Neural crest contribution to pharyngeal arches US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neural crest contribution to pharyngeal arches. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neural crest contribution to pharyngeal arches US Medical PG Question 1: A 7-year-old boy is brought to the emergency department with a high fever and oxygen desaturation. He had a tracheostomy placed as an infant and has been placed on mechanical ventilation intermittently. Since then, he has had several bouts of pneumonia similar to his current presentation. In addition, he has been deaf since birth but is able to communicate through sign language. He attends school and performs above average for his grade. Physical exam reveals underdeveloped cheekbones, hypoplasia of the mandible, and malformed ears. Abnormal development of which of the following structures is most likely responsible for this patient's symptoms?
- A. Branchial cleft 1
- B. Branchial pouch 3
- C. Branchial arch 2
- D. Branchial arch 1 (Correct Answer)
- E. Branchial pouch 1
Neural crest contribution to pharyngeal arches Explanation: ***Branchial arch 1***
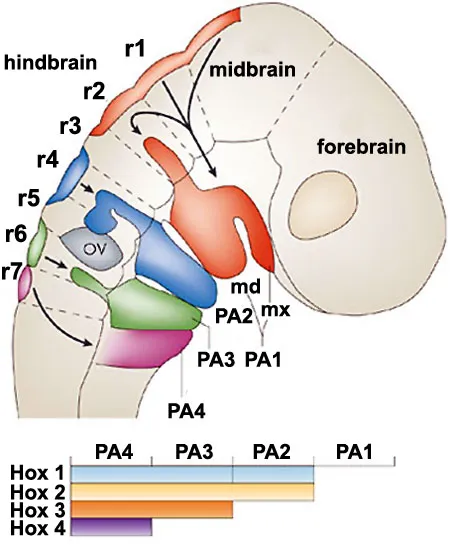
- **Branchial arch 1** (mandibular arch) derivatives include the **mandible**, zygoma, part of the maxilla, incus, malleus, and facial muscles of mastication. Abnormal development leads to features like **underdeveloped cheekbones**, **mandibular hypoplasia**, and ear malformations, consistent with **Treacher Collins syndrome**.
- **Treacher Collins syndrome** is characterized by craniofacial anomalies resulting from improper development of structures derived from the **first and second pharyngeal arches**, specifically affecting the mandible, maxilla, zygoma, and ears. These malformations lead to airway difficulties requiring tracheostomy, chronic pneumonia due to aspiration, and conductive hearing loss.
*Branchial cleft 1*
- **Branchial cleft 1** anomalies typically present as **cysts** or **fistulas** in the periauricular or submandibular region, which are not described in this patient.
- While they can be associated with ear malformations, they do not typically cause the extensive **skeletal hypoplasia** of the face seen in this case.
*Branchial pouch 3*
- **Branchial pouch 3** develops into the **inferior parathyroid glands** and the **thymus**. Abnormalities here are associated with **DiGeorge syndrome**, characterized by hypocalcemia, T-cell immunodeficiency, and cardiac defects.
- These clinical features (hypocalcemia, immunodeficiency, heart defects) are distinct from the patient's presentation of craniofacial anomalies and recurrent respiratory issues related to airway compromise.
*Branchial arch 2*
- **Branchial arch 2** (hyoid arch) contributes to the development of the **stapes**, styloid process, lesser horn of the hyoid, and facial expression muscles. Dysfunction primarily leads to disorders like **facial nerve paralysis** or specific ear ossicle anomalies.
- While **Treacher Collins syndrome** also affects **branchial arch 2** derivatives, the primary skeletal and severe airway issues stem from the **first arch** involvement. The prominent features presented (mandibular and zygomatic hypoplasia) are more directly linked to the first arch.
*Branchial pouch 1*
- **Branchial pouch 1** gives rise to the **Eustachian tube** and the **middle ear cavity**. Abnormalities here can cause middle ear effusions or conductive hearing loss but do not explain the extensive craniofacial bony deformities and related airway issues.
- While the patient has deafness, the entire constellation of symptoms, including mandibular and zygomatic hypoplasia, points to structural development beyond just the middle ear.
