Clinical correlations of pharyngeal development US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Clinical correlations of pharyngeal development. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Clinical correlations of pharyngeal development US Medical PG Question 1: A 4-year-old girl is brought by her mother to the pediatrician for neck drainage. The mother reports that the child has always had a small pinpoint opening on the front of her neck, though the opening has never been symptomatic. The child developed a minor cold approximately 10 days ago which resolved after a week. However, over the past 2 days, the mother has noticed clear thick drainage from the opening on the child’s neck. The child is otherwise healthy. She had an uncomplicated birth and is currently in the 45th and 40th percentiles for height and weight, respectively. On examination, there is a small opening along the skin at the anterior border of the right sternocleidomastoid at the junction of the middle and lower thirds of the neck. There is some slight clear thick discharge from the opening. Palpation around the opening elicits a cough from the child. This patient’s condition is caused by tissue that also forms which of the following?
- A. Epithelial tonsillar lining (Correct Answer)
- B. Thymus gland
- C. Epithelial lining of the Eustachian tube
- D. Superior parathyroid glands
- E. Inferior parathyroid glands
Clinical correlations of pharyngeal development Explanation: ***Epithelial tonsillar lining***
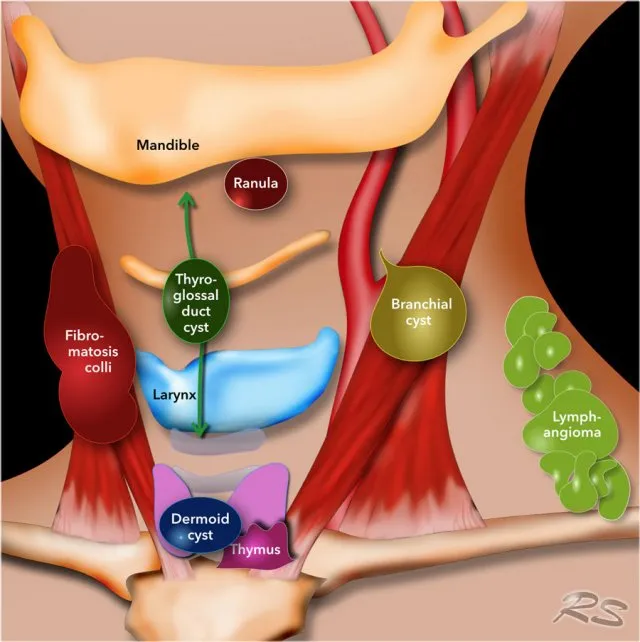
- The clinical presentation of a **pinpoint opening with drainage along the anterior border of the sternocleidomastoid muscle**, especially with **cough elicited upon palpation**, is highly suggestive of a **second branchial cleft cyst/fistula**.
- This condition arises from incomplete obliteration of the **second branchial cleft**, which is part of the second pharyngeal arch complex.
- The **second pharyngeal pouch** (endodermal component of the second arch complex) forms the **epithelial lining of the palatine tonsils**.
- While the cleft (ectodermal) and pouch (endodermal) are technically distinct, they both derive from the second pharyngeal arch apparatus.
*Thymus gland*
- The **thymus gland** develops from the **third pharyngeal pouch**, not the second pharyngeal arch complex.
- Abnormalities of the thymus typically present as issues with immune function or mediastinal masses, not lateral neck drainage.
*Epithelial lining of the Eustachian tube*
- The **Eustachian tube** (auditory tube) develops from the **first pharyngeal pouch**.
- Manifestations related to the Eustachian tube typically involve middle ear issues, not drainage in the lateral neck.
*Superior parathyroid glands*
- The **superior parathyroid glands** develop from the **fourth pharyngeal pouch**.
- Dysgenesis of these glands leads to issues with calcium regulation (hypoparathyroidism), not neck fistulas.
*Inferior parathyroid glands*
- The **inferior parathyroid glands** develop from the **third pharyngeal pouch**, along with the thymus.
- Similar to the superior parathyroids, their abnormalities are related to calcium metabolism and would not present as a draining neck lesion.
