Neurological radiologic landmarks US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neurological radiologic landmarks. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neurological radiologic landmarks US Medical PG Question 1: You are seeing a patient in clinic who presents with complaints of weakness. Her physical exam is notable for right sided hyperreflexia, as well as the reflex finding shown in the image below. Where is the most likely location of this patient's lesion?
- A. Postcentral gyrus
- B. Neuromuscular junction
- C. Lateral geniculate nucleus
- D. Internal capsule (Correct Answer)
- E. Subthalamic nucleus
Neurological radiologic landmarks Explanation: ***Internal capsule***
- The combination of **right-sided hyperreflexia** (an upper motor neuron sign) and a positive **Babinski sign** (as implied by a video demonstrating this reflex) points to an upper motor neuron lesion.
- The **internal capsule** contains descending motor pathways, and a lesion here would affect the contralateral side of the body, causing **weakness** and upper motor neuron signs.
*Postcentral gyrus*
- The **postcentral gyrus** is the primary somatosensory cortex and primarily deals with sensory processing, not motor output.
- A lesion here would typically cause **contralateral sensory deficits**, such as numbness or loss of proprioception, rather than motor weakness with hyperreflexia.
*Neuromuscular junction*
- Diseases of the **neuromuscular junction**, such as myasthenia gravis, cause **fatigable weakness** without hyperreflexia or other upper motor neuron signs.
- Reflexes are typically normal or decreased in these conditions.
*Lateral geniculate nucleus*
- The **lateral geniculate nucleus** is a thalamic relay center for visual information.
- Lesions here would result in **visual field deficits** (e.g., homonymous hemianopsia), not motor weakness or hyperreflexia.
*Subthalamic nucleus*
- The **subthalamic nucleus** is part of the basal ganglia and is involved in motor control, particularly in regulating movement initiation and stopping.
- Lesions here are classically associated with **hemiballismus**, which is characterized by wild, flinging movements, rather than weakness and hyperreflexia.
Neurological radiologic landmarks US Medical PG Question 2: A 53-year-old man is brought to the emergency department for confusion. He was in his usual state of health until about 3 hours ago when he tried to use his sandwich to turn off the TV. He also complained to his wife that he had a severe headache. Past medical history is notable for hypertension, which has been difficult to control on multiple medications. His temperature is 36.7°C (98°F), the pulse is 70/min, and the blood pressure is 206/132 mm Hg. On physical exam he is alert and oriented only to himself, repeating over and over that his head hurts. The physical exam is otherwise unremarkable and his neurologic exam is nonfocal. The noncontrast CT scan of the patient's head is shown and reveals an acute intraparenchymal hemorrhage in the basal ganglia. Which of the following diagnostic tests would be most helpful in determining the underlying cause of this patient's hemorrhage?
- A. Lumbar puncture
- B. Electroencephalogram (EEG)
- C. MRI of the brain
- D. CT angiography of the neck
- E. CT angiography of the brain (Correct Answer)
Neurological radiologic landmarks Explanation: ***CT angiography of the brain***
- Following identification of an **intracerebral hemorrhage** on noncontrast CT, **CT angiography (CTA) of the brain** is the most appropriate next diagnostic test to identify underlying vascular abnormalities such as **arteriovenous malformations (AVMs)**, **aneurysms**, **dural arteriovenous fistulas**, or **moyamoya disease**.
- While this patient has severe hypertension (a common cause of basal ganglia hemorrhage), CTA should still be performed to rule out secondary causes, particularly in patients under 70 years old or those with atypical features.
- CTA can be performed rapidly in the acute setting and has high sensitivity for detecting vascular lesions that may require specific treatment.
*MRI of the brain*
- MRI with specialized sequences (GRE, SWI, FLAIR) can provide detailed information about **chronic microhemorrhages**, **cerebral amyloid angiopathy**, **underlying tumors**, or **cavernomas**.
- However, MRI is typically performed **after CTA** in the workup of intracerebral hemorrhage, not as the immediate next step.
- MRI is less readily available in the acute setting and takes longer to perform than CTA.