Neural crest contribution to pharyngeal arches US Medical PG Question 2: A 10-year-old boy comes for a post-operative clinic visit with his ENT surgeon three months after airway reconstruction surgery and placement of a tracheostomy tube. Since the surgery, he says that he has been able to breathe better and is now getting used to tracheostomy care and tracheostomy tube changes. In addition to this surgery, he has had over twenty surgeries to implant hearing aids, reconstruct his cheekbones, and support his jaw to enable him to swallow. He was born with these abnormalities and had difficult breathing, hearing, and eating throughout his childhood. Fortunately, he is now beginning to feel better and is able to attend public school where he is one of the best students in the class. Abnormal development of which of the following structures is most likely responsible for this patient's malformations?
- A. Second branchial cleft
- B. First branchial pouch
- C. Third and fourth branchial pouches
- D. First branchial arch (Correct Answer)
- E. Second branchial arch
Neural crest contribution to pharyngeal arches Explanation: ***First branchial arch***
- The clinical presentation describes features consistent with **Treacher Collins syndrome** (TCS), also known as mandibulofacial dysostosis, which results from maldevelopment of **both the first and second branchial arches**.
- However, the **predominant and most characteristic features** arise from **first branchial arch** abnormalities: **mandibular hypoplasia** (requiring jaw support for swallowing), **malar/zygomatic hypoplasia** (reconstructed cheekbones), and **maxillary hypoplasia**.
- These first arch skeletal abnormalities cause the **airway obstruction** (requiring tracheostomy) and feeding difficulties.
- The first branchial arch gives rise to: **mandible, maxilla, zygomatic bone, incus, malleus, muscles of mastication, and CN V** (trigeminal nerve).
- While hearing issues may involve second arch structures (stapes), the **overwhelming majority** of this patient's clinical problems stem from first arch malformations.
*Second branchial cleft*
- The second branchial cleft typically forms the **cervical sinus**, which normally obliterates. Persistence can lead to **cervical cysts or fistulas**, presenting as neck masses.
- Abnormalities of the second branchial cleft do not explain the extensive craniofacial malformations, hearing deficits, or airway compromise seen in this patient.
*First branchial pouch*
- The first branchial pouch gives rise to the **auditory (eustachian) tube** and the **tympanic cavity** (middle ear).
- While isolated first pouch defects could contribute to hearing problems, they would **not explain** the severe facial bone malformations (mandibular and malar hypoplasia), airway obstruction, or feeding difficulties.
- The pouch is distinct from the arch, which forms the skeletal and muscular structures.
*Third and fourth branchial pouches*
- The third branchial pouch contributes to the **inferior parathyroid glands** and the **thymus**. The fourth branchial pouch contributes to the **superior parathyroid glands** and the **ultimobranchial body** (parafollicular C cells of the thyroid).
- Abnormalities in these pouches, such as in **DiGeorge syndrome (22q11.2 deletion)**, lead to **T-cell immunodeficiency, hypocalcemia, and cardiac defects** but do not account for the craniofacial and hearing abnormalities described.
*Second branchial arch*
- The second branchial arch gives rise to the **stapes**, **styloid process**, **lesser horn and upper body of hyoid bone**, **stapedius muscle**, and **CN VII** (facial nerve).
- While Treacher Collins syndrome involves both first and second arch abnormalities, the **second arch contributions** are less prominent clinically.
- Second arch defects could contribute to **conductive hearing loss** (via stapes abnormalities) and **facial nerve issues**, but these are not the predominant features in this case.
- The critical skeletal malformations causing airway compromise, feeding difficulties, and facial dysmorphism are primarily **first arch** derivatives.
Neural crest contribution to pharyngeal arches US Medical PG Question 3: A syndrome caused by chromosomal anomalies is being researched in the immunology laboratory. Several congenital conditions are observed among the participating patients, mostly involving the thymus and the heart. Common facial features of affected individuals are shown in the image below. Flow cytometry analysis of patient samples reveals a CD19+ and CD3- result. What kind of congenital anomaly is generally observed in these patients, specifically in the thymus?
- A. Deformation
- B. Malformation
- C. Disruption
- D. Aplasia (Correct Answer)
- E. Agenesis
Neural crest contribution to pharyngeal arches Explanation: ***Aplasia***
- The scenario describes **DiGeorge syndrome**, characterized by a **22q11.2 deletion**, leading to defective development of the 3rd and 4th pharyngeal pouches.
- This results in **thymic hypoplasia or aplasia**, causing **T-cell immunodeficiency** (CD3-), and **parathyroid aplasia**, leading to hypocalcemia.
