Fourth and sixth pharyngeal arch derivatives US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Fourth and sixth pharyngeal arch derivatives. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 1: An otherwise healthy 58-year-old man comes to the physician because of a 1-year history of episodic coughing whenever he cleans his left ear. There is no history of hearing loss, tinnitus, or vertigo. Stimulating his left ear canal with a cotton swab triggers a bout of coughing. The physician informs him that these symptoms are caused by hypersensitivity of a cranial nerve. A peripheral lesion of this nerve is most likely to manifest with which of the following findings on physical examination?
- A. Ipsilateral sensorineural hearing loss
- B. Ipsilateral deviation of the tongue
- C. Inability to raise ipsilateral eyebrow
- D. Decreased secretion from ipsilateral sublingual gland
- E. Ipsilateral vocal cord palsy (Correct Answer)
Fourth and sixth pharyngeal arch derivatives Explanation: ***Ipsilateral vocal cord palsy***
- The sensation in the external auditory canal that triggers a cough reflex is mediated by the **auricular branch of the vagus nerve (CN X)**, also known as Arnold's nerve.
- A peripheral lesion of the vagus nerve would most likely affect its motor functions, including the innervation of the **larynx**, leading to **ipsilateral vocal cord palsy** and hoarseness.
*Ipsilateral sensorineural hearing loss*
- Hearing loss is primarily associated with pathology of the **vestibulocochlear nerve (CN VIII)**, not the vagus nerve.
- The patient's presentation does not describe any auditory symptoms.
*Ipsilateral deviation of the tongue*
- Tongue deviation is a sign of compromise of the **hypoglossal nerve (CN XII)**, which controls the intrinsic and extrinsic muscles of the tongue.
- This is not a function of the vagus nerve.
*Inability to raise ipsilateral eyebrow*
- The ability to raise the eyebrow is controlled by the **facial nerve (CN VII)**, which innervates the muscles of facial expression.
- Vagus nerve lesions do not typically present with facial weakness.
*Decreased secretion from ipsilateral sublingual gland*
- Secretion from the sublingual gland is controlled by the **facial nerve (CN VII)** via the submandibular ganglion.
- While the vagus nerve has autonomic functions, it does not directly control sublingual gland secretion.
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 2: A 45-year-old male patient presents with difficulty swallowing and hoarseness that has progressively worsened over the past month. During physical examination, the physician notices that the patient's left vocal cord is paralyzed. The paralysis is most likely due to compression of which of the following nerves?
- A. Left superior laryngeal nerve
- B. Left vagus nerve
- C. Right recurrent laryngeal nerve
- D. Left recurrent laryngeal nerve (Correct Answer)
Fourth and sixth pharyngeal arch derivatives Explanation: ***Left recurrent laryngeal nerve***
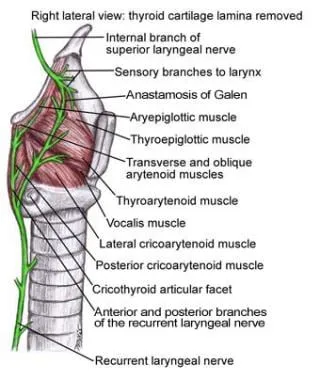
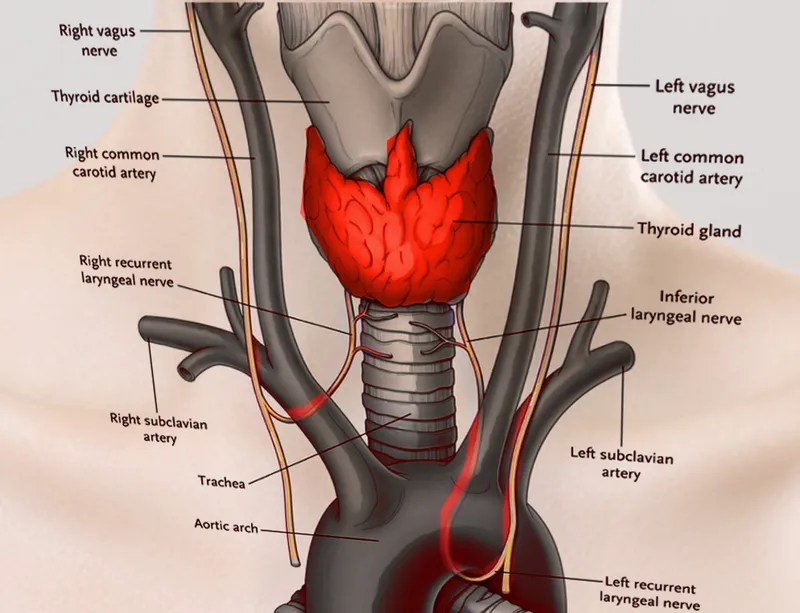
- The **left recurrent laryngeal nerve** innervates all intrinsic muscles of the left larynx, except the cricothyroid muscle [1].
