Pharyngeal clefts US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pharyngeal clefts. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pharyngeal clefts US Medical PG Question 1: A 20-year-old man presents with a painless neck mass that has gradually increased in size. The mass is anteromedial to the right sternocleidomastoid muscle and has been present for 3 years. The mass increased in size and became more tender following an upper respiratory infection. An ultrasound of the neck identifies a single, round cystic mass with uniform, low echogenicity, and no internal septations. A contrast-enhanced CT scan of the neck shows a homogeneous mass with low attenuation centrally and with smooth rim enhancement. Which of the following is the most likely diagnosis?
- A. First branchial cleft cyst
- B. Sternomastoid tumor
- C. Second branchial cleft cyst (Correct Answer)
- D. Ectopic thyroid tissue
- E. Cervical lymphadenopathy
Pharyngeal clefts Explanation: **Second branchial cleft cyst**
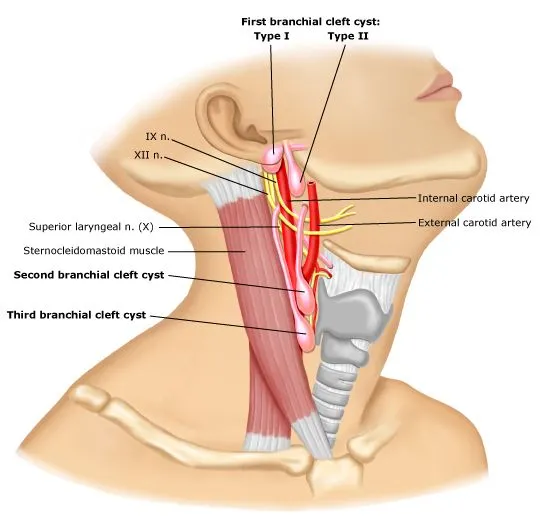
- The **location** (anteromedial to the sternocleidomastoid muscle), **painless** nature, and history of **gradual enlargement** becoming tender after an URI are classic presentations.
- **Imaging findings** (single, round cystic mass with uniform low echogenicity on ultrasound; homogeneous mass with low attenuation centrally and smooth rim enhancement on CT) are highly characteristic of an infected branchial cleft cyst.
*First branchial cleft cyst*
- Typically presents with a mass located near the **external auditory canal** or **angle of the mandible**, often causing otorrhea or recurrent infections.
- The presented mass is in a different anatomical location, **anteromedial** to the sternocleidomastoid.
*Sternomastoid tumor*
- This condition usually presents as a **fibrotic mass** within the sternocleidomastoid muscle in **neonates or infants**, associated with **congenital muscular torticollis**.
- The patient's age (20 years old) and the **cystic nature** of the mass make this diagnosis unlikely.
*Ectopic thyroid tissue*
- While possible in the neck, ectopic thyroid tissue would typically present as a **solid mass** and would show **iodine uptake** on nuclear imaging, not a cystic appearance on ultrasound and CT.
- It is more commonly located in the **midline** of the neck (e.g., lingual thyroid) rather than anteromedial to the sternocleidomastoid.
*Cervical lymphadenopathy*
- Enlarged lymph nodes typically present with **multiple, often tender, solid masses** or a single mass with typical lymph node morphology (e.g., hilar fat, oval shape), especially after an infection.
- The **cystic nature** described by imaging, with uniform low echogenicity and rim enhancement, is not typical for uncomplicated lymphadenopathy.
Pharyngeal clefts US Medical PG Question 2: A 4-year-old girl is brought by her mother to the pediatrician for neck drainage. The mother reports that the child has always had a small pinpoint opening on the front of her neck, though the opening has never been symptomatic. The child developed a minor cold approximately 10 days ago which resolved after a week. However, over the past 2 days, the mother has noticed clear thick drainage from the opening on the child’s neck. The child is otherwise healthy. She had an uncomplicated birth and is currently in the 45th and 40th percentiles for height and weight, respectively. On examination, there is a small opening along the skin at the anterior border of the right sternocleidomastoid at the junction of the middle and lower thirds of the neck. There is some slight clear thick discharge from the opening. Palpation around the opening elicits a cough from the child. This patient’s condition is caused by tissue that also forms which of the following?
