Contrast-enhanced landmark identification US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Contrast-enhanced landmark identification. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Contrast-enhanced landmark identification US Medical PG Question 1: A 57-year-old man presents to his family physician for a routine exam. He feels well and reports no new complaints since his visit last year. Last year, he had a colonoscopy which showed no polyps, a low dose chest computerized tomography (CT) scan that showed no masses, and routine labs which showed a fasting glucose of 93 mg/dL. He is relatively sedentary and has a body mass index (BMI) of 24 kg/m^2. He has a history of using methamphetamines, alcohol (4-5 drinks per day since age 30), and tobacco (1 pack per day since age 18), but he joined Alcoholics Anonymous and has been in recovery, not using any of these for the past 7 years. Which of the following is indicated at this time?
- A. Colonoscopy
- B. Chest computerized tomography (CT) scan (Correct Answer)
- C. Abdominal ultrasound
- D. Chest radiograph
- E. Fasting glucose
Contrast-enhanced landmark identification Explanation: ***Chest computerized tomography (CT) scan***
- This patient has a significant **smoking history** (1 pack per day since age 18 = **39 pack-years**) and is 57 years old, placing him in a high-risk group for **lung cancer**.
- Annual low-dose CT screening for lung cancer is recommended for individuals aged 50-80 with a 20 pack-year smoking history who currently smoke or have quit within the past 15 years.
- He meets all criteria: age 57, 39 pack-years, and quit only 7 years ago (within the 15-year window).
- Since he had screening **last year** with no masses, this year's visit represents the appropriate time for his **annual follow-up screening**.
*Colonoscopy*
- The patient had a colonoscopy last year with **no polyps**, suggesting he is at average risk for colorectal cancer.
- For individuals at average risk with normal findings, repeat screening colonoscopy is typically recommended every **10 years** (or every 5 years for flexible sigmoidoscopy), not annually.
*Abdominal ultrasound*
- One-time abdominal ultrasound screening for **abdominal aortic aneurysm (AAA)** is recommended for men aged 65-75 who have ever smoked.
- This patient is only 57 years old and does not yet meet the age criteria for AAA screening.
*Chest radiograph*
- While a chest radiograph can identify some lung abnormalities, a **low-dose CT scan** is far more sensitive and specific for detecting early-stage lung cancer in high-risk populations.
- Chest radiography is **not recommended** as a screening tool for lung cancer due to its lower sensitivity and lack of mortality benefit in trials.
*Fasting glucose*
- The patient had a **normal fasting glucose** of 93 mg/dL last year, and there are no new symptoms suggestive of diabetes.
- For asymptomatic adults with normal glucose, diabetes screening is typically repeated every **3 years**.
- Annual re-screening is not indicated without new risk factors or symptoms.
Contrast-enhanced landmark identification US Medical PG Question 2: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Contrast-enhanced landmark identification Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
Contrast-enhanced landmark identification US Medical PG Question 3: A 49-year-old male presents to his primary care physician for the first time in twelve years. His chief complaint is a new onset of diarrhea, which nothing seems to improve. He first noticed this diarrhea about a month ago. He complains of greasy stools, which leave a residue in his toilet bowl. Review of systems is notable for alcohol consumption of 12-16 cans of beer per day for the last two decades. Additionally, the patient endorses losing 12 lbs unintentionally over the last month. Vital signs are within normal limits and stable. Exam demonstrates a male who appears older than stated age; abdominal exam is notable for epigastric tenderness to palpation. What is the next step in diagnosis?