- Damage or compression of this nerve leads to **left vocal cord paralysis** and associated symptoms like hoarseness and difficulty swallowing (dysphagia).
*Left superior laryngeal nerve*
- The **superior laryngeal nerve** innervates the cricothyroid muscle, which is responsible for tensing the vocal cords.
- Damage to this nerve primarily affects **pitch control** and would not typically cause complete vocal cord paralysis.
*Left vagus nerve*
- The **vagus nerve** gives rise to both the superior and recurrent laryngeal nerves [1].
- While damage to the main vagus nerve would cause vocal cord paralysis, the more specific finding of isolated vocal cord paralysis points to an issue with its branch, the recurrent laryngeal nerve [1].
*Right recurrent laryngeal nerve*
- The **right recurrent laryngeal nerve** controls the intrinsic muscles of the right larynx.
- Damage to this nerve would result in **right vocal cord paralysis**, not left vocal cord paralysis as described in the patient.
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 3: A 50-year-old man is brought in by ambulance to the emergency department with difficulty breathing and speaking. His wife reports that he might have swallowed a fishbone. While taking his history the patient develops a paroxysmal cough. Visualization of his oropharynx and larynx shows a fishbone lodged in the right piriform recess. After successfully removing the fishbone the patient feels comfortable, but he is not able to cough like before. Damage to which of the following nerves is responsible for the impaired cough reflex in this patient?
- A. Inferior laryngeal nerve
- B. Internal laryngeal nerve (Correct Answer)
- C. External laryngeal nerve
- D. Superior laryngeal nerve
- E. Recurrent laryngeal nerve
Fourth and sixth pharyngeal arch derivatives Explanation: ***Internal laryngeal nerve***
- The internal laryngeal nerve is the **sensory nerve** of the larynx above the vocal cords, including the piriform recess. Damage to this nerve, often due to trauma from a foreign body like a fishbone, impairs the **afferent limb of the cough reflex**.
- A fishbone lodged in the **piriform recess** directly implicates the sensory function of the internal laryngeal nerve, explaining the subsequent loss of the cough reflex even after removal of the foreign body.
*Inferior laryngeal nerve*
- This nerve is primarily **motor** to almost all intrinsic laryngeal muscles and provides **sensory innervation** below the vocal folds. Damage would primarily affect phonation (hoarseness) or breathing due to vocal cord paralysis.
- It would not directly affect the sensory input initiating a cough reflex from the piriform recess, which is above the vocal folds.
*External laryngeal nerve*
- The external laryngeal nerve is a **motor nerve** supplying the **cricothyroid muscle**, which is responsible for tensing the vocal cords and altering voice pitch.
- Damage to this nerve would lead to **hoarseness** and difficulty with high-pitched sounds, not an impaired cough reflex from the piriform recess.
*Superior laryngeal nerve*
- The superior laryngeal nerve divides into the internal and external laryngeal nerves. While it contains sensory fibers that lead to the internal laryngeal nerve, stating damage to the entire superior laryngeal nerve is less specific than identifying the internal laryngeal nerve as the direct cause of the sensory deficit.
- Damage to the superior laryngeal nerve would encompass both sensory and motor deficits (internal and external branches), but the specific symptom of impaired cough reflex primarily points to the internal laryngeal branch.
*Recurrent laryngeal nerve*
- This nerve is another name for the **inferior laryngeal nerve** and is primarily **motor** to the intrinsic laryngeal muscles (except cricothyroid) and provides sensory innervation below the vocal cords.
- Damage to this nerve primarily results in **vocal cord paralysis** and voice changes (hoarseness), not the sensory loss affecting the cough reflex from the piriform recess.