- A. Epithelial tonsillar lining (Correct Answer)
- B. Thymus gland
- C. Epithelial lining of the Eustachian tube
- D. Superior parathyroid glands
- E. Inferior parathyroid glands
Pharyngeal clefts Explanation: ***Epithelial tonsillar lining***
- The clinical presentation of a **pinpoint opening with drainage along the anterior border of the sternocleidomastoid muscle**, especially with **cough elicited upon palpation**, is highly suggestive of a **second branchial cleft cyst/fistula**.
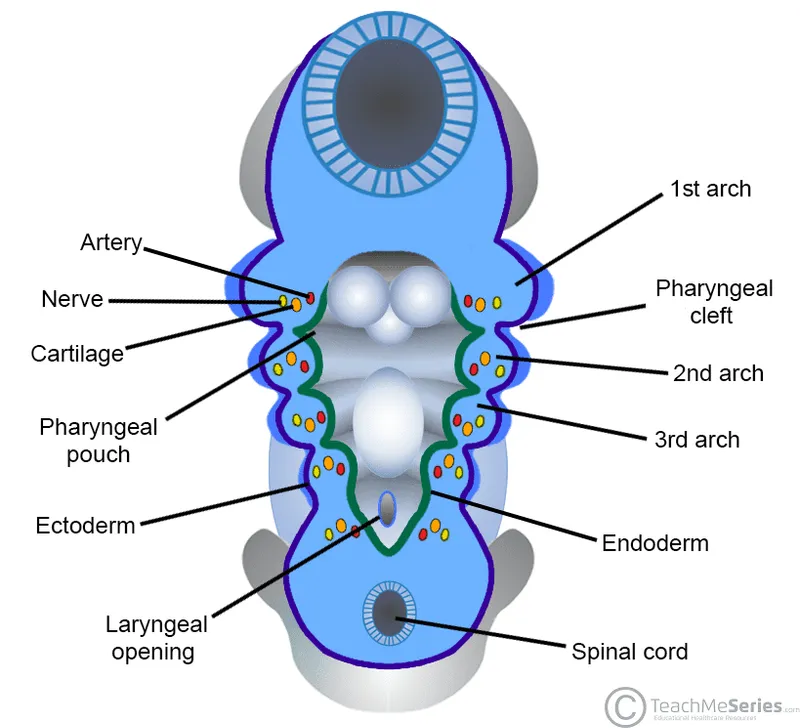
- This condition arises from incomplete obliteration of the **second branchial cleft**, which is part of the second pharyngeal arch complex.
- The **second pharyngeal pouch** (endodermal component of the second arch complex) forms the **epithelial lining of the palatine tonsils**.
- While the cleft (ectodermal) and pouch (endodermal) are technically distinct, they both derive from the second pharyngeal arch apparatus.
*Thymus gland*
- The **thymus gland** develops from the **third pharyngeal pouch**, not the second pharyngeal arch complex.
- Abnormalities of the thymus typically present as issues with immune function or mediastinal masses, not lateral neck drainage.
*Epithelial lining of the Eustachian tube*
- The **Eustachian tube** (auditory tube) develops from the **first pharyngeal pouch**.
- Manifestations related to the Eustachian tube typically involve middle ear issues, not drainage in the lateral neck.
*Superior parathyroid glands*
- The **superior parathyroid glands** develop from the **fourth pharyngeal pouch**.
- Dysgenesis of these glands leads to issues with calcium regulation (hypoparathyroidism), not neck fistulas.
*Inferior parathyroid glands*
- The **inferior parathyroid glands** develop from the **third pharyngeal pouch**, along with the thymus.
- Similar to the superior parathyroids, their abnormalities are related to calcium metabolism and would not present as a draining neck lesion.
Pharyngeal clefts US Medical PG Question 3: A 7-year-old boy is brought to the emergency department with a high fever and oxygen desaturation. He had a tracheostomy placed as an infant and has been placed on mechanical ventilation intermittently. Since then, he has had several bouts of pneumonia similar to his current presentation. In addition, he has been deaf since birth but is able to communicate through sign language. He attends school and performs above average for his grade. Physical exam reveals underdeveloped cheekbones, hypoplasia of the mandible, and malformed ears. Abnormal development of which of the following structures is most likely responsible for this patient's symptoms?
- A. Branchial cleft 1
- B. Branchial pouch 3
- C. Branchial arch 2
- D. Branchial arch 1 (Correct Answer)
- E. Branchial pouch 1
Pharyngeal clefts Explanation: ***Branchial arch 1***
- **Branchial arch 1** (mandibular arch) derivatives include the **mandible**, zygoma, part of the maxilla, incus, malleus, and facial muscles of mastication. Abnormal development leads to features like **underdeveloped cheekbones**, **mandibular hypoplasia**, and ear malformations, consistent with **Treacher Collins syndrome**.