Clinical correlations of pharyngeal development US Medical PG Question 2: A 2720-g (6-lb) female newborn is delivered at term to a 39-year-old woman, gravida 3, para 2. Examination in the delivery room shows micrognathia, prominent occiput with flattened nasal bridge, and pointy low-set ears. The eyes are upward slanting with small palpebral fissures. The fists are clenched with fingers tightly flexed. The index finger overlaps the third finger and the fifth finger overlaps the fourth. A 3/6 holosystolic murmur is heard at the lower left sternal border. The nipples are widely spaced and the feet have prominent heels and convex, rounded soles. Which of the following is the most likely cause of these findings?
- A. Deletion of Chromosome 5p
- B. Trisomy 13
- C. Fetal alcohol syndrome
- D. Trisomy 18 (Correct Answer)
- E. Trisomy 21
Clinical correlations of pharyngeal development Explanation: **_Trisomy 18_**
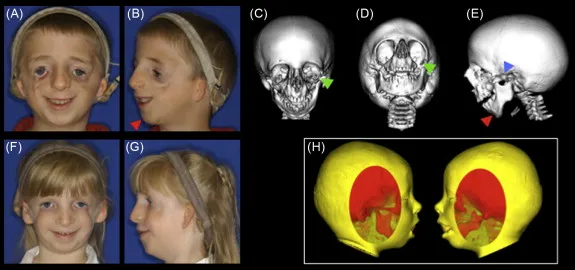
- The constellation of findings, including **micrognathia**, prominent occiput, **low-set ears**, short palpebral fissures, **clenched fists with overlapping fingers**, widely spaced nipples, and **rocker-bottom feet**, are classic signs of **Edwards syndrome (Trisomy 18)**.
- The **holosystolic murmur** suggests a **ventricular septal defect (VSD)**, which is commonly associated with Trisomy 18.
*Deletion of Chromosome 5p*
- This is associated with **Cri-du-chat syndrome**, characterized by a **cat-like cry**, microcephaly, and intellectual disability.
- The classic features described in the case, such as rocker-bottom feet and overlapping fingers, are not typical of Cri-du-chat syndrome.
*Trisomy 13*
- This is **Patau syndrome**, characterized by **polydactyly**, cleft lip/palate, microphthalmia, and cutis aplasia.
- While it shares some features of severe developmental abnormalities, the specific hand posture and ear/facial anomalies point away from Trisomy 13.
*Fetal alcohol syndrome*
- This condition presents with **facial dysmorphology** (short palpebral fissures, thin upper lip, smooth philtrum), growth restriction, and intellectual disability.
- It does not typically include the prominent occiput, micrognathia, or characteristic finger positioning and foot deformities seen in this patient.
*Trisomy 21*
- Also known as **Down syndrome**, characterized by features such as **epicanthal folds**, upslanting palpebral fissures, a single palmar crease, and hypotonia.
- While some features like a VSD can overlap, the specific facial features and skeletal anomalies (e.g., clenched fists with overlapping fingers, rocker-bottom feet) are distinctly different from Down syndrome.
Clinical correlations of pharyngeal development US Medical PG Question 3: A child is born by routine delivery and quickly develops respiratory distress. He is noted to have epicanthal folds, low-set ears that are pressed against his head, widely set eyes, a broad, flat nose, clubbed feet, and a receding chin. The mother had one prenatal visit, at which time the routine ultrasound revealed an amniotic fluid index of 3 cm. What is the most likely underlying cause of this patient's condition?
- A. Unilateral renal agenesis
- B. An extra 18th chromosome
- C. Autosomal recessive polycystic kidney disease (ARPKD)
- D. A microdeletion in chromosome 22
- E. Bilateral renal agenesis (Correct Answer)
Clinical correlations of pharyngeal development Explanation: ***Bilateral renal agenesis***
- The combination of **amniotic fluid index (AFI) of 3 cm** (indicating **oligohydramnios**) and multiple facial and limb anomalies strongly suggests **Potter sequence**.
- **Bilateral renal agenesis** is the most common cause of **Potter sequence**, leading to absence of fetal urine production and subsequent oligohydramnios, which restricts fetal movement and lung development.
*Unilateral renal agenesis*
- **Unilateral renal agenesis** typically does not cause **oligohydramnios** because the single functioning kidney can produce sufficient urine.
- While it can be associated with other anomalies, the severe extent of Potter sequence features described here is unlikely with only unilateral involvement.
*An extra 18th chromosome*
- An extra 18th chromosome refers to **Edwards syndrome (Trisomy 18)**, which presents with severe intellectual disability, micrognathia, prominent occiput, and rocker-bottom feet.