- The CD19+ (B cells present) and CD3- (T cells absent) flow cytometry result specifically points to **thymic aplasia** as the cause for the lack of mature T-cells.
*Deformation*
- A deformation refers to an **abnormality in shape or position of a normally formed body part** due to extrinsic mechanical forces, such as uterine constraint.
- This is not the primary mechanism behind the thymic and cardiac anomalies described, which are due to inherent developmental defects.
*Malformation*
- A malformation is an **intrinsic abnormality of development** occurring during the embryonic period, due to genetic or environmental factors.
- While DiGeorge syndrome involves malformations (e.g., cardiac defects, characteristic facial features), the specific term for the complete or near-complete absence of an organ like the thymus is aplasia or hypoplasia, which is a more precise description in this context.
*Disruption*
- A disruption is a **morphological defect of an organ or body part from extrinsic breakdown of, or an interference with, an originally normal developmental process**.
- Examples include **amniotic bands** causing limb defects; this does not fit the description of a primary developmental defect of the pharyngeal pouches.
*Agenesis*
- Agenesis refers to the **complete absence of an organ** due to failure of development during embryonic growth.
- While agenesis is severe, **aplasia** (failure of development resulting in a rudimentary structure or complete absence) is often used interchangeably or to describe a more specific severe lack of development, especially in conditions like DiGeorge syndrome where there can be hypoplasia or complete absence. In clinical practice for DiGeorge, aplasia or hypoplasia is more commonly used for the thymus.
Neural crest contribution to pharyngeal arches US Medical PG Question 4: A 23-year-old man comes to the physician for evaluation of decreased hearing, dizziness, and ringing in his right ear for the past 6 months. Physical examination shows multiple soft, yellow plaques and papules on his arms, chest, and back. There is sensorineural hearing loss and weakness of facial muscles bilaterally. His gait is unsteady. An MRI of the brain shows a 3-cm mass near the right internal auditory meatus and a 2-cm mass at the left cerebellopontine angle. The abnormal cells in these masses are most likely derived from which of the following embryological structures?
- A. Surface ectoderm
- B. Neural tube
- C. Neural crest (Correct Answer)
- D. Notochord
- E. Mesoderm
Neural crest contribution to pharyngeal arches Explanation: ***Neural crest***
- The patient's symptoms (bilateral sensorineural hearing loss, facial weakness, unsteady gait, central masses) along with cutaneous lesions (soft, yellow plaques) are highly suggestive of **Neurofibromatosis type 2 (NF2)**.
- NF2 is characterized by **vestibular schwannomas** (acoustic neuromas) and other CNS tumors, which are derived from **Schwann cells**. Schwann cells, along with melanocytes and other peripheral nervous system components, originate from the **neural crest**.
*Surface ectoderm*
- The surface ectoderm forms structures such as the **epidermis**, hair, nails, and anterior pituitary.
- While the skin lesions are present, the primary tumors (schwannomas) are not derived from the surface ectoderm.
*Neural tube*
- The neural tube gives rise to the **central nervous system** (brain and spinal cord) and motor neurons.
- While the tumors affect the brain and cranial nerves, the specific cell type forming schwannomas (Schwann cells) does not originate directly from the neural tube.
*Notochord*
- The notochord induces the formation of the neural tube and eventually degenerates, contributing to the **nucleus pulposus** of the intervertebral discs.
- It is not involved in the pathogenesis or cellular origin of schwannomas.
*Mesoderm*
- The mesoderm gives rise to connective tissues, blood, bone, muscle, and most internal organs.
- While some tumors can have mesodermal origins, schwannomas are neuroectodermal in origin.
Neural crest contribution to pharyngeal arches US Medical PG Question 5: A 25-year-old man presents to the clinic with a midline swelling in his neck. He is unsure about when it appeared. He denies any difficulty with swallowing or hoarseness. His past medical history is insignificant. On physical examination, there is a 1 cm x 2 cm firm mildly tender nodule on the anterior midline aspect of the neck which moves with deglutition and elevates with protrusion of the tongue. Which of the following is the most likely embryologic origin of the nodule in this patient?