- A. Endoscopic retrograde cholangiopancreatography (ERCP)
- B. Somatostatin receptor scintigraphy
- C. d-Xylose absorption test
- D. CT abdomen with IV contrast (Correct Answer)
- E. EGD with biopsy of gastric mucosa
Contrast-enhanced landmark identification Explanation: ***CT abdomen with IV contrast***
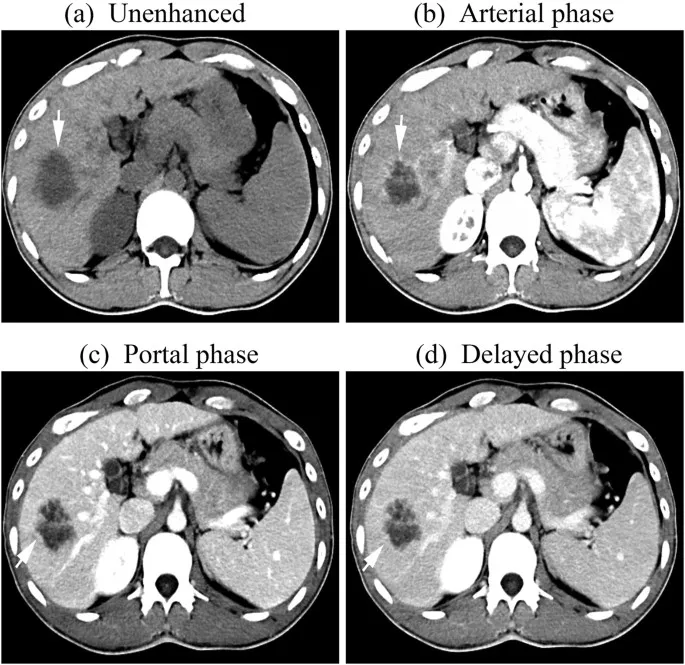
- Given the patient's history of **heavy chronic alcohol intake**, **weight loss**, **new-onset diarrhea**, **greasy stools (steatorrhea)**, and **epigastric tenderness**, **chronic pancreatitis** with **exocrine pancreatic insufficiency** is highly suspected.
- A **CT scan of the abdomen with IV contrast** is the initial diagnostic test of choice to evaluate the pancreas for changes consistent with chronic pancreatitis, such as **calcifications**, **ductal dilation**, or **atrophy**, and also to rule out other causes like pancreatic tumors.
*Endoscopic retrograde cholangiopancreatography (ERCP)*
- **ERCP** is an **invasive procedure** primarily used therapeutically for conditions like **bile duct stones** or **strictures**, or sometimes for detailed pancreatic duct imaging.
- It is generally **not the first-line diagnostic test** for suspected chronic pancreatitis due to its invasive nature and risk of complications like pancreatitis.
*Somatostatin receptor scintigraphy*
- This imaging technique is primarily used to detect **neuroendocrine tumors (NETs)**, particularly those that express somatostatin receptors.
- While diarrhea can be a symptom of certain NETs (e.g., **VIPoma**), the patient's strong history of chronic alcohol abuse and steatorrhea points more directly to pancreatic exocrine insufficiency, making a CT scan a more appropriate initial investigation.
*d-Xylose absorption test*
- The **d-xylose absorption test** is used to assess **small bowel mucosal function** and differentiate between primary mucosal disease and pancreatic insufficiency as causes of malabsorption.
- In this case, with strong indicators for pancreatic dysfunction (greasy stools, chronic alcohol use), directly evaluating the pancreas via imaging is a more targeted next step.
*EGD with biopsy of gastric mucosa*
- **Esophagogastroduodenoscopy (EGD)** with biopsy is indicated for evaluating upper gastrointestinal symptoms, such as **dysphagia**, **gastric ulcers**, or **celiac disease**.
- While it could evaluate for celiac disease, the patient's history of heavy alcohol use and greasy stools makes **pancreatic insufficiency** a more probable cause of malabsorption, and EGD would not directly assess pancreatic function or structure.
Contrast-enhanced landmark identification US Medical PG Question 4: A 74-year-old man is brought to the emergency department after he had copious amounts of blood-stained stools. Minutes later, he turned sweaty, felt light-headed, and collapsed into his wife’s arms. Upon admission, he is found to have a blood pressure of 78/40 mm Hg, a pulse of 140/min, and oxygen saturation of 98%. His family history is relevant for both gastric and colorectal cancer. His personal history is relevant for hypertension, for which he takes amlodipine. After an initial successful resuscitation with intravenous fluids, which of the following should be the first step in approaching this case?
- A. Radionuclide imaging
- B. Mesenteric angiography
- C. Upper endoscopy (Correct Answer)
- D. Colonoscopy
- E. Nasogastric lavage
Contrast-enhanced landmark identification Explanation: ***Upper endoscopy***
- After **initial hemodynamic stabilization** (as stated in the question), **early upper endoscopy** is the recommended first-line approach for patients with acute GI bleeding.
- **Upper GI sources** must be ruled out first, even in patients presenting with hematochezia (blood-stained stools), as **10-15% of cases** with bright red blood per rectum originate from an upper GI source.
- Upper endoscopy is both **diagnostic and therapeutic**, allowing for immediate intervention (banding, sclerotherapy, thermal coagulation, clipping) if a bleeding source is identified.