- While Edwards syndrome is associated with a variety of anomalies, including renal issues, the constellation of features (especially the clear link to oligohydramnios and respiratory distress) points more directly to Potter sequence.
*Autosomal recessive polycystic kidney disease (ARPKD)*
- **ARPKD** causes **enlarged, cystic kidneys** and can lead to **oligohydramnios** and respiratory distress due to renal insufficiency.
- However, the description of **epicanthal folds, low-set ears, widely set eyes, and a broad, flat nose** is more characteristic of the **Potter facies** seen in severe oligohydramnios, rather than specific to ARPKD itself.
*A microdeletion in chromosome 22*
- A microdeletion in chromosome 22 typically refers to **22q11.2 deletion syndrome (DiGeorge syndrome)**, which is associated with **cardiac defects**, **abnormal facies**, **thymic hypoplasia**, **cleft palate**, and **hypocalcemia**.
- While renal anomalies can occur in DiGeorge syndrome, the primary presentation is not characterized by the severe oligohydramnios and classic Potter sequence features described.
Clinical correlations of pharyngeal development US Medical PG Question 4: A 25-year-old man presents to the clinic with a midline swelling in his neck. He is unsure about when it appeared. He denies any difficulty with swallowing or hoarseness. His past medical history is insignificant. On physical examination, there is a 1 cm x 2 cm firm mildly tender nodule on the anterior midline aspect of the neck which moves with deglutition and elevates with protrusion of the tongue. Which of the following is the most likely embryologic origin of the nodule in this patient?
- A. Midline endoderm of the pharynx (Correct Answer)
- B. 1st and 2nd pharyngeal arch
- C. The branchial cleft
- D. 4th pharyngeal arch
- E. 4th pharyngeal pouch
Clinical correlations of pharyngeal development Explanation: ***Midline endoderm of the pharynx***
- The symptoms described, particularly a midline neck swelling that **moves with deglutition** and **elevates with tongue protrusion**, are classic for a **thyroglossal duct cyst**.
- Thyroglossal duct cysts arise from remnants of the **thyroglossal duct**, an embryonic structure that forms from the **midline endoderm of the pharyngeal floor** and descends to form the thyroid gland.
*1st and 2nd pharyngeal arch*
- The 1st and 2nd pharyngeal arches primarily contribute to the formation of structures in the **mandible**, **maxilla**, **middle ear**, and **hyoid bone**.
- Abnormalities in these arches typically lead to conditions like **Treacher Collins syndrome** or **Pierre Robin sequence**, not midline neck cysts with these specific movement characteristics.
*The branchial cleft*
- **Branchial cleft cysts** typically present as **lateral neck masses**, often anterior to the sternocleidomastoid muscle, and usually do not move with deglutition or tongue protrusion.
- They arise from incomplete obliteration of **pharyngeal clefts**, which are ectodermal structures.
*4th pharyngeal arch*
- The 4th pharyngeal arch contributes to the formation of the **cricothyroid muscle**, part of the **pharynx**, and the **laryngeal cartilages**.
- Anomalies of the 4th pharyngeal arch are rare and typically involve **vascular structures** or **recurrent laryngeal nerve** abnormalities, not midline neck cysts.
*4th pharyngeal pouch*
- The 4th pharyngeal pouch contributes to the development of the **superior parathyroid glands** and the **ultimobranchial body** (which gives rise to parafollicular C cells of the thyroid).
- Malformations of this pouch are associated with parathyroid and thyroid conditions, not midline thyroglossal duct cysts.
Clinical correlations of pharyngeal development US Medical PG Question 5: A 2850-g (6-lb 5-oz) newborn is delivered at term to a 19-year-old primigravid woman via normal spontaneous vaginal delivery. The mother has had no prenatal care. Examination of the newborn in the delivery room shows malformed external ears, facial nerve palsy, and absence of the stapes bone on audiological testing. This patient's condition is most likely caused by abnormal development of the structure that also gives rise to which of the following?
- A. Muscles of mastication (Correct Answer)
- B. Maxillary process
- C. Meckel's cartilage
- D. Palatine tonsil
- E. Trigeminal nerve (CN V)
Clinical correlations of pharyngeal development Explanation: ***Muscles of mastication***
- The patient's presentation with **malformed external ears, facial nerve palsy (CN VII), and absence of the stapes** is characteristic of **second pharyngeal arch** abnormalities (seen in conditions like hemifacial microsomia or other branchial arch syndromes).