- **Treacher Collins syndrome** is characterized by craniofacial anomalies resulting from improper development of structures derived from the **first and second pharyngeal arches**, specifically affecting the mandible, maxilla, zygoma, and ears. These malformations lead to airway difficulties requiring tracheostomy, chronic pneumonia due to aspiration, and conductive hearing loss.
*Branchial cleft 1*
- **Branchial cleft 1** anomalies typically present as **cysts** or **fistulas** in the periauricular or submandibular region, which are not described in this patient.
- While they can be associated with ear malformations, they do not typically cause the extensive **skeletal hypoplasia** of the face seen in this case.
*Branchial pouch 3*
- **Branchial pouch 3** develops into the **inferior parathyroid glands** and the **thymus**. Abnormalities here are associated with **DiGeorge syndrome**, characterized by hypocalcemia, T-cell immunodeficiency, and cardiac defects.
- These clinical features (hypocalcemia, immunodeficiency, heart defects) are distinct from the patient's presentation of craniofacial anomalies and recurrent respiratory issues related to airway compromise.
*Branchial arch 2*
- **Branchial arch 2** (hyoid arch) contributes to the development of the **stapes**, styloid process, lesser horn of the hyoid, and facial expression muscles. Dysfunction primarily leads to disorders like **facial nerve paralysis** or specific ear ossicle anomalies.
- While **Treacher Collins syndrome** also affects **branchial arch 2** derivatives, the primary skeletal and severe airway issues stem from the **first arch** involvement. The prominent features presented (mandibular and zygomatic hypoplasia) are more directly linked to the first arch.
*Branchial pouch 1*
- **Branchial pouch 1** gives rise to the **Eustachian tube** and the **middle ear cavity**. Abnormalities here can cause middle ear effusions or conductive hearing loss but do not explain the extensive craniofacial bony deformities and related airway issues.
- While the patient has deafness, the entire constellation of symptoms, including mandibular and zygomatic hypoplasia, points to structural development beyond just the middle ear.
Pharyngeal clefts US Medical PG Question 4: A 25-year-old man presents to the clinic with a midline swelling in his neck. He is unsure about when it appeared. He denies any difficulty with swallowing or hoarseness. His past medical history is insignificant. On physical examination, there is a 1 cm x 2 cm firm mildly tender nodule on the anterior midline aspect of the neck which moves with deglutition and elevates with protrusion of the tongue. Which of the following is the most likely embryologic origin of the nodule in this patient?
- A. Midline endoderm of the pharynx (Correct Answer)
- B. 1st and 2nd pharyngeal arch
- C. The branchial cleft
- D. 4th pharyngeal arch
- E. 4th pharyngeal pouch
Pharyngeal clefts Explanation: ***Midline endoderm of the pharynx***
- The symptoms described, particularly a midline neck swelling that **moves with deglutition** and **elevates with tongue protrusion**, are classic for a **thyroglossal duct cyst**.
- Thyroglossal duct cysts arise from remnants of the **thyroglossal duct**, an embryonic structure that forms from the **midline endoderm of the pharyngeal floor** and descends to form the thyroid gland.
*1st and 2nd pharyngeal arch*
- The 1st and 2nd pharyngeal arches primarily contribute to the formation of structures in the **mandible**, **maxilla**, **middle ear**, and **hyoid bone**.
- Abnormalities in these arches typically lead to conditions like **Treacher Collins syndrome** or **Pierre Robin sequence**, not midline neck cysts with these specific movement characteristics.
*The branchial cleft*
- **Branchial cleft cysts** typically present as **lateral neck masses**, often anterior to the sternocleidomastoid muscle, and usually do not move with deglutition or tongue protrusion.
- They arise from incomplete obliteration of **pharyngeal clefts**, which are ectodermal structures.
*4th pharyngeal arch*
- The 4th pharyngeal arch contributes to the formation of the **cricothyroid muscle**, part of the **pharynx**, and the **laryngeal cartilages**.
- Anomalies of the 4th pharyngeal arch are rare and typically involve **vascular structures** or **recurrent laryngeal nerve** abnormalities, not midline neck cysts.