*CT angiography of the neck*
- This test visualizes the **carotid and vertebral arteries** in the neck to detect **stenosis**, **dissection**, or **atherosclerotic disease**.
- It is not directly useful for identifying the cause of an **intraparenchymal hemorrhage** within the brain substance itself.
*Lumbar puncture*
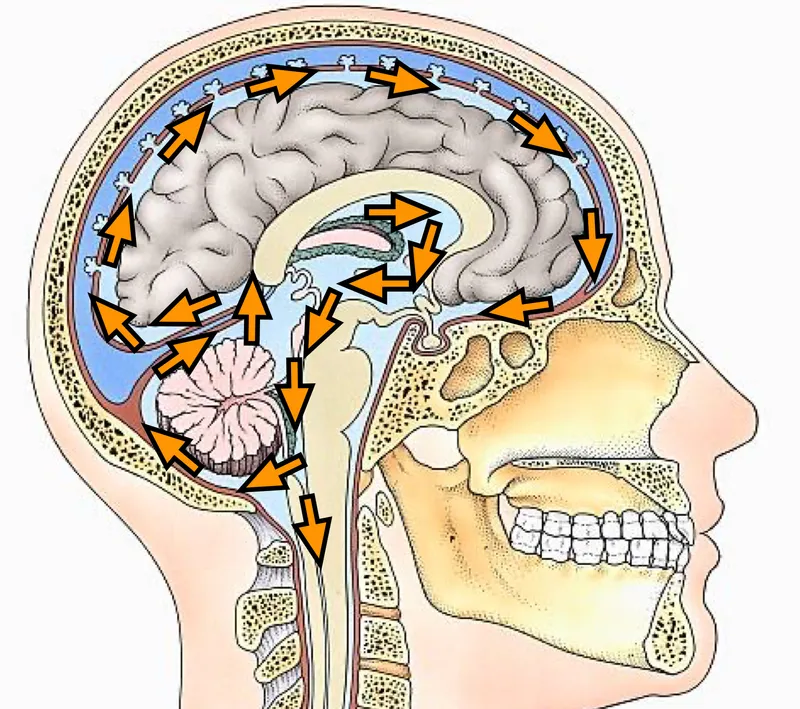
- Lumbar puncture analyzes **cerebrospinal fluid (CSF)** and is primarily used for suspected **subarachnoid hemorrhage** (when CT is negative), **meningitis**, or **encephalitis**.
- It is **contraindicated** in patients with significant intraparenchymal hemorrhage due to risk of herniation from increased intracranial pressure.
*Electroencephalogram (EEG)*
- EEG measures **electrical activity in the brain** and is used to diagnose **seizure disorders** or evaluate altered mental status from metabolic or epileptic causes.
- While confusion can result from seizures, the primary pathology is the **intracerebral hemorrhage** identified on CT, which EEG cannot diagnose or characterize.
Neurological radiologic landmarks US Medical PG Question 3: A 67-year-old female patient is brought to the emergency department after her daughter noticed she has been having meaningless speech. When assessing the patient, she calls the chair a table, and at times would make up new words. She does not appear to be aware of her deficit, and is carrying on an empty conversation. Her speech is fluent, but with paraphasic errors. Her repetition is impaired. On physical examination, a right upper quadrant field-cut is appreciated, with impairment in comprehension and repetition. Which of the following structures is most likely involved in this patient’s presentation?
- A. Superior temporal gyrus (Correct Answer)
- B. Arcuate fasciculus
- C. Inferior frontal gyrus
- D. Frontal lobe, sparing Brodmann's area 44 and 45
- E. Arcuate fasciculus, inferior frontal gyrus, and superior temporal gyrus
Neurological radiologic landmarks Explanation: ***Superior temporal gyrus***
- The patient's presentation of **fluent aphasia** with **paraphasic errors**, **impaired comprehension**, **impaired repetition**, and **lack of awareness** of the deficit is classic for **Wernicke's aphasia**.
- **Wernicke's area**, located in the posterior part of the **superior temporal gyrus** (Brodmann area 22) in the dominant hemisphere, is responsible for language comprehension.