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 4: A 68-year-old man comes to the physician because of a 6-month history of difficulty swallowing pieces of meat and choking frequently during meal times. He also sometimes regurgitates foul-smelling, undigested food particles. Examination shows a 3 x 3 cm soft cystic, immobile mass in the upper third of the left side of his neck anterior to the left sternocleidomastoid muscle that becomes prominent when he coughs. A barium swallow shows an accumulation of contrast on the lateral aspect of the neck at the C5 level. Which of the following is the most likely underlying cause for this patient's condition?
- A. Remnant of the embryological omphalomesenteric duct
- B. Inadequate relaxation of lower esophageal sphincter
- C. Remnant of the thyroglossal duct
- D. Increased intrapharyngeal pressure (Correct Answer)
- E. Remnant of the second branchial cleft
Fourth and sixth pharyngeal arch derivatives Explanation: ***Increased intrapharyngeal pressure***
- The symptoms of **dysphagia**, **regurgitation of undigested food**, and a **neck mass prominent with coughing** are classic for a **Zenker's diverticulum**, which results from increased intrapharyngeal pressure causing herniation of mucosa through Killian's triangle.
- The barium swallow showing **contrast accumulation** and the location of the mass further support this diagnosis, as Zenker's diverticula are pseudo-diverticula caused by pulsion from high pressure during swallowing.
*Remnant of the embryological omphalomesenteric duct*
- An **omphalomesenteric duct remnant** typically presents as a **Meckel's diverticulum** in the small intestine or an umbilical fistula, not as a neck mass with swallowing difficulties.
- This embryological anomaly is related to the midgut development and has no connection to pharyngeal issues.
*Inadequate relaxation of lower esophageal sphincter*
- **Inadequate relaxation of the lower esophageal sphincter** (LES) is characteristic of **achalasia**, which causes dysphagia and regurgitation, but typically of *fermented* rather than *undigested* food, and does not present with a palpable neck mass as described.
- Achalasia involves the distal esophagus and does not lead to a pharyngeal outpouching.
*Remnant of the thyroglossal duct*
- A **thyroglossal duct cyst** is a midline neck mass that moves with swallowing and tongue protrusion, which is not consistent with the lateral, pulsion-type mass that becomes prominent with coughing.
- While it can be found in the upper third of the neck, its embryological origin and presentation differ significantly from a Zenker's diverticulum.
*Remnant of the second branchial cleft*
- A **second branchial cleft cyst** is typically a lateral neck mass, often located anterior to the sternocleidomastoid muscle, but it is congenital and does not typically present with progressive dysphagia and regurgitation of undigested food in adulthood, nor does it typically become prominent with coughing due to increased intrapharyngeal pressure.
- These cysts are usually asymptomatic unless infected and are not directly related to swallowing mechanics.
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 5: A patient undergoes an MRI of the brain that reveals a tumor compressing the facial nerve at the internal acoustic meatus. Which of the following symptoms would most likely be present?
- A. Loss of taste in the posterior third of the tongue
- B. Loss of taste in the anterior two-thirds of the tongue
- C. Decreased salivation
- D. Facial muscle weakness and hyperacusis (Correct Answer)
- E. Decreased lacrimation
Fourth and sixth pharyngeal arch derivatives Explanation: ***Facial muscle weakness and hyperacusis***
- Compression of the **facial nerve (CN VII)** before it branches within the facial canal affects both its motor and special visceral afferent functions. [1]
- **Facial muscle weakness** results from damage to the motor fibers, while **hyperacusis** occurs due to paralysis of the stapedius muscle, innervated by the facial nerve's branch to the stapedius. [1]
*Loss of taste in the posterior third of the tongue*
- **Taste sensation** from the posterior third of the tongue is conveyed by the **glossopharyngeal nerve (CN IX)**, not the facial nerve.
- Therefore, compression of the facial nerve at the internal acoustic meatus would not impact taste in this region.
*Loss of taste in the anterior two-thirds of the tongue*
- While the **chorda tympani nerve** (a branch of the facial nerve) carries taste from the anterior two-thirds of the tongue, this branch typically separates from the facial nerve **distal to the internal acoustic meatus**.
- Compression at the internal acoustic meatus would affect the main trunk before this branching, but other symptoms are more prominent. [1]
*Decreased salivation*
- **Salivation** (specifically from the submandibular and sublingual glands) is mediated by the **chorda tympani nerve**, a branch of the facial nerve. [1]
- Similar to taste, this branch usually separates later, and while salivation can be affected, other symptoms like facial weakness and hyperacusis are more consistently prominent with proximal compression.