- A. Midline endoderm of the pharynx (Correct Answer)
- B. 1st and 2nd pharyngeal arch
- C. The branchial cleft
- D. 4th pharyngeal arch
- E. 4th pharyngeal pouch
Neural crest contribution to pharyngeal arches Explanation: ***Midline endoderm of the pharynx***
- The symptoms described, particularly a midline neck swelling that **moves with deglutition** and **elevates with tongue protrusion**, are classic for a **thyroglossal duct cyst**.
- Thyroglossal duct cysts arise from remnants of the **thyroglossal duct**, an embryonic structure that forms from the **midline endoderm of the pharyngeal floor** and descends to form the thyroid gland.
*1st and 2nd pharyngeal arch*
- The 1st and 2nd pharyngeal arches primarily contribute to the formation of structures in the **mandible**, **maxilla**, **middle ear**, and **hyoid bone**.
- Abnormalities in these arches typically lead to conditions like **Treacher Collins syndrome** or **Pierre Robin sequence**, not midline neck cysts with these specific movement characteristics.
*The branchial cleft*
- **Branchial cleft cysts** typically present as **lateral neck masses**, often anterior to the sternocleidomastoid muscle, and usually do not move with deglutition or tongue protrusion.
- They arise from incomplete obliteration of **pharyngeal clefts**, which are ectodermal structures.
*4th pharyngeal arch*
- The 4th pharyngeal arch contributes to the formation of the **cricothyroid muscle**, part of the **pharynx**, and the **laryngeal cartilages**.
- Anomalies of the 4th pharyngeal arch are rare and typically involve **vascular structures** or **recurrent laryngeal nerve** abnormalities, not midline neck cysts.
*4th pharyngeal pouch*
- The 4th pharyngeal pouch contributes to the development of the **superior parathyroid glands** and the **ultimobranchial body** (which gives rise to parafollicular C cells of the thyroid).
- Malformations of this pouch are associated with parathyroid and thyroid conditions, not midline thyroglossal duct cysts.
Neural crest contribution to pharyngeal arches US Medical PG Question 6: A 35-year-old man comes to the physician for evaluation of a neck mass and hoarseness. He has no history of major medical illness. Physical examination shows a 2.5-cm fixed, irregular thyroid nodule. His serum calcitonin concentration is elevated. The nodule is most likely comprised of cells that are embryologically derived from which of the following structures?
- A. Second branchial pouch
- B. Fourth branchial arch
- C. Surface ectoderm
- D. Third branchial pouch
- E. Neural crest cells (Correct Answer)
Neural crest contribution to pharyngeal arches Explanation: ***Neural crest cells***
- The elevated **serum calcitonin** in the presence of a thyroid nodule is highly suggestive of **medullary thyroid carcinoma (MTC)**.
- **MTC** originates from the **parafollicular C cells** of the thyroid, which are embryologically derived from **neural crest cells** that migrate to the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) during development and subsequently integrate into the thyroid gland.
- This is the definitive embryological origin of calcitonin-producing C cells.
*Second branchial pouch*
- The second branchial pouch typically gives rise to the **palatine tonsil crypts** and **tonsillar fossa**.
- It is not associated with the development of the **parafollicular C cells** or thyroid malignancies.
*Fourth branchial arch*
- The fourth branchial arch gives rise to the **superior laryngeal nerve** and associated laryngeal cartilages.
- While the **ultimobranchial body** (from the 4th/5th pharyngeal pouch) does contribute C cells to the thyroid, these cells themselves are derived from **neural crest cells** that migrate to this structure, not from the pouch itself.
- Therefore, the embryological origin is neural crest, not the branchial arch/pouch.
*Surface ectoderm*
- Surface ectoderm forms structures such as the **epidermis of the skin**, **hair**, **nails**, and **lens of the eye**.
- It does not contribute to the development of the **C cells** or the thyroid gland.
*Third branchial pouch*
- The third branchial pouch gives rise to the **inferior parathyroid glands** and the majority of the **thymus**.
- While it contributes to endocrine tissues, it does not form the **parafollicular C cells** of the thyroid.
Neural crest contribution to pharyngeal arches US Medical PG Question 7: A 59-year-old man comes to the physician for evaluation of a progressively enlarging, 8-mm skin lesion on the right shoulder that developed 1 month ago. The patient has a light-skinned complexion and has had several dysplastic nevi removed in the past. A photograph of the lesion is shown. The lesion is most likely derived from cells that are also the embryological origin of which of the following tumors?