- **Current ACG/ASGE guidelines** recommend endoscopy **within 24 hours** (ideally within 12 hours) after resuscitation in patients with acute upper GI bleeding.
- The degree of **hemodynamic instability** in this patient (BP 78/40, HR 140) suggests a brisk bleed more consistent with an upper GI source.
*Nasogastric lavage*
- NG lavage has **low sensitivity (42-84%)** for upper GI bleeding and can miss up to 15% of cases.
- It is **no longer routinely recommended** by current guidelines as it delays definitive diagnosis and treatment without providing therapeutic benefit.
- Modern practice favors proceeding directly to endoscopy after stabilization rather than performing NG lavage first.
*Radionuclide imaging*
- **Tagged RBC scan** is useful for **intermittent or slow bleeding** (0.1-0.5 mL/min) when endoscopy is non-diagnostic.
- Not appropriate as the **first step** in an acute, massive bleed requiring immediate source localization and potential intervention.
- Provides localization but no therapeutic capability.
*Mesenteric angiography*
- Indicated for **active, brisk bleeding** (>0.5-1 mL/min) when endoscopy fails to identify the source or when immediate therapeutic embolization is needed.
- Can be both diagnostic and therapeutic but is typically a **second-line intervention** after endoscopy.
- Requires active bleeding at the time of the procedure to visualize the source.
*Colonoscopy*
- **Colonoscopy** is the appropriate diagnostic tool for **lower GI bleeding** after upper GI sources have been excluded.
- Should be performed **after upper endoscopy** rules out an upper source, particularly in patients with this degree of hemodynamic compromise.
- Requires adequate bowel preparation for optimal visualization, which may delay diagnosis.
Contrast-enhanced landmark identification US Medical PG Question 5: A 37-year-old woman presents to the Emergency Department after 8 hours of left sided flank pain that radiates to her groin and pelvic pain while urinating. Her medical history is relevant for multiple episodes of urinary tract infections, some requiring hospitalization, and intravenous antibiotics. In the hospital, her blood pressure is 125/83 mm Hg, pulse of 88/min, a respiratory rate of 28/min, and a body temperature of 36.5°C (97.7°F). On physical examination, she has left costovertebral tenderness and lower abdominal pain. Laboratory studies include a negative pregnancy test, mild azotemia, and a urinary dipstick that is positive for blood. Which of the following initial tests would be most useful in the diagnosis of this case?
- A. Urine osmolality
- B. Fractional excretion of sodium (FeNa+)
- C. Renal ultrasonography (Correct Answer)
- D. Contrast abdominal computed tomography
- E. Blood urea nitrogen (BUN): serum creatinine (SCr) ratio
Contrast-enhanced landmark identification Explanation: ***Renal ultrasonography***
- This is the most appropriate initial imaging test to evaluate for **kidney stones** (given the flank pain radiating to groin and hematuria) and **hydronephrosis** (which can indicate obstruction) and assess for signs of **pyelonephritis** (given the history of recurrent UTIs and CVA tenderness).
- It is **non-invasive**, readily available, and avoids radiation exposure, making it suitable as a first-line diagnostic tool in this setting.
*Urine osmolality*
- This test primarily assesses the kidney's ability to **concentrate urine**, which is more relevant for evaluating fluid balance, diabetes insipidus, or other renal tubular disorders.
- It would not directly diagnose the cause of acute flank pain or urinary tract obstruction.
*Fractional excretion of sodium (FeNa+)*
- FeNa+ is used to differentiate between **prerenal azotemia** and **acute tubular necrosis**, indicating the kidney's response to hypoperfusion.
- While the patient has mild azotemia, FeNa+ would not identify the underlying cause of the flank pain, hematuria, or potential obstruction.
*Contrast abdominal computed tomography*
- While highly sensitive for diagnosing kidney stones and other renal pathologies, **contrast CT** exposes the patient to **ionizing radiation** and risks associated with contrast agents (e.g., contrast-induced nephropathy), especially with pre-existing azotemia.
- It is often reserved for cases where ultrasound is inconclusive or more detailed anatomical information is needed.
*Blood urea nitrogen (BUN): serum creatinine (SCr) ratio*
- This ratio is primarily used to differentiate between **prerenal** causes of acute kidney injury (high ratio, e.g., >20:1) and **intrinsic renal** causes (lower ratio, e.g., <15:1).
- While it can provide insight into the etiology of azotemia, it does not directly identify the cause of the patient's acute flank pain or potential urinary tract obstruction.