*Decreased lacrimation*
- **Lacrimation** is primarily controlled by the **greater petrosal nerve**, which branches off the facial nerve earlier in its course.
- While theoretically possible with very proximal compression affecting all components, compression at the internal acoustic meatus is more commonly associated with the motor and stapedius muscle function impairments first due to the spatial arrangement of fibers.
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 6: A 72-year-old man comes to the physician for a 5-month history of hoarseness, exertional dyspnea, and fatigue. He does not smoke or drink alcohol. His pulse is 98/min and irregular. His voice is coarse in quality. Physical examination shows a liver span of 16 cm and a soft diastolic murmur heard best at the apex. Which of the following is the most likely cause of this patient's hoarseness?
- A. Carcinoma arising from the mucosa of the larynx
- B. Laryngeal inflammation due to chemical irritant
- C. Circulating acetylcholine receptor antibodies
- D. Extrinsic impingement of the recurrent laryngeal nerve (Correct Answer)
- E. Bacterial infection of the vocal folds
Fourth and sixth pharyngeal arch derivatives Explanation: ***Extrinsic impingement of the recurrent laryngeal nerve***
- The combination of **hoarseness**, **irregular pulse**, **exertional dyspnea**, a **soft diastolic murmur**, and **hepatomegaly** in an older patient strongly suggests heart failure with left atrial enlargement, which can compress the **left recurrent laryngeal nerve** (Ortner's syndrome).
- The recurrent laryngeal nerve controls the intrinsic muscles of the larynx, and its compression leads to **vocal cord paralysis** and hoarseness.
*Carcinoma arising from the mucosa of the larynx*
- While laryngeal carcinoma can cause hoarseness, the additional symptoms of **exertional dyspnea**, **irregular pulse**, **diastolic murmur**, and **hepatomegaly** are not typically associated with primary laryngeal cancer.
- The patient's lack of smoking and alcohol history makes laryngeal carcinoma less likely, although not impossible.
*Laryngeal inflammation due to chemical irritant*
- This would typically present with hoarseness and possibly cough, but it would not explain the systemic findings of **irregular pulse**, **dyspnea**, **diastolic murmur**, or **hepatomegaly**.
- Without exposure to irritants, this cause is less probable.
*Circulating acetylcholine receptor antibodies*
- This condition is **myasthenia gravis**, which can cause generalized weakness, including weakness of laryngeal muscles leading to hoarseness and dyspnea.
- However, the other findings like an **irregular pulse**, **diastolic murmur**, and **hepatomegaly** are not characteristic features of myasthenia gravis, making it less likely.
*Bacterial infection of the vocal folds*
- A bacterial infection (laryngitis) would typically present with acute onset hoarseness, sore throat, and possibly fever.
- It would not account for the chronic nature of the symptoms (5 months) or the associated cardiac and hepatic findings.
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 7: A 2850-g (6-lb 5-oz) newborn is delivered at term to a 19-year-old primigravid woman via normal spontaneous vaginal delivery. The mother has had no prenatal care. Examination of the newborn in the delivery room shows malformed external ears, facial nerve palsy, and absence of the stapes bone on audiological testing. This patient's condition is most likely caused by abnormal development of the structure that also gives rise to which of the following?
- A. Muscles of mastication (Correct Answer)
- B. Maxillary process
- C. Meckel's cartilage
- D. Palatine tonsil
- E. Trigeminal nerve (CN V)
Fourth and sixth pharyngeal arch derivatives Explanation: ***Muscles of mastication***
- The patient's presentation with **malformed external ears, facial nerve palsy (CN VII), and absence of the stapes** is characteristic of **second pharyngeal arch** abnormalities (seen in conditions like hemifacial microsomia or other branchial arch syndromes).
- The **second pharyngeal arch** (Reichert's cartilage) gives rise to the stapes, muscles of facial expression, styloid process, and is associated with CN VII (facial nerve).
- However, this question asks what else derives from "the structure" causing these findings. Since the **muscles of mastication derive from the first pharyngeal arch**, this appears to test understanding that they are NOT from the same arch as the stapes.
- **NOTE:** If this represents a combined first and second arch syndrome, then muscles of mastication (first arch) could be co-affected, making this the correct answer in that clinical context.
*Maxillary process*
- The maxillary process is derived from the **first pharyngeal arch** and forms the maxilla, zygoma, and part of the temporal bone.