*4th pharyngeal pouch*
- The 4th pharyngeal pouch contributes to the development of the **superior parathyroid glands** and the **ultimobranchial body** (which gives rise to parafollicular C cells of the thyroid).
- Malformations of this pouch are associated with parathyroid and thyroid conditions, not midline thyroglossal duct cysts.
Pharyngeal clefts US Medical PG Question 5: An investigator is studying the teratogenicity of cigarette smoking during pregnancy. He reviews several databases containing data about birth defects and prenatal drug exposures and finds that infants exposed to cigarette smoke in utero are approximately 2 times as likely to have a particular birth defect than unexposed infants. This defect results from abnormal development during the 6th week of gestation, when the maxillary prominences grow medially and fuse first with the lateral and then the medial nasal prominence. The defect is most likely which of the following?
- A. Cleft palate
- B. Macrognathia
- C. Torus palatinus
- D. Choanal atresia
- E. Cleft lip (Correct Answer)
Pharyngeal clefts Explanation: ***Cleft lip***
- **Cleft lip** results from the incomplete fusion of the **medial nasal prominence** and the **maxillary prominence**, which normally occurs around the 6th week of gestation.
- Exposure to **cigarette smoking** during pregnancy is a known **teratogen** that increases the risk of this developmental abnormality.
*Cleft palate*
- **Cleft palate** involves the incomplete fusion of the **palatal shelves**, occurring later in gestation (weeks 7-12), and is a separate developmental defect from cleft lip.
- While smoking can increase the risk of cleft palate, the described embryological event (fusion of maxillary and nasal prominences) specifically leads to **cleft lip**.
*Macrognathia*
- **Macrognathia** refers to an abnormally large jaw, which is a growth anomaly rather than a failure of fusion of facial prominences.
- This condition is not directly related to the developmental processes described in the question.
*Torus palatinus*
- **Torus palatinus** is a benign bony protuberance on the hard palate, often a genetically inherited trait, and is not a birth defect caused by failed embryonic fusion.
- It develops much later in life or can be present from birth but does not involve the specific embryonic structures mentioned.
*Choanal atresia*
- **Choanal atresia** is a blockage of the posterior nasal passage, caused by the failure of the **nasal cavity** to communicate with the **nasopharynx**.
- This defect is not related to the fusion of the maxillary and nasal prominences, which forms the upper lip and primary palate.
Pharyngeal clefts US Medical PG Question 6: A patient was admitted with skull base trauma. The doctor was testing the marked structure in the pharyngeal region. Which of the following nerves was being tested?
- A. Trigeminal nerve
- B. Facial nerve
- C. Glossopharyngeal nerve (Correct Answer)
- D. Vagus
- E. Hypoglossal nerve
Pharyngeal clefts Explanation: ***Glossopharyngeal nerve***
- The image shows a probe stimulating the posterior part of the **pharynx**, which elicits the **gag reflex**.
- The afferent limb of the **gag reflex** is mediated primarily by the **glossopharyngeal nerve (CN IX)**, which detects sensation from the posterior tongue and pharynx.
*Trigeminal nerve*
- The **trigeminal nerve (CN V)** primarily mediates sensation from the face, teeth, and anterior two-thirds of the tongue, and motor control of the **muscles of mastication**.
- It does not have a primary role in the sensation or reflex of the posterior pharyngeal wall.
*Facial nerve*
- The **facial nerve (CN VII)** is responsible for the **muscles of facial expression**, taste from the anterior two-thirds of the tongue, and parasympathetic innervation to several glands.
- While it contributes to some aspects of swallowing, it is not the main sensory nerve for the gag reflex from the posterior pharynx.
*Vagus*
- The **vagus nerve (CN X)** provides the efferent limb of the gag reflex, causing pharyngeal muscle contraction.
- However, the sensory input from the posterior pharynx (the afferent limb being tested by the probe) is primarily carried by the **glossopharyngeal nerve**.
*Hypoglossal nerve*
- The **hypoglossal nerve (CN XII)** provides motor innervation to the intrinsic and extrinsic muscles of the tongue.
- While it is relevant in skull base trauma, it does not mediate sensation from the pharynx or the gag reflex being tested in the image.
Pharyngeal clefts US Medical PG Question 7: A 78-year-old man comes to the physician because of a change in his voice. His wife says his voice has progressively become higher pitched, and he has had a 5.4-kg (11.9-lb) weight loss over the past 4 months. He has smoked half a pack of cigarettes daily for the past 40 years. Direct laryngoscopy shows an irregular, nodular glottic mass. A biopsy specimen of the mass shows poorly differentiated squamous cells with nuclear atypia, hyperkeratosis, and disruption of the basement membrane. Involvement of a muscle derived from which of the following branchial arches is the most likely cause of his symptoms?