Contrast-enhanced landmark identification US Medical PG Question 6: A 67-year-old man presents to his primary care provider with bloody urine. He first noticed the blood 1 week ago. He otherwise feels healthy. His past medical history is significant for type 2 diabetes mellitus for 18 years, for which he takes insulin injections. He has smoked 30–40 cigarettes per day for the past 29 years and drinks alcohol socially. Today his vital signs include: temperature 36.6°C (97.8°F), blood pressure 135/82 mm Hg, and heart rate 105/min. There are no findings on physical examination. Urinalysis shows 15–20 red cells/high power field. Which of the following is the next best test to evaluate this patient’s condition?
- A. Prostate-specific antigen
- B. Urine cytology
- C. Urinary markers
- D. Biopsy
- E. Contrast-enhanced CT (Correct Answer)
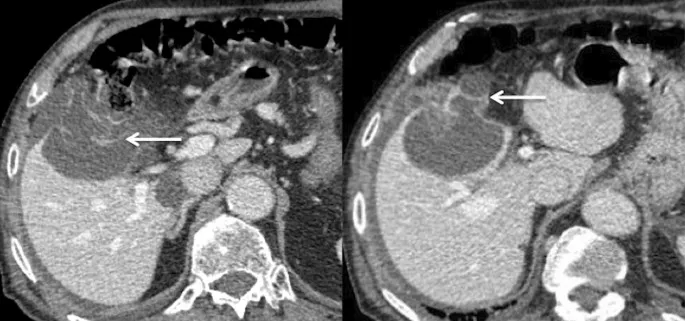
Contrast-enhanced landmark identification Explanation: ***Contrast-enhanced CT***
- This patient presents with **painless gross hematuria** and significant risk factors, including a 29-year history of **heavy smoking** and age, which raise suspicion for **urothelial carcinoma** (e.g., bladder cancer, renal cell carcinoma).
- A **contrast-enhanced CT** of the abdomen and pelvis is the most appropriate initial imaging study to evaluate the entire urinary tract for masses, stones, or other structural abnormalities causing the hematuria.
*Prostate-specific antigen*
- This test is primarily used for **prostate cancer screening** and monitoring, and while prostate issues can cause hematuria, the absence of urinary obstruction symptoms and the patient's age and smoking history make other causes more likely.
- An elevated **PSA** would not explain gross, painless hematuria in this context and would not be the initial diagnostic step for evaluating the urinary tract in general.
*Urine cytology*
- While urine cytology can detect **malignant cells**, its sensitivity for urothelial carcinoma is variable and often low, especially for low-grade tumors.
- A negative cytology does not rule out cancer, and an imaging study is still necessary to **localize the source** of bleeding and assess for structural abnormalities.
*Urinary markers*
- Various **urinary markers** (e.g., BTA stat, NMP22) are available for bladder cancer detection, but they are generally less sensitive and specific than imaging or cystoscopy.
- These markers are often used in conjunction with other tests or for surveillance, but not as the initial definitive test for **gross hematuria** in a high-risk patient.
*Biopsy*
- A biopsy is a **definitive diagnostic step** for confirming cancer but requires an identified lesion to target.
- Before a biopsy can be performed, imaging (like CT) is needed to **locate any potential tumors** in the kidneys, ureters, or bladder that would then be amenable to biopsy (e.g., via cystoscopy with biopsy or renal biopsy).
Contrast-enhanced landmark identification US Medical PG Question 7: A CT scan of the abdomen reveals a mass in the pancreatic uncinate process. Which of the following structures is most likely to be compressed by this mass?
- A. Common bile duct
- B. Portal vein
- C. Splenic vein
- D. Superior mesenteric vein (Correct Answer)
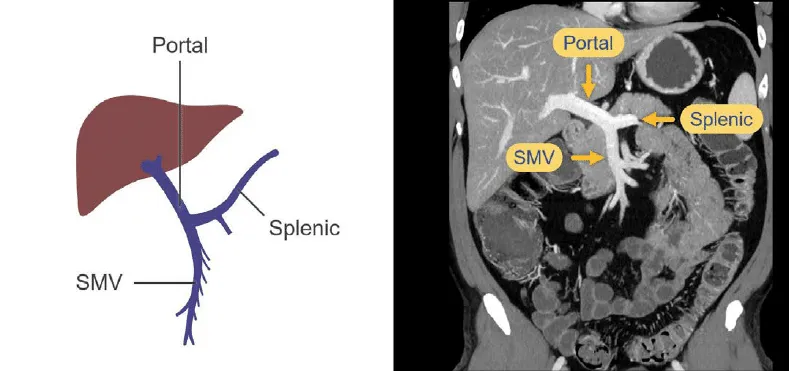
Contrast-enhanced landmark identification Explanation: ***Superior mesenteric vein***
- The **uncinate process** of the pancreas hooks around the **superior mesenteric vessels**. Therefore, a mass in this region would most directly compress the **superior mesenteric vein (SMV)** and artery (SMA).