- This is not derived from the second pharyngeal arch, which is primarily affected in this patient based on the stapes absence and facial nerve palsy.
*Meckel's cartilage*
- **Meckel's cartilage** is the cartilaginous component of the **first pharyngeal arch** and gives rise to the malleus, incus, anterior ligament of malleus, and sphenomandibular ligament.
- The **stapes** originates from the **second pharyngeal arch** (Reichert's cartilage), not Meckel's cartilage, making this an incorrect association.
*Palatine tonsil*
- The palatine tonsil develops from the **second pharyngeal pouch** (endoderm), not from the pharyngeal arches (mesoderm).
- Pouch derivatives are distinct from arch derivatives and are not involved in the skeletal and nerve malformations described.
*Trigeminal nerve (CN V)*
- The trigeminal nerve is the nerve of the **first pharyngeal arch** and provides sensory innervation to the face and motor innervation to the muscles of mastication.
- The **facial nerve (CN VII)** is the nerve of the **second pharyngeal arch**, which is the arch primarily affected in this clinical presentation.
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 8: A 25-year-old woman gives birth to a male child at 30 weeks of gestation. Pregnancy was complicated by polyhydramnios diagnosed on ultrasonography at 26 weeks of gestation. The baby is born vaginally weighing 1.2 kg (2.64 lb). Because he does not cry immediately after birth, endotracheal intubation is attempted to secure the airway. However, the vocal cords cannot be visualized because there is only a single opening corresponding to the esophagus. He is transferred to the NICU under bag and mask ventilation, where intubation is attempted once again by passing the endotracheal tube in the visualized opening, after which his oxygen saturation begins to improve. His temperature is 37.0ºC (98.6°F), pulse is 120/min, and respiratory rate is 42/min. On physical examination, no abnormalities are noted. Chest radiography is suggestive of respiratory distress syndrome. Which of the following most likely failed to develop in this patient?
- A. Second branchial arch
- B. Mesonephric duct
- C. Fourth and sixth branchial arches (Correct Answer)
- D. First branchial arch
- E. Third branchial arch
Fourth and sixth pharyngeal arch derivatives Explanation: ***Fourth and sixth branchial arches***
- The clinical presentation of **inability to visualize the vocal cords** and the presence of only a **single opening** suggests **laryngeal atresia** or severe laryngotracheal malformation. While the laryngotracheal structures primarily develop from the laryngotracheal diverticulum (an outgrowth of the foregut), the **fourth and sixth pharyngeal arches** are critical for the development of **laryngeal cartilages** and **innervation**:
- **Fourth arch**: Contributes to the thyroid cartilage, cricothyroid muscle, and superior laryngeal nerve
- **Sixth arch**: Forms the cricoid cartilage, arytenoid cartilages, and provides the recurrent laryngeal nerve (innervating all intrinsic laryngeal muscles except cricothyroid)
- Failure of proper development of these arches results in **absence or malformation of the larynx**, preventing normal vocal cord formation and airway development.
- The **polyhydramnios** occurs because the fetus cannot swallow amniotic fluid effectively due to airway obstruction.
*Second branchial arch*
- The **second branchial arch** (hyoid arch) contributes to the **stapes**, styloid process, stylohyoid ligament, lesser horn and upper body of the hyoid bone, and muscles of facial expression (via facial nerve).
- Defects in this arch typically lead to conditions like **Treacher Collins syndrome** or hemifacial microsomia, not laryngeal agenesis.
*Mesonephric duct*
- The **mesonephric duct (Wolffian duct)** is an embryonic structure crucial for the development of male internal reproductive organs including the **epididymis**, vas deferens, seminal vesicles, and ejaculatory duct.
- Failure of this duct to develop would result in male reproductive anomalies, not respiratory tract malformations.
*First branchial arch*
- The **first branchial arch** (mandibular arch) gives rise to the **maxilla, mandible, malleus, incus**, muscles of mastication, and trigeminal nerve branches.
- Malformations of this arch are associated with conditions like **Pierre Robin sequence** or mandibulofacial dysostosis, presenting with micrognathia and facial abnormalities, which are not described in this case.
*Third branchial arch*
- The **third branchial arch** forms the **greater horn and lower body of the hyoid bone**, stylopharyngeus muscle, and glossopharyngeal nerve.
- Anomalies of this arch may present with swallowing difficulties or glossopharyngeal nerve deficits, but do not cause the complete absence of laryngeal structures described in this scenario.