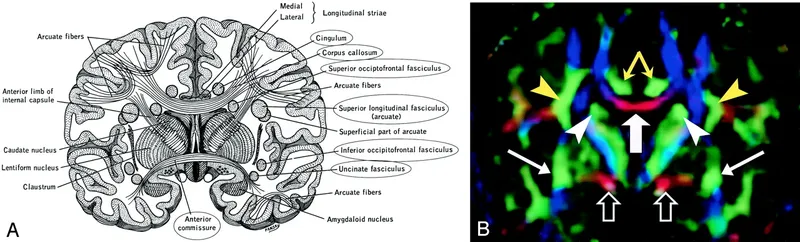
*Arcuate fasciculus*
- Damage to the **arcuate fasciculus** typically causes **conduction aphasia**, characterized by **impaired repetition** with relatively preserved comprehension and fluent speech.
- However, it does not explain the significant comprehension deficits and paraphasic errors seen in this patient to the same extent as a Wernicke's lesion.
*Inferior frontal gyrus*
- The **inferior frontal gyrus** (Brodmann areas 44 and 45) is commonly associated with **Broca's area**, responsible for language production.
- Damage here would result in **non-fluent aphasia** with effortful speech and relatively preserved comprehension, which is contrary to the patient's fluent speech.
*Frontal lobe, sparing Brodmann's area 44 and 45*
- While damage to other parts of the **frontal lobe** can cause various cognitive deficits, sparing Broca's area (44 and 45) would generally not result in the specific pattern of **fluent aphasia** with severe comprehension and repetition impairment seen here.
- This option does not precisely localize the critical language areas affected.
*Arcuate fasciculus, inferior frontal gyrus, and superior temporal gyrus*
- While damage to all these areas would certainly cause severe aphasia, the specific constellation of symptoms—**fluent speech**, **poor comprehension**, **poor repetition**, and **paraphasic errors**—points most directly and primarily to involvement of the **superior temporal gyrus** (Wernicke's area).
- While some level of repetition impairment (seen in Wernicke's aphasia) implies some involvement in the broader language network, a lesion centered in the superior temporal gyrus is the most parsimonious explanation for this classic presentation.
Neurological radiologic landmarks US Medical PG Question 4: A 40-year-old man is brought to the emergency department after sustaining multiple lacerations during a bar fight. The patient’s wife says that he has been showing worsening aggression and has been involved in a lot of arguments and fights for the past 2 years. The patient has no significant past medical or psychiatric history and currently takes no medications. The patient cannot provide any relevant family history since he was adopted as an infant. His vitals are within normal limits. On physical examination, the patient looks apathetic and grimaces repeatedly. Suddenly, his arms start to swing by his side in an uncontrolled manner. Which area of the brain is most likely affected in this patient?
- A. Cerebral cortex
- B. Caudate nucleus (Correct Answer)
- C. Cerebellum
- D. Medulla oblongata
- E. Substantia nigra
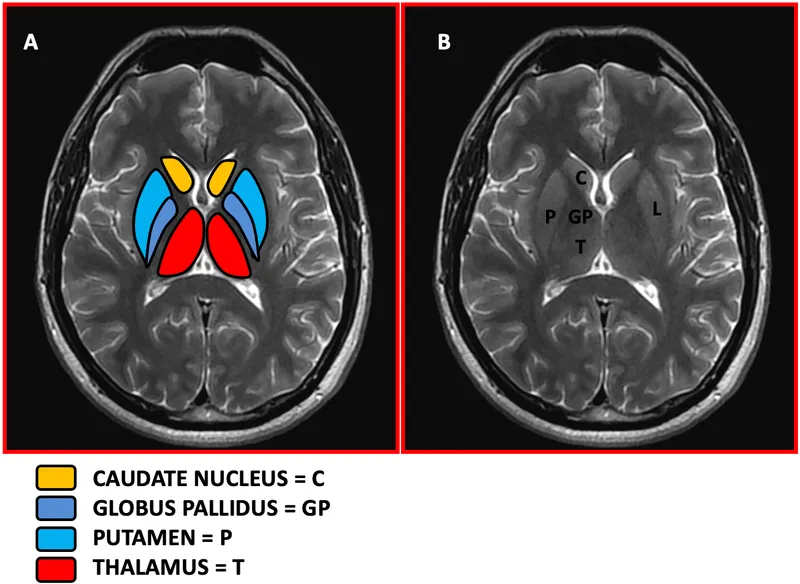
Neurological radiologic landmarks Explanation: **Caudate nucleus**
- The patient exhibits features like **worsening aggression**, **apathy**, and **uncontrolled, sudden movements** of the limbs, which are characteristic of Huntington's disease, a condition primarily affecting the **caudate nucleus**.