- A. Adrenal adenoma
- B. Liposarcoma
- C. Basal cell carcinoma
- D. Neuroblastoma (Correct Answer)
- E. Medullary thyroid cancer
Neural crest contribution to pharyngeal arches Explanation: ***Neuroblastoma***
- The skin lesion described, with history of dysplastic nevi and progressive growth, is highly suggestive of **melanoma**. Melanoma arises from **melanocytes**, which are derived from the **neural crest**.
- **Neuroblastoma** is a tumor of the **sympathetic nervous system** that also originates from **neural crest cells**, making it the correct embryological match.
- Neuroblastoma is the **classic example** of a neural crest-derived tumor taught alongside melanoma in medical education.
*Adrenal adenoma*
- **Adrenal adenomas** are benign tumors of the adrenal cortex, which is derived from the **mesoderm**.
- This embryological origin is distinct from the neural crest origin of melanocytes.
*Liposarcoma*
- **Liposarcomas** are malignant tumors of adipose tissue, which arises from the **mesoderm**.
- This origin does not match the neural crest origin of melanocytes.
*Basal cell carcinoma*
- **Basal cell carcinoma** originates from the **basal layer of the epidermis**, which is derived from **surface ectoderm** (not neural crest).
- While it's an ectodermal derivative, it does not share the neural crest origin of melanocytes.
*Medullary thyroid cancer*
- **Medullary thyroid cancer** originates from the **parafollicular C cells** of the thyroid gland, which are also derived from the **neural crest**.
- While this shares the same embryological origin as melanoma, **neuroblastoma** is the more commonly tested and classic pairing with melanoma in standard medical examinations when discussing neural crest-derived tumors.
Neural crest contribution to pharyngeal arches US Medical PG Question 8: A 52-year-old woman sees you in your office with a complaint of new-onset headaches over the past few weeks. On exam, you find a 2 x 2 cm dark, irregularly shaped, pigmented lesion on her back. She is concerned because her father recently passed away from skin cancer. What tissue type most directly gives rise to the lesion this patient is experiencing?
- A. Neural crest cells (Correct Answer)
- B. Endoderm
- C. Mesoderm
- D. Ectoderm
- E. Neuroectoderm
Neural crest contribution to pharyngeal arches Explanation: ***Neural crest cells***
- The suspected lesion, given its description and the patient's family history of skin cancer, is likely a **melanoma**.
- Melanoma originates from **melanocytes**, which are derived from **neural crest cells** during embryonic development.
*Endoderm*
- The endoderm gives rise to the **lining of the gastrointestinal and respiratory tracts**, as well as organs such as the liver and pancreas.
- It is not involved in the formation of melanocytes or skin lesions like melanoma.
*Mesoderm*
- The mesoderm forms tissues such as **muscle, bone, cartilage, connective tissue**, and the circulatory system.
- It does not directly give rise to melanocytes, which are the cells of origin for melanoma.
*Ectoderm*
- The ectoderm gives rise to the **epidermis, nervous system**, and sensory organs.
- While melanocytes are found in the epidermis, they are specifically derived from the **neural crest (a sub-population of ectoderm)**, not the general ectoderm.
*Neuroectoderm*
- Neuroectoderm specifically refers to the ectoderm that develops into the **nervous system**.
- While neural crest cells originate from the neuroectoderm, "neural crest cells" is a more precise answer for the origin of melanocytes.
Neural crest contribution to pharyngeal arches US Medical PG Question 9: A 78-year-old man comes to the physician because of a change in his voice. His wife says his voice has progressively become higher pitched, and he has had a 5.4-kg (11.9-lb) weight loss over the past 4 months. He has smoked half a pack of cigarettes daily for the past 40 years. Direct laryngoscopy shows an irregular, nodular glottic mass. A biopsy specimen of the mass shows poorly differentiated squamous cells with nuclear atypia, hyperkeratosis, and disruption of the basement membrane. Involvement of a muscle derived from which of the following branchial arches is the most likely cause of his symptoms?
- A. 1st arch
- B. 3rd arch
- C. 2nd arch
- D. 6th arch (Correct Answer)
- E. 4th arch
Neural crest contribution to pharyngeal arches Explanation: ***6th arch***
- The patient's symptoms, including **hoarseness (change in voice)**, weight loss, and the biopsy findings of **squamous cell carcinoma of the glottis**, indicate a malignancy affecting the **larynx**.