- A. 1st arch
- B. 3rd arch
- C. 2nd arch
- D. 6th arch (Correct Answer)
- E. 4th arch
Pharyngeal clefts Explanation: ***6th arch***
- The patient's symptoms, including **hoarseness (change in voice)**, weight loss, and the biopsy findings of **squamous cell carcinoma of the glottis**, indicate a malignancy affecting the **larynx**.
- The intrinsic muscles of the larynx, responsible for vocal cord movement and voice production, are derived from the **6th pharyngeal arch**. Damage to these muscles or their innervation (recurrent laryngeal nerve, also derived from the 6th arch) by a tumor would cause vocal changes.
*1st arch*
- The first pharyngeal arch derivatives include the **muscles of mastication** (e.g., temporalis, masseter, medial and lateral pterygoids), and the **mylohyoid** and **anterior belly of digastric**.
- These muscles are primarily involved in jaw movement and chewing, and their involvement would not directly cause a high-pitched voice.
*3rd arch*
- The third pharyngeal arch derivatives include the **stylopharyngeus muscle**.
- This muscle is involved in swallowing and elevating the pharynx, and its dysfunction would not typically present as a change in voice pitch.
*2nd arch*
- The second pharyngeal arch derivatives include the **muscles of facial expression** (e.g., orbicularis oculi, orbicularis oris, platysma), **stapedius**, and the **posterior belly of the digastric**.
- These muscles are mainly involved in facial movements and hearing, and their pathology would not explain the patient's laryngeal symptoms.
*4th arch*
- The fourth pharyngeal arch derivatives include the **cricothyroid muscle** and other muscles of the soft palate and pharynx (e.g., levator veli palatini, superior/middle/inferior pharyngeal constrictors).
- While the cricothyroid muscle influences vocal cord tension and pitch, it is innervated by the **superior laryngeal nerve** (a derivative of the 4th arch), and a tumor in the glottis directly affecting the vocal cords (whose main adductors/abductors are 6th arch derivatives like the posterior cricoarytenoid and lateral cricoarytenoid muscles) makes the 6th arch the more encompassing answer for the symptom.
Pharyngeal clefts US Medical PG Question 8: A 64-year-old woman presents to an endocrinologist after her second time having a kidney stone in the last year. The patient reports no other symptoms except overall fatigue. On evaluation, the patient’s temperature is 98.4°F (36.9°C), blood pressure is 120/76 mmHg, pulse is 72/min, and respirations are 12/min. The patient has no neck masses and no tenderness to palpation in the abdomen. On laboratory workup, the endocrinologist finds that the patient has elevated parathyroid hormone levels and serum calcium. For surgical planning, the patient undergoes a sestamibi scan, which localizes disease to an area near the superior aspect of the thyroid in the right neck. Which of the following is the embryologic origin of this tissue?
- A. Fourth branchial arch
- B. Fourth branchial pouch (Correct Answer)
- C. Third branchial arch
- D. Dorsal wings of the third branchial pouch
- E. Ventral wings of the third branchial pouch
Pharyngeal clefts Explanation: ***Fourth branchial pouch***
- The superior parathyroid glands, generally located near the superior aspect of the thyroid, develop from the **fourth branchial pouch (dorsal wing)**.
- The **ultimobranchial body (C-cells)** also originates from the fourth branchial pouch.
*Fourth branchial arch*
- The fourth branchial arch forms structures like the **cricothyroid muscle**, pharyngeal constrictors, and laryngeal cartilages.
- It does not give rise to the parathyroid glands.
*Third branchial arch*
- The third branchial arch forms structures including the **stylopharyngeus muscle**, greater horn of the hyoid, and parts of the pharynx.
- It does not contribute to the formation of the parathyroid glands.
*Dorsal wings of the third branchial pouch*
- The **dorsal wings of the third branchial pouch** give rise to the inferior parathyroid glands.
- In this case, the diseased tissue was localized to the superior aspect nearest the superior parathyroid glands, not the inferior glands.
*Ventral wings of the third branchial pouch*
- The **ventral wings of the third branchial pouch** give rise to the thymus.
- This structure is not involved in parathyroid gland development.
More Pharyngeal clefts US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.