- **Huntington's disease** is an autosomal dominant neurodegenerative disorder linked to a trinucleotide repeat expansion (CAG) on chromosome 4, leading to atrophy of the **caudate and putamen**.
*Cerebral cortex*
- While damage to the cerebral cortex can cause personality changes and motor deficits, the specific combination of **choreiform movements** and progressive cognitive/behavioral decline seen here is more indicative of a basal ganglia disorder like Huntington's.
- Cortical lesions more commonly present with **focal neurological deficits** such as hemiparesis, aphasia, or sensory loss, which are not the primary features described.
*Cerebellum*
- Damage to the cerebellum typically results in **ataxia**, **dysmetria**, **intention tremor**, and problems with balance and coordination.
- The patient's **uncontrolled, sudden limb movements** are characteristic of chorea, not cerebellar dysfunction.
*Medulla oblongata*
- The medulla oblongata is crucial for vital autonomic functions such as **breathing, heart rate, and blood pressure regulation**.
- Lesions in this area would likely cause life-threatening symptoms, including **respiratory failure** or severe cardiovascular instability, which are not present in this patient.
*Substantia nigra*
- Damage or degeneration of the substantia nigra is primarily associated with **Parkinson's disease**, leading to symptoms like **bradykinesia**, **rigidity**, **resting tremor**, and **postural instability**.
- The patient's **hyperkinetic movements** (choreiform movements) are opposite to the hypokinetic presentation of Parkinson's disease.
Neurological radiologic landmarks US Medical PG Question 5: In a patient with acute myocardial ischemia, which of the following cardiovascular structures is at greatest risk of damage?
- A. Pulmonary valve
- B. Cardiac conduction system (Correct Answer)
- C. Coronary artery
- D. Cardiac septum
- E. Temporal artery
Neurological radiologic landmarks Explanation: ***Cardiac conduction system***
- The **cardiac conduction system** is highly dependent on a constant oxygen supply, and its disruption by ischemia can lead to serious **arrhythmias** and **heart blocks**.
- Ischemia in critical areas like the **AV node** (supplied by the RCA) or the **bundle branches** can severely impair the heart's electrical activity.
*Pulmonary valve*
- The **pulmonary valve** is primarily a passive structure and is generally not directly damaged by acute myocardial ischemia.
- Its function is more affected by changes in **pulmonary artery pressure** or **ventricular remodeling**, not immediate ischemic injury.
*Coronary artery*
- While **coronary artery disease (CAD)** is the *cause* of myocardial ischemia, the coronary artery itself is not the structure *damaged* in the sense of functional impairment due to lack of blood flow in acute ischemia.
- The damage occurs downstream in the **myocardium** that the artery supplies.
*Cardiac septum*
- The **cardiac septum** can be damaged by myocardial ischemia, particularly the **interventricular septum**, leading to complications like **septal rupture**.
- However, the conduction system is at *greatest* immediate risk of functional damage leading to life-threatening events due to its critical role in rhythm generation.
*Temporal artery*
- The **temporal artery** is a blood vessel located in the head, entirely separate from the heart.
- It is not involved in myocardial ischemia and is not at risk of damage from a cardiac event.
