjacent vertebrae and forms the posterior boundary of the spinal canal, making it the first ligament encountered anteriorly after removing the lamina.
- While performing a posterior approach **laminectomy**, the ligamentum flavum is typically divided or removed to gain access to the neural structures within the spinal canal.
*Nuchal ligament*
- The **nuchal ligament** is located in the cervical spine and provides attachment for muscles, extending from the external occipital protuberance to the spinous process of C7.
- It is not present at the **L4-L5 level** and therefore plays no role in lumbar spinal surgery.
*Anterior longitudinal ligament*
- The **anterior longitudinal ligament** runs along the anterior surfaces of the vertebral bodies and intervertebral discs.
- It would be encountered during an **anterior surgical approach** to the spine, not a posterior approach to access the spinal canal.
*Supraspinous ligament*
- The **supraspinous ligament** connects the tips of the spinous processes and is the most superficial ligament posteriorly.
- While it is incised during a posterior approach, it is **superficial to the lamina** and ligamentum flavum; therefore, the lamina and ligamentum flavum must be removed or divided first to access the canal.
Spinal radiologic landmarks US Medical PG Question 7: A 51-year-old woman comes to the physician because of progressively worsening lower back pain. The pain radiates down the right leg to the lateral side of the foot. She has had no trauma, urinary incontinence, or fever. An MRI of the lumbar spine shows disc degeneration and herniation at the level of L5–S1. Which of the following is the most likely finding on physical examination?
- A. Difficulty walking on heels
- B. Exaggerated patellar tendon reflex
- C. Diminished sensation of the anus and genitalia
- D. Diminished sensation of the anterior lateral thigh
- E. Weak Achilles tendon reflex (Correct Answer)
Spinal radiologic landmarks Explanation: ***Weak Achilles tendon reflex***
- A herniated disc at **L5-S1** typically compresses the **S1 nerve root**, which is responsible for the **Achilles tendon reflex**.
- **S1 radiculopathy** presents with weakness in plantarflexion, diminished or absent Achilles reflex, and sensory loss in the **lateral foot** (matching the patient's symptoms).
*Difficulty walking on heels*
- Difficulty walking on heels (**dorsiflexion weakness**) is primarily associated with **L4-L5 disc herniation** compressing the **L5 nerve root**.
- This symptom indicates **L5 radiculopathy**, which affects the tibialis anterior muscle, not S1.
*Exaggerated patellar tendon reflex*
- An exaggerated patellar tendon reflex (**hyperreflexia**) indicates an **upper motor neuron lesion** or spinal cord compression above the lumbar region.
- A disc herniation at **L5-S1** causes a **lower motor neuron lesion** with diminished reflexes, not hyperreflexia.
*Diminished sensation of the anus and genitalia*
- This symptom, along with urinary incontinence and saddle anesthesia, is characteristic of **cauda equina syndrome**, a surgical emergency.
- The patient lacks urinary incontinence and the specific unilateral pain pattern points to isolated **S1 radiculopathy**, not cauda equina syndrome.
*Diminished sensation of the anterior lateral thigh*
- Sensory loss in the **anterior lateral thigh** is associated with compression of the **lateral femoral cutaneous nerve** or **L2-L4 nerve roots**.
- This pattern is not consistent with **L5-S1 disc herniation**, which causes sensory changes in the lateral foot and posterior leg.
Spinal radiologic landmarks US Medical PG Question 8: A 50-year-old man presents with severe chest pain for a week. His pain increases with breathing and is localized to the right. He has tried over-the-counter medications at home, but they did not help. The patient has a 20-pack-year smoking history and currently smokes 2 packs of cigarettes daily, and he drinks 3 to 4 cans of beer daily before dinner. His temperature is 39.1°C (102.3°F), blood pressure is 127/85 mm Hg, pulse is 109/min, and respirations are 20/min. Respiratory examination shows dullness to percussion from the 7th rib inferiorly at the right midaxillary line, decreased vocal tactile fremitus, and diminished breath sounds in the same area. Chest radiograph is shown in the image. The patient is prepared for thoracocentesis. Which of the following locations would be the most appropriate for insertion of a chest tube?
- A. Below the inferior border of the 7th rib in the midaxillary line
- B. Above the superior border of the 8th rib in the midaxillary line (Correct Answer)
- C. Above the superior border of the 5th rib in the midclavicular line
- D. Below the inferior border of the 5th rib in the midaxillary line
- E. Above the superior border of the 7th rib in the midclavicular line
Spinal radiologic landmarks Explanation: ***Above the superior border of the 8th rib in the midaxillary line***
- The patient presents with symptoms and signs suggestive of a **pleural effusion** (dullness to percussion, decreased fremitus, diminished breath sounds) and potentially an **empyema** given the fever and lung consolidation on the radiograph.
- Thoracocentesis should be performed in the **midaxillary line** between the 6th and 9th ribs to avoid injuring the **diaphragm and abdominal organs**, which can rise as high as the 5th intercostal space during expiration. To prevent damage to the neurovascular bundle that runs along the inferior border of the ribs, the needle should be inserted just **above the superior border** of the rib below the chosen intercostal space.
*Below the inferior border of the 7th rib in the midaxillary line*
- Inserting below the inferior border of the 7th rib increases the risk of injuring the **neurovascular bundle** that runs along the inferior rib margin.