- The **second pharyngeal arch** (Reichert's cartilage) gives rise to the stapes, muscles of facial expression, styloid process, and is associated with CN VII (facial nerve).
- However, this question asks what else derives from "the structure" causing these findings. Since the **muscles of mastication derive from the first pharyngeal arch**, this appears to test understanding that they are NOT from the same arch as the stapes.
- **NOTE:** If this represents a combined first and second arch syndrome, then muscles of mastication (first arch) could be co-affected, making this the correct answer in that clinical context.
*Maxillary process*
- The maxillary process is derived from the **first pharyngeal arch** and forms the maxilla, zygoma, and part of the temporal bone.
- This is not derived from the second pharyngeal arch, which is primarily affected in this patient based on the stapes absence and facial nerve palsy.
*Meckel's cartilage*
- **Meckel's cartilage** is the cartilaginous component of the **first pharyngeal arch** and gives rise to the malleus, incus, anterior ligament of malleus, and sphenomandibular ligament.
- The **stapes** originates from the **second pharyngeal arch** (Reichert's cartilage), not Meckel's cartilage, making this an incorrect association.
*Palatine tonsil*
- The palatine tonsil develops from the **second pharyngeal pouch** (endoderm), not from the pharyngeal arches (mesoderm).
- Pouch derivatives are distinct from arch derivatives and are not involved in the skeletal and nerve malformations described.
*Trigeminal nerve (CN V)*
- The trigeminal nerve is the nerve of the **first pharyngeal arch** and provides sensory innervation to the face and motor innervation to the muscles of mastication.
- The **facial nerve (CN VII)** is the nerve of the **second pharyngeal arch**, which is the arch primarily affected in this clinical presentation.
Clinical correlations of pharyngeal development US Medical PG Question 6: During embryological development, failure of the lateral palatine processes to fuse with the primary palate results in which of the following conditions?
- A. Pierre Robin sequence
- B. Submucous cleft
- C. Isolated cleft palate (Correct Answer)
- D. Bifid uvula
Clinical correlations of pharyngeal development Explanation: ***Isolated cleft palate***
- This condition occurs when the **lateral palatine processes** (secondary palate) **fail to fuse** with each other and/or with the **primary palate**. [1]
- It results in an **opening between the oral and nasal cavities**, affecting feeding and speech. [1]
*Pierre Robin sequence*
- Characterized by **micrognathia**, **glossoptosis**, and often a **U-shaped cleft palate**.
- While a cleft palate can be present, the defining features are the small mandible and posterior displacement of the tongue.
*Submucous cleft*
- Involves failure of **muscle or bone fusion under intact mucous membranes**.
- It can be difficult to diagnose visually, often identified by a **bifid uvula**, notch in the hard palate, or abnormal muscle function of the soft palate.
*Bifid uvula*
- This is a mild form of **cleft palate**, where only the **uvula is split**.
- It indicates incomplete fusion of the palatine shelves but does not represent a full failure of the lateral palatine processes to fuse with the primary palate.
Clinical correlations of pharyngeal development US Medical PG Question 7: An investigator is studying the teratogenicity of cigarette smoking during pregnancy. He reviews several databases containing data about birth defects and prenatal drug exposures and finds that infants exposed to cigarette smoke in utero are approximately 2 times as likely to have a particular birth defect than unexposed infants. This defect results from abnormal development during the 6th week of gestation, when the maxillary prominences grow medially and fuse first with the lateral and then the medial nasal prominence. The defect is most likely which of the following?
- A. Cleft palate
- B. Macrognathia
- C. Torus palatinus
- D. Choanal atresia
- E. Cleft lip (Correct Answer)
Clinical correlations of pharyngeal development Explanation: ***Cleft lip***
- **Cleft lip** results from the incomplete fusion of the **medial nasal prominence** and the **maxillary prominence**, which normally occurs around the 6th week of gestation.
- Exposure to **cigarette smoking** during pregnancy is a known **teratogen** that increases the risk of this developmental abnormality.
*Cleft palate*
- **Cleft palate** involves the incomplete fusion of the **palatal shelves**, occurring later in gestation (weeks 7-12), and is a separate developmental defect from cleft lip.
- While smoking can increase the risk of cleft palate, the described embryological event (fusion of maxillary and nasal prominences) specifically leads to **cleft lip**.