Neurological radiologic landmarks US Medical PG Question 6: A 57-year-old man is brought to the physician for worsening mental status over the past 2 months. His wife reports he was initially experiencing lapses in memory and over the past 3 weeks he has begun having difficulties performing activities of daily living. Yesterday, he became lost heading to the post office down the street. He has hypertension treated with lisinopril and hydrochlorothiazide. Vital signs are within normal limits. He is alert but verbally uncommunicative. Muscle strength is normal. Reflexes are 2+ in bilateral upper and lower extremities. He has diffuse involuntary muscle jerking that can be provoked by loud noises. Mental status examination shows a blunt affect. A complete blood count and serum concentrations of glucose, creatinine, and electrolytes are within the reference range. Which of the following is the most likely diagnosis?
- A. Parkinson's disease
- B. Creutzfeldt-Jakob disease (Correct Answer)
- C. Alzheimer's disease
- D. Normal pressure hydrocephalus
- E. Huntington's disease
Neurological radiologic landmarks Explanation: ***Creutzfeldt-Jakob disease***
- The rapid progression of **dementia**, combined with **myoclonus** (involuntary muscle jerking provoked by loud noises, also known as **startle myoclonus**), is highly characteristic of Creutzfeldt-Jakob disease (CJD).
- CJD is a **prion disease** that causes spongiform encephalopathy, leading to rapidly progressive neurologic decline over weeks to months, typically fatal within a year.
*Parkinson's disease*
- Characterized by a classic triad of **bradykinesia**, **rigidity**, and **resting tremor**, none of which are prominently described in this patient.
- While dementia can occur in later stages of Parkinson's, the **rapid progression** and presence of **myoclonus** are atypical.
*Alzheimer's disease*
- Presents with a **gradual onset** and **slow progression** of memory loss and cognitive decline, typically over many years, which contrasts with this patient's **2-month rapid deterioration**.
- **Myoclonus** is not a common early feature and the rate of progression is inconsistent with Alzheimer's.
*Normal pressure hydrocephalus*
- Classically presents with a triad of **gait disturbance**, **urinary incontinence**, and **dementia**; while dementia is present, the other two key features are not mentioned, and the progression is faster than typically seen.
- The characteristic **myoclonus** is not a feature of normal pressure hydrocephalus.
*Huntington's disease*
- Genetically inherited disorder characterized by **chorea** (involuntary, jerky movements) and psychiatric symptoms, followed by dementia.
- The onset is typically earlier (30s-40s) and the primary motor symptom is chorea, not the **startle myoclonus with rapid progression** observed here.
Neurological radiologic landmarks US Medical PG Question 7: An 82-year-old right-handed woman is brought in by ambulance after being found down in her home. On presentation, she is found to be awake but does not follow directions or respond to questions. She is able to speak and produces a fluent string of nonsensical words and sounds. She does not appear to be bothered by her deficits. Subsequent neurologic exam finds that the patient is unable to comprehend any instructions and is also unable to repeat phrases. CT scan reveals an acute stroke to her left hemisphere. Damage to which of the following structures would be most likely to result in this pattern of deficits?
- A. Precentral gyrus
- B. Superior temporal gyrus (Correct Answer)
- C. Arcuate fasciculus
- D. Inferior frontal gyrus
- E. Watershed zone
Neurological radiologic landmarks Explanation: ***Superior temporal gyrus***
- This patient presents with **fluent aphasia** (speaking nonsensical words), severely impaired **comprehension**, and impaired **repetition**. This triad is characteristic of **Wernicke's aphasia**.
- **Wernicke's area**, responsible for language comprehension, is located in the **posterior part of the superior temporal gyrus** in the dominant hemisphere (typically left).
*Precentral gyrus*
- The **precentral gyrus** contains the **primary motor cortex** and its damage would primarily cause contralateral motor deficits (e.g., **hemiparesis** or **hemiplegia**).
- This area is not directly involved in language comprehension or production of fluent but nonsensical speech.
*Arcuate fasciculus*
- Damage to the **arcuate fasciculus**, a white matter tract connecting Broca's and Wernicke's areas, results in **conduction aphasia**.
- In **conduction aphasia**, comprehension and fluency are relatively preserved, but **repetition is severely impaired**. This patient also has impaired comprehension.