- Compression of the SMV can lead to **venous outflow obstruction** from the small intestine, potentially causing **bowel ischemia** or edema.
*Common bile duct*
- The **common bile duct** passes through the **head of the pancreas**, not typically the uncinate process.
- Compression of the common bile duct would more commonly be associated with masses in the **head of the pancreas**, leading to **jaundice**.
*Portal vein*
- The **portal vein** is formed by the union of the **splenic vein** and the **superior mesenteric vein**, generally posterior to the neck of the pancreas.
- While pancreatic masses can affect the portal vein, a mass specifically in the uncinate process would more directly impinge on the SMV before significantly affecting the main portal vein, which is superior and posterior to the uncinate process.
*Splenic vein*
- The **splenic vein** runs along the **posterior aspect of the body and tail of the pancreas**.
- A mass in the uncinate process, located at the inferior margin of the head, is relatively distant from the splenic vein.
Contrast-enhanced landmark identification US Medical PG Question 8: A 43-year-old man presents with acute-onset left flank pain for the past 6 hours. He describes the pain as severe, intermittent, colicky, and “coming in waves”, and he points to the area of the left costovertebral angle (CVA). He says he recently has been restricting oral liquid intake to only 2 glasses of water per day based on the advice of his healer. He also reports nausea and vomiting. The patient has a history of hypertension, gout, and type 2 diabetes mellitus. He is afebrile, and his vital signs are within normal limits. On physical examination, he is writhing in pain and moaning. There is exquisite left CVA tenderness. A urinalysis shows gross hematuria. Which of the following is the next best step in the management of this patient?
- A. Non-contrast CT of the abdomen
- B. Contrast CT of the abdomen and pelvis
- C. Supine abdominal radiograph
- D. Renal ultrasound
- E. Non-contrast CT of the abdomen and pelvis (Correct Answer)
Contrast-enhanced landmark identification Explanation: **Non-contrast CT of the abdomen and pelvis**
- **Non-contrast CT of the abdomen and pelvis** is the gold standard for diagnosing urolithiasis, providing high sensitivity and specificity for detecting stones, identifying their size and location, and assessing for hydronephrosis.
- The patient's presentation with **acute-onset, severe, colicky flank pain**, nausea, vomiting, gross hematuria, and CVA tenderness is highly suggestive of **renal colic due to a kidney stone**.
*Non-contrast CT of the abdomen*
- This option is **insufficient** as kidney stones can be located in the ureters within the pelvis; a scan of the abdomen alone might miss stones in the distal ureter.
- While a non-contrast CT is appropriate, the scope of only the abdomen is **incomplete** for evaluating the entire urinary tract that might be affected by stones.
*Contrast CT of the abdomen and pelvis*
- **Contrast-enhanced CT is generally not indicated** for the initial evaluation of suspected renal colic due to urolithiasis because it can obscure the visualization of urinary stones.
- The use of contrast also carries risks such as **allergic reaction** and **contrast-induced nephropathy**, which are unnecessary in this acute, non-complicated setting.
*Supine abdominal radiograph*
- A supine abdominal radiograph (KUB) has **limited sensitivity** for detecting kidney stones, especially radiolucent stones (e.g., uric acid stones) or small stones.
- It also provides **poor anatomical detail** and cannot assess for hydronephrosis or other complications as effectively as CT.
*Renal ultrasound*
- Renal ultrasound can detect **hydronephrosis** and some kidney stones but is less sensitive than CT for visualizing smaller stones, especially in the ureters.
- Its diagnostic utility can be **limited by body habitus** and operator dependence, making it less reliable as a primary diagnostic tool for acute renal colic.