*Macrognathia*
- **Macrognathia** refers to an abnormally large jaw, which is a growth anomaly rather than a failure of fusion of facial prominences.
- This condition is not directly related to the developmental processes described in the question.
*Torus palatinus*
- **Torus palatinus** is a benign bony protuberance on the hard palate, often a genetically inherited trait, and is not a birth defect caused by failed embryonic fusion.
- It develops much later in life or can be present from birth but does not involve the specific embryonic structures mentioned.
*Choanal atresia*
- **Choanal atresia** is a blockage of the posterior nasal passage, caused by the failure of the **nasal cavity** to communicate with the **nasopharynx**.
- This defect is not related to the fusion of the maxillary and nasal prominences, which forms the upper lip and primary palate.
Clinical correlations of pharyngeal development US Medical PG Question 8: A 25-year-old woman gives birth to a male child at 30 weeks of gestation. Pregnancy was complicated by polyhydramnios diagnosed on ultrasonography at 26 weeks of gestation. The baby is born vaginally weighing 1.2 kg (2.64 lb). Because he does not cry immediately after birth, endotracheal intubation is attempted to secure the airway. However, the vocal cords cannot be visualized because there is only a single opening corresponding to the esophagus. He is transferred to the NICU under bag and mask ventilation, where intubation is attempted once again by passing the endotracheal tube in the visualized opening, after which his oxygen saturation begins to improve. His temperature is 37.0ºC (98.6°F), pulse is 120/min, and respiratory rate is 42/min. On physical examination, no abnormalities are noted. Chest radiography is suggestive of respiratory distress syndrome. Which of the following most likely failed to develop in this patient?
- A. Second branchial arch
- B. Mesonephric duct
- C. Fourth and sixth branchial arches (Correct Answer)
- D. First branchial arch
- E. Third branchial arch
Clinical correlations of pharyngeal development Explanation: ***Fourth and sixth branchial arches***
- The clinical presentation of **inability to visualize the vocal cords** and the presence of only a **single opening** suggests **laryngeal atresia** or severe laryngotracheal malformation. While the laryngotracheal structures primarily develop from the laryngotracheal diverticulum (an outgrowth of the foregut), the **fourth and sixth pharyngeal arches** are critical for the development of **laryngeal cartilages** and **innervation**:
- **Fourth arch**: Contributes to the thyroid cartilage, cricothyroid muscle, and superior laryngeal nerve
- **Sixth arch**: Forms the cricoid cartilage, arytenoid cartilages, and provides the recurrent laryngeal nerve (innervating all intrinsic laryngeal muscles except cricothyroid)
- Failure of proper development of these arches results in **absence or malformation of the larynx**, preventing normal vocal cord formation and airway development.
- The **polyhydramnios** occurs because the fetus cannot swallow amniotic fluid effectively due to airway obstruction.
*Second branchial arch*
- The **second branchial arch** (hyoid arch) contributes to the **stapes**, styloid process, stylohyoid ligament, lesser horn and upper body of the hyoid bone, and muscles of facial expression (via facial nerve).
- Defects in this arch typically lead to conditions like **Treacher Collins syndrome** or hemifacial microsomia, not laryngeal agenesis.
*Mesonephric duct*
- The **mesonephric duct (Wolffian duct)** is an embryonic structure crucial for the development of male internal reproductive organs including the **epididymis**, vas deferens, seminal vesicles, and ejaculatory duct.
- Failure of this duct to develop would result in male reproductive anomalies, not respiratory tract malformations.
*First branchial arch*
- The **first branchial arch** (mandibular arch) gives rise to the **maxilla, mandible, malleus, incus**, muscles of mastication, and trigeminal nerve branches.
- Malformations of this arch are associated with conditions like **Pierre Robin sequence** or mandibulofacial dysostosis, presenting with micrognathia and facial abnormalities, which are not described in this case.
*Third branchial arch*
- The **third branchial arch** forms the **greater horn and lower body of the hyoid bone**, stylopharyngeus muscle, and glossopharyngeal nerve.
- Anomalies of this arch may present with swallowing difficulties or glossopharyngeal nerve deficits, but do not cause the complete absence of laryngeal structures described in this scenario.