*Inferior frontal gyrus*
- The **inferior frontal gyrus** houses **Broca's area**, which is responsible for **language production and motor aspects of speech**.
- Damage to this area typically causes **Broca's aphasia**, characterized by **non-fluent speech**, preserved comprehension, and impaired repetition. This patient has fluent speech.
*Watershed zone*
- **Watershed infarcts** occur at the borders between major arterial territories due to hypoperfusion, often leading to **transcortical aphasias**.
- While transcortical sensory aphasia involves impaired comprehension and fluent speech, **repetition is preserved**, which is not the case here.
Neurological radiologic landmarks US Medical PG Question 8: Arrange in sequence the structures involved in the direct pathway (1=Striatum, 2=GPi, 3=Thalamus, 4=Cortex output, 5=Cortex input):-
- A. 1,3,4,2,5
- B. 5,1,2,3,4 (Correct Answer)
- C. 1,2,3,4,5
- D. 5,4,2,3,1
- E. 5,1,3,2,4
Neurological radiologic landmarks Explanation: ***5,1,2,3,4***
- The direct pathway of the basal ganglia begins with the **cortex** (5) sending excitatory signals to the **striatum** (1).
- The striatum then inhibits the **internal globus pallidus (GPi)** (2), which disinhibits the **thalamus** (3), leading to excitation of the **cortex** (4).
- This is the correct sequence: **Cortex input → Striatum → GPi → Thalamus → Cortex output**.
*1,3,4,2,5*
- This sequence is incorrect as it starts with the striatum instead of cortical input.
- The direct pathway does not begin with striatal activity; the cortex must first activate the striatum.
*1,2,3,4,5*
- This order is incorrect because it implies the pathway starts at the striatum rather than the cortex.
- The cortex should be the starting point (5) and the ending point (4) of the motor loop.
*5,4,2,3,1*
- This sequence is incorrect as it places cortex output (4) before the striatum receives input.
- This reverses the functional flow and does not follow the **disinhibitory mechanism** of the direct pathway.
*5,1,3,2,4*
- This sequence incorrectly places the thalamus (3) before the GPi (2).
- In the direct pathway, the striatum must first inhibit the GPi before the thalamus can be disinhibited.
Neurological radiologic landmarks US Medical PG Question 9: A 68-year-old man is brought to the emergency department by ambulance after he was found to be altered at home. Specifically, his wife says that he fell and was unable to get back up while walking to bed. When she approached him, she found that he was unable to move his left leg. His past medical history is significant for hypertension, atrial fibrillation, and diabetes. In addition, he has a 20-pack-year smoking history. On presentation, he is found to still have difficulty moving his left leg though motor function in his left arm is completely intact. The cause of this patient's symptoms most likely occurred in an artery supplying which of the following brain regions?
- A. Motor cortex (ACA) (Correct Answer)
- B. Cerebellum (PICA/SCA)
- C. Occipital cortex (PCA)
- D. Brainstem (Vertebrobasilar)
- E. Motor cortex (MCA)
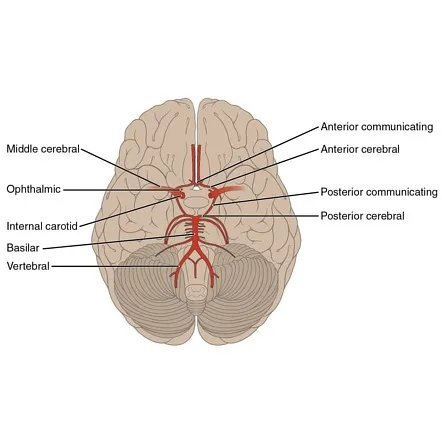
Neurological radiologic landmarks Explanation: ***Motor cortex (ACA)***
- The patient's inability to move his **left leg** while his **left arm** remains intact points to an injury in the **right cerebral hemisphere** affecting the leg area of the motor cortex.
- The leg area of the **primary motor cortex** is primarily supplied by the **anterior cerebral artery (ACA)**, making an ACA stroke the most likely cause.
*Motor cortex (MCA)*
- The **middle cerebral artery (MCA)** primarily supplies the motor cortex areas responsible for the **face and arm**, not typically isolated leg weakness.