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 9: A group of investigators studying embryological defects in mice knock out a gene that is responsible for the development of the ventral wing of the third branchial pouch. A similar developmental anomaly in a human embryo is most likely to result in which of the following findings after birth?
- A. Cleft palate
- B. Discharging neck sinus (Correct Answer)
- C. Carpopedal spasm
- D. Conductive hearing loss
- E. White oral patches
Fourth and sixth pharyngeal arch derivatives Explanation: ***Discharging neck sinus***
- The **ventral wing of the third pharyngeal pouch** gives rise to the **thymus**
- During embryonic development, the thymus descends from the pharynx into the anterior mediastinum via the **thymopharyngeal duct**
- Normally, this duct obliterates completely, but **failure of obliteration** can result in a **cervical thymic cyst** or **persistent thymic tract**
- This presents as a **discharging neck sinus** along the lateral neck (anterior border of sternocleidomastoid), which may drain clear fluid or become infected
- This is a classic presentation of a **third pharyngeal pouch anomaly** affecting the thymic descent pathway
*Carpopedal spasm*
- **Carpopedal spasm** is a sign of **hypocalcemia** due to **hypoparathyroidism**
- The **dorsal wing** (not ventral wing) of the third pharyngeal pouch forms the **inferior parathyroid glands**
- Since the question specifically identifies a defect in the **ventral wing** (thymus), hypoparathyroidism would not result
- A dorsal wing defect would cause absent inferior parathyroid glands and hypocalcemia
*Cleft palate*
- Results from failure of **palatine shelf fusion** during weeks 8-12 of development
- Associated with **maxillary prominence** derivatives (first pharyngeal arch) and secondary palate formation
- Not related to third pharyngeal pouch development
*Conductive hearing loss*
- Associated with **first and second pharyngeal arch** derivatives affecting the middle ear structures
- First arch: malleus, incus (in part); Second arch: stapes (in part)
- The **third pharyngeal pouch** does not contribute to auditory structures
*White oral patches*
- Typically represent **mucosal lesions** (leukoplakia, candidiasis, lichen planus)
- Not associated with embryological defects of the pharyngeal apparatus
- Unrelated to third pharyngeal pouch derivatives
Fourth and sixth pharyngeal arch derivatives US Medical PG Question 10: A 64-year-old woman presents to an endocrinologist after her second time having a kidney stone in the last year. The patient reports no other symptoms except overall fatigue. On evaluation, the patient’s temperature is 98.4°F (36.9°C), blood pressure is 120/76 mmHg, pulse is 72/min, and respirations are 12/min. The patient has no neck masses and no tenderness to palpation in the abdomen. On laboratory workup, the endocrinologist finds that the patient has elevated parathyroid hormone levels and serum calcium. For surgical planning, the patient undergoes a sestamibi scan, which localizes disease to an area near the superior aspect of the thyroid in the right neck. Which of the following is the embryologic origin of this tissue?
- A. Fourth branchial arch
- B. Fourth branchial pouch (Correct Answer)
- C. Third branchial arch
- D. Dorsal wings of the third branchial pouch
- E. Ventral wings of the third branchial pouch
Fourth and sixth pharyngeal arch derivatives Explanation: ***Fourth branchial pouch***
- The superior parathyroid glands, generally located near the superior aspect of the thyroid, develop from the **fourth branchial pouch (dorsal wing)**.
- The **ultimobranchial body (C-cells)** also originates from the fourth branchial pouch.
*Fourth branchial arch*
- The fourth branchial arch forms structures like the **cricothyroid muscle**, pharyngeal constrictors, and laryngeal cartilages.
- It does not give rise to the parathyroid glands.
*Third branchial arch*
- The third branchial arch forms structures including the **stylopharyngeus muscle**, greater horn of the hyoid, and parts of the pharynx.
- It does not contribute to the formation of the parathyroid glands.
*Dorsal wings of the third branchial pouch*
- The **dorsal wings of the third branchial pouch** give rise to the inferior parathyroid glands.
- In this case, the diseased tissue was localized to the superior aspect nearest the superior parathyroid glands, not the inferior glands.
*Ventral wings of the third branchial pouch*
- The **ventral wings of the third branchial pouch** give rise to the thymus.
- This structure is not involved in parathyroid gland development.
More Fourth and sixth pharyngeal arch derivatives US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.