- Such placement might also be too low, increasing the risk of penetrating the **diaphragm** or **abdominal organs**. This location would correspond to the 8th intercostal space, but the 'below inferior border' part is incorrect.
*Above the superior border of the 5th rib in the midclavicular line*
- The **midclavicular line** is typically used for needle decompression of a tension pneumothorax (2nd intercostal space) but is not the preferred site for thoracocentesis due to the risk of striking the lung parenchyma or internal mammary artery.
- Even if considering a pneumothorax, the 5th intercostal space in the midclavicular line is not the standard site, and an effusion is indicated here.
*Below the inferior border of the 5th rib in the midaxillary line*
- Inserting below the inferior border of the 5th rib, similar to option A, risks injury to the **neurovascular bundle**.
- While in the midaxillary line, the 5th rib might be too high for an effusion, and the technique of inserting below the inferior border is incorrect.
*Above the superior border of the 7th rib in the midclavicular line*
- The **midclavicular line** is generally avoided for thoracocentesis of effusions due to the risks mentioned previously and poor drainage if the effusion is posterior.
- The 7th intercostal space in the midclavicular line is also a non-standard and less safe location for this procedure.
Spinal radiologic landmarks US Medical PG Question 9: An MRI of a patient with low back pain reveals compression of the L5 nerve root. Which of the following muscles would most likely show weakness during physical examination?
- A. Tibialis posterior
- B. Tibialis anterior (Correct Answer)
- C. Gastrocnemius
- D. Quadriceps femoris
Spinal radiologic landmarks Explanation: ***Tibialis anterior***
- The **L5 nerve root** primarily innervates muscles responsible for **dorsiflexion** of the foot, with the **tibialis anterior** being the primary dorsiflexor.
- Weakness of the tibialis anterior would manifest as difficulty lifting the front of the foot, potentially leading to a **foot drop** gait.
*Tibialis posterior*
- The **tibialis posterior** is primarily innervated by the **tibial nerve** (S1-S2) and is responsible for **plantarflexion** and **inversion** of the foot.
- Weakness in this muscle would not be the most likely presentation of L5 nerve root compression.
*Gastrocnemius*
- The **gastrocnemius** muscle is primarily innervated by the **tibial nerve** (S1-S2) and is a powerful **plantarflexor** of the foot.
- Weakness in this muscle would indicate an S1 or S2 nerve root issue, not typically L5.
*Quadriceps femoris*
- The **quadriceps femoris** is innervated by the **femoral nerve**, predominantly originating from the **L2, L3, and L4 nerve roots**.
- Weakness would manifest as difficulty extending the knee, which is not characteristic of L5 compression.
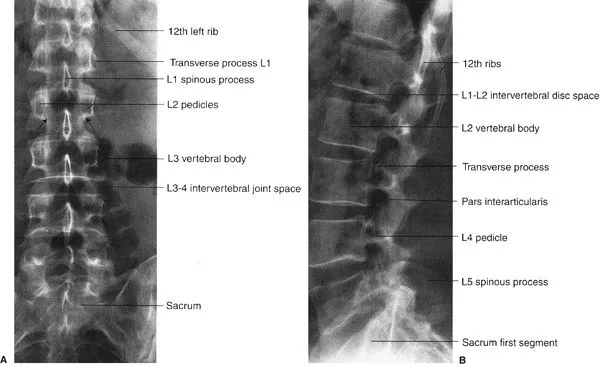
Spinal radiologic landmarks US Medical PG Question 10: A 40-year-old woman is brought to the emergency department by a paramedic team from the scene of a motor vehicle accident where she was the driver. The patient was restrained by a seat belt and was unconscious at the scene. On physical examination, the patient appears to have multiple injuries involving the trunk and extremities. There are no penetrating injuries to the chest. As part of her trauma workup, a CT scan of the chest is ordered. At what vertebral level of the thorax is this image from?
- A. T1
- B. T6
- C. T4
- D. T5
- E. T8 (Correct Answer)
Spinal radiologic landmarks Explanation: ***T8***
- The CT image shows the **inferior vena cava (IVC)** located anterior and to the right of the aorta, and the **esophagus** located posterior to the aorta and slightly to the left. The **azygos vein** is seen to the right of the vertebral body and posterior to the esophagus.
- The **mainstem bronchi** are no longer visible, indicating a level below the carina. The presence of the IVC, aorta, esophagus, and azygos vein with the absence of mainstem bronchi is characteristic of the **T8 vertebral level**.
*T1*
- At the T1 level, the structures would primarily be the **trachea** anterior to the esophagus, with the main great vessels (e.g., brachiocephalic veins and arteries) visible, not the IVC.
- The mainstem bronchi would not yet be visualized at this higher level.
*T6*
- At the T6 level, the **trachea would have already bifurcated into the mainstem bronchi**, which would be prominent structures visible on the CT scan.
- While the aorta and esophagus would be present, the specific arrangement relative to the mainstem bronchi would differentiate it from T8.
*T4*
- The T4 level is typically associated with the **carina**, where the trachea bifurcates into the mainstem bronchi.
- The great vessels would be prominent, but the IVC in its more inferior course would not be as distinctly visualized in this configuration compared to T8.
*T5*
- At the T5 level, the **mainstem bronchi** would still be clearly visible, having just diverged from the trachea.
- While vessels like the aorta are present, the key differentiating factor from T8 is the presence of the mainstem bronchi.
More Spinal radiologic landmarks US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.