- If the MCA were affected, you would expect to see involvement of the face and/or arm on the contralateral side in addition to leg weakness.
*Brainstem (Vertebrobasilar)*
- A **brainstem stroke** would likely present with more widespread neurological deficits, including **cranial nerve palsies**, ataxia, or altered consciousness.
- Isolated contralateral leg weakness without arm involvement is not characteristic of a brainstem lesion.
*Cerebellum (PICA/SCA)*
- The **cerebellum** is primarily involved in **coordination and balance**, not direct motor strength.
- A cerebellar stroke would present with symptoms like **ataxia**, dysarthria, or nystagmus, not isolated paralysis.
*Occipital cortex (PCA)*
- The **occipital cortex** is primarily responsible for **vision**.
- A posterior cerebral artery (PCA) stroke would typically cause **visual field defects** (e.g., contralateral homonymous hemianopia) rather than motor weakness.
Neurological radiologic landmarks US Medical PG Question 10: A 65-year-old man is referred by his primary care provider to a neurologist for leg pain. He reports a 6-month history of progressive bilateral lower extremity pain that is worse in his left leg. The pain is 5/10 in severity at its worst and is described as a "burning" pain. He has noticed that the pain is acutely worse when he walks downhill. He has started riding his stationary bike more often as it relieves his pain. His past medical history is notable for hypertension, diabetes mellitus, and a prior myocardial infarction. He also sustained a distal radius fracture the previous year after falling on his outstretched hand. He takes aspirin, atorvastatin, metformin, glyburide, enalapril, and metoprolol. He has a 30-pack-year smoking history and drinks 2-3 glasses of wine with dinner every night. His temperature is 99°F (37.2°C), blood pressure is 145/85 mmHg, pulse is 91/min, and respirations are 18/min. On exam, he is well-appearing and in no acute distress. A straight leg raise is negative. A valsalva maneuver does not worsen his pain. Which of the following is the most appropriate test to confirm this patient's diagnosis?
- A. Electromyography
- B. Ankle-brachial index
- C. Computerized tomography myelography
- D. Magnetic resonance imaging (Correct Answer)
- E. Radiography
Neurological radiologic landmarks Explanation: **Magnetic resonance imaging**
- **Magnetic resonance imaging (MRI)** is the most appropriate test for diagnosing **lumbar spinal stenosis** because it provides detailed imaging of soft tissues, including the **spinal cord, nerve roots, and intervertebral discs**.
- The patient's symptoms of bilateral lower extremity pain, worse with downhill walking and relieved by stationary biking (which typically involves a flexed spine), are classic for **neurogenic claudication** caused by spinal stenosis.
*Electromyography*
- **Electromyography (EMG)** measures electrical activity of muscles and can identify **radiculopathy** or **neuropathy** but does not directly visualize the spinal canal or its contents to diagnose the cause of nerve compression.
- While it could show nerve root involvement, it wouldn't be the primary diagnostic test to confirm **spinal stenosis** itself.
*Ankle-brachial index*
- The **ankle-brachial index (ABI)** is used to diagnose **peripheral artery disease (PAD)**, which can also cause leg pain with activity (**vascular claudication**).
- However, the patient's pain being worse with downhill walking and relieved by spine flexion (like on a stationary bike) is more consistent with **neurogenic claudication** than vascular claudication.
*Computerized tomography myelography*
- **CT myelography** involves injecting contrast into the spinal canal and then performing a CT scan. While it can visualize the spinal canal, it is more invasive than MRI and exposes the patient to **ionizing radiation**.
- It is typically reserved for cases where MRI is contraindicated (e.g., pacemakers) or when MRI findings are inconclusive.
*Radiography*
- **Radiography (X-rays)** can show bony changes such as **spondylosis** and **degenerative disc disease**, which are often associated with spinal stenosis.
- However, X-rays do not directly visualize the **spinal cord, nerve roots, or soft tissue compression**, making them inadequate for confirming spinal stenosis as the cause of neurogenic claudication.
More Neurological radiologic landmarks US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.