- The intrinsic muscles of the larynx, responsible for vocal cord movement and voice production, are derived from the **6th pharyngeal arch**. Damage to these muscles or their innervation (recurrent laryngeal nerve, also derived from the 6th arch) by a tumor would cause vocal changes.
*1st arch*
- The first pharyngeal arch derivatives include the **muscles of mastication** (e.g., temporalis, masseter, medial and lateral pterygoids), and the **mylohyoid** and **anterior belly of digastric**.
- These muscles are primarily involved in jaw movement and chewing, and their involvement would not directly cause a high-pitched voice.
*3rd arch*
- The third pharyngeal arch derivatives include the **stylopharyngeus muscle**.
- This muscle is involved in swallowing and elevating the pharynx, and its dysfunction would not typically present as a change in voice pitch.
*2nd arch*
- The second pharyngeal arch derivatives include the **muscles of facial expression** (e.g., orbicularis oculi, orbicularis oris, platysma), **stapedius**, and the **posterior belly of the digastric**.
- These muscles are mainly involved in facial movements and hearing, and their pathology would not explain the patient's laryngeal symptoms.
*4th arch*
- The fourth pharyngeal arch derivatives include the **cricothyroid muscle** and other muscles of the soft palate and pharynx (e.g., levator veli palatini, superior/middle/inferior pharyngeal constrictors).
- While the cricothyroid muscle influences vocal cord tension and pitch, it is innervated by the **superior laryngeal nerve** (a derivative of the 4th arch), and a tumor in the glottis directly affecting the vocal cords (whose main adductors/abductors are 6th arch derivatives like the posterior cricoarytenoid and lateral cricoarytenoid muscles) makes the 6th arch the more encompassing answer for the symptom.
Neural crest contribution to pharyngeal arches US Medical PG Question 10: A 29-year-old mother brings in her 2-week-old baby boy to a pediatrician because he has been having difficulty feeding. The mother reveals that she had no prenatal care during her pregnancy and gave birth at home without complications. She says that her son seems to be having difficulty sucking, and she occasionally sees breast milk coming out of the infant’s nose. Physical exam reveals that this patient has a gap between his oral and nasal cavities behind the incisive foramen. He is therefore prescribed specialized bottles and his mom is taught positional techniques to ensure better feeding. Failure to fuse which of the following structures is most likely responsible for this patient's disorder?
- A. Maxillary and medial nasal prominences
- B. Nasal septum with primary plates
- C. Maxillary and lateral nasal prominences
- D. Palatine shelves with primary plates
- E. Palatine shelves with nasal septum (Correct Answer)
Neural crest contribution to pharyngeal arches Explanation: ***Palatine shelves with nasal septum***
- A **cleft palate** results from the **failure of fusion of the palatine shelves** with each other and/or with the **nasal septum**, creating an abnormal communication between the oral and nasal cavities.
- This anatomical defect explains the infant's **feeding difficulties** and the leakage of breast milk into the nose, as well as the observed **gap behind the incisive foramen**.
*Maxillary and medial nasal prominences*
- The failure of fusion between the maxillary and medial nasal prominences results in a **cleft lip**, which is an anterior defect and does not explain the posterior gap described.
- While cleft lip can coexist with cleft palate, the symptoms here specifically point to a palatal defect, not primarily a lip defect.
*Nasal septum with primary plates*
- The primary palate forms from the fusion of the medial nasal prominences, anterior to the incisive foramen.
- While crucial for normal development, the specific clinical presentation (gap *behind* the incisive foramen and feeding difficulties) is more characteristic of a secondary palate defect involving the palatine shelves.
*Maxillary and lateral nasal prominences*
- The fusion of these structures contributes to the formation of the **nasolacrimal groove** and parts of the cheek, not the palate.
- Deficiencies in this fusion would lead to defects in the lateral facial region, not an oro-nasal communication related to feeding.
*Palatine shelves with primary plates*
- The **primary palate** fuses with the anterior part of the secondary palate (formed by the palatine shelves) at the incisive foramen.
- However, the more common and clinically relevant defect leading to an open communication between the oral and nasal cavities, especially *behind* the incisive foramen, involves the failure of fusion of the **palatine shelves** with each other and the **nasal septum**.
More Neural crest contribution to pharyngeal arches US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.