Clinical correlations of pharyngeal development US Medical PG Question 9: A 29-year-old mother brings in her 2-week-old baby boy to a pediatrician because he has been having difficulty feeding. The mother reveals that she had no prenatal care during her pregnancy and gave birth at home without complications. She says that her son seems to be having difficulty sucking, and she occasionally sees breast milk coming out of the infant’s nose. Physical exam reveals that this patient has a gap between his oral and nasal cavities behind the incisive foramen. He is therefore prescribed specialized bottles and his mom is taught positional techniques to ensure better feeding. Failure to fuse which of the following structures is most likely responsible for this patient's disorder?
- A. Maxillary and medial nasal prominences
- B. Nasal septum with primary plates
- C. Maxillary and lateral nasal prominences
- D. Palatine shelves with primary plates
- E. Palatine shelves with nasal septum (Correct Answer)
Clinical correlations of pharyngeal development Explanation: ***Palatine shelves with nasal septum***
- A **cleft palate** results from the **failure of fusion of the palatine shelves** with each other and/or with the **nasal septum**, creating an abnormal communication between the oral and nasal cavities.
- This anatomical defect explains the infant's **feeding difficulties** and the leakage of breast milk into the nose, as well as the observed **gap behind the incisive foramen**.
*Maxillary and medial nasal prominences*
- The failure of fusion between the maxillary and medial nasal prominences results in a **cleft lip**, which is an anterior defect and does not explain the posterior gap described.
- While cleft lip can coexist with cleft palate, the symptoms here specifically point to a palatal defect, not primarily a lip defect.
*Nasal septum with primary plates*
- The primary palate forms from the fusion of the medial nasal prominences, anterior to the incisive foramen.
- While crucial for normal development, the specific clinical presentation (gap *behind* the incisive foramen and feeding difficulties) is more characteristic of a secondary palate defect involving the palatine shelves.
*Maxillary and lateral nasal prominences*
- The fusion of these structures contributes to the formation of the **nasolacrimal groove** and parts of the cheek, not the palate.
- Deficiencies in this fusion would lead to defects in the lateral facial region, not an oro-nasal communication related to feeding.
*Palatine shelves with primary plates*
- The **primary palate** fuses with the anterior part of the secondary palate (formed by the palatine shelves) at the incisive foramen.
- However, the more common and clinically relevant defect leading to an open communication between the oral and nasal cavities, especially *behind* the incisive foramen, involves the failure of fusion of the **palatine shelves** with each other and the **nasal septum**.
Clinical correlations of pharyngeal development US Medical PG Question 10: A six year-old female presents for evaluation of dry skin, fatigue, sensitivity to cold and constipation. The patient’s mother recalls that the patient had surgery to remove a “benign mass” at the base of her tongue 3 months ago because of trouble swallowing. What was the likely cause of the surgically removed mass?
- A. Failed caudal migration of the thyroid gland (Correct Answer)
- B. Iodine deficiency
- C. Failed fusion of the palatine shelves with the nasal septum
- D. Radiation exposure
- E. Maternal Diabetes Mellitus
Clinical correlations of pharyngeal development Explanation: ***Failed caudal migration of the thyroid gland***
- The symptoms of **dry skin, fatigue, cold sensitivity, and constipation** are classic signs of **hypothyroidism**.
- A mass at the **base of the tongue** that is later removed and leads to hypothyroidism strongly suggests a **lingual thyroid**, which results from the thyroid gland's **failure to descend** from its embryonic origin at the foramen cecum.
*Iodine deficiency*
- While iodine deficiency can cause **hypothyroidism** and **goiter**, it typically does not present as a **discrete mass** at the base of the tongue requiring surgical removal.
- It would usually result in a more generalized **enlargement of the thyroid gland**, often in the neck.
*Failed fusion of the palatine shelves with the nasal septum*
- This developmental anomaly leads to a **cleft palate**, affecting the **roof of the mouth**.
- It has no direct association with thyroid function or masses at the base of the tongue.
*Radiation exposure*
- Radiation exposure can increase the risk of thyroid cancer or hypothyroidism later in life, but it typically doesn't cause a congenital benign mass at the base of the tongue that presents in early childhood.
- Furthermore, the specific presentation points to a developmental anomaly rather than an acquired condition.
*Maternal Diabetes Mellitus*
- Maternal diabetes can lead to various congenital anomalies in the fetus, such as **macrosomia, caudal regression syndrome, or cardiac defects**.
- However, it is not a recognized cause of a lingual thyroid or a failure of thyroid migration.
More Clinical correlations of pharyngeal development US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.