Contrast-enhanced landmark identification US Medical PG Question 9: A 55-year-old man presents to urgent care for weakness and weight loss. He states for the past several months he has felt progressively weaker and has lost 25 pounds. The patient also endorses intermittent abdominal pain. The patient has not seen a physician in 30 years and recalls being current on most of his vaccinations. He says that a few years ago, he went to the emergency department due to abdominal pain and was found to have increased liver enzymes due to excessive alcohol use and incidental gallstones. The patient has a 50 pack-year smoking history. His temperature is 99.5°F (37.5°C), blood pressure is 161/108 mmHg, pulse is 90/min, respirations are 17/min, and oxygen saturation is 95% on room air. Physical exam reveals an emaciated man. The patient has a negative Murphy's sign and his abdomen is non-tender. Cardiopulmonary exam is within normal limits. Which of the following is the next best step in management?
- A. CT scan of the abdomen (Correct Answer)
- B. CT scan of the liver
- C. Right upper quadrant ultrasound
- D. HIDA scan
- E. Smoking cessation advice and primary care follow up
Contrast-enhanced landmark identification Explanation: ***CT scan of the abdomen***
- The patient presents with **constitutional symptoms** (weakness, significant weight loss), **intermittent abdominal pain**, and a **50 pack-year smoking history**, which are red flags for potential **malignancy**.
- A CT scan of the abdomen is the most appropriate initial imaging study to **evaluate for masses, metastases, or other pathologies** that would explain these symptoms comprehensively.
*CT scan of the liver*
- While the patient has a history of elevated liver enzymes and gallstones, focusing solely on the liver might **miss other abdominal pathologies** that could explain his symptoms.
- A CT of the liver is a more targeted scan, usually performed after a broader abdominal assessment suggests a primary liver issue.
*Right upper quadrant ultrasound*
- An ultrasound of the right upper quadrant is excellent for evaluating the **gallbladder, bile ducts, and liver parenchyma** for stones, cholecystitis, or focal lesions.
- However, it has **limited ability to visualize the retroperitoneum, pancreas, or other bowel structures** which could be the source of the patient's symptoms.
*HIDA scan*
- A HIDA scan is used to assess **gallbladder function** and is primarily indicated for suspected **acute cholecystitis** when ultrasound findings are equivocal, or for chronic gallbladder dysfunction.
- The patient's presentation of generalized weakness, significant weight loss, and non-tender abdomen does not acutely point towards biliary obstruction or acute cholecystitis.
*Smoking cessation advice and primary care follow up*
- While **smoking cessation** is crucial for long-term health, and **primary care follow-up** is necessary, these steps are not the *next best step in management* for a patient presenting with alarming symptoms of weakness, significant weight loss, and abdominal pain.
- These are important secondary measures, but the immediate concern is to **investigate the cause of his current severe symptoms**.
Contrast-enhanced landmark identification US Medical PG Question 10: A 22-year-old Caucasian male is stabbed in his left flank, injuring his left kidney. As the surgeon undertakes operative repair, she reviews relevant renal anatomy. All of the following are correct regarding the left kidney EXCEPT?
- A. The left kidney has a longer renal vein than the right kidney
- B. The left kidney underlies the left 12th rib
- C. The left kidney moves vertically during deep breathing
- D. The left kidney has a longer renal artery than the right kidney (Correct Answer)
- E. The left kidney lies between T12 and L3
Contrast-enhanced landmark identification Explanation: ***The left kidney has a longer renal artery than the right kidney***
- The **aorta** lies to the left of the midline, so the **right renal artery** must traverse a greater distance to reach the right kidney.
- Therefore, the right renal artery is longer than the left renal artery.
*The left kidney has a longer renal vein than the right kidney*
- The **inferior vena cava (IVC)** is positioned to the right of the midline, requiring the **left renal vein** to cross the aorta to drain.
- This anatomical arrangement makes the left renal vein longer than the right renal vein.
*The left kidney underlies the left 12th rib*
- The kidneys are retroperitoneal organs, and the 12th rib provides significant posterior protection for **both kidneys**.
- The superior pole of the left kidney typically extends to the level of the **11th and 12th ribs**.
*The left kidney moves vertically during deep breathing*
- The kidneys are surrounded by **perirenal fat** and are influenced by the diaphragm's movement.
- During **deep inspiration**, the diaphragm descends, causing both kidneys to move vertically by 2-3 cm.
*The left kidney lies between T12 and L3*
- The kidneys are situated in the retroperitoneum, generally extending from the level of the **T12 vertebra** to the **L3 vertebra**.
- The left kidney is typically positioned slightly higher than the right kidney.
More Contrast-enhanced landmark identification US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.