Urinary bladder and urethra US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Urinary bladder and urethra. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Urinary bladder and urethra US Medical PG Question 1: A 62-year-old man comes to the physician because of increased frequency of urination. He also says that he needs to urinate 4 to 5 times nightly and has difficulty initiating a urinary stream. He has had several episodes of acute cystitis treated with ciprofloxacin during the past year. Digital rectal examination shows a firm, symmetrically enlarged, non-tender prostate. This patient is most likely to develop which of the following complications?
- A. Inflammation of the renal interstitium
- B. Blastic bone lesions
- C. Abscess formation in the prostate
- D. Impaired intracavernosal blood flow
- E. Irreversible decrease in renal function (Correct Answer)
Urinary bladder and urethra Explanation: ***Irreversible decrease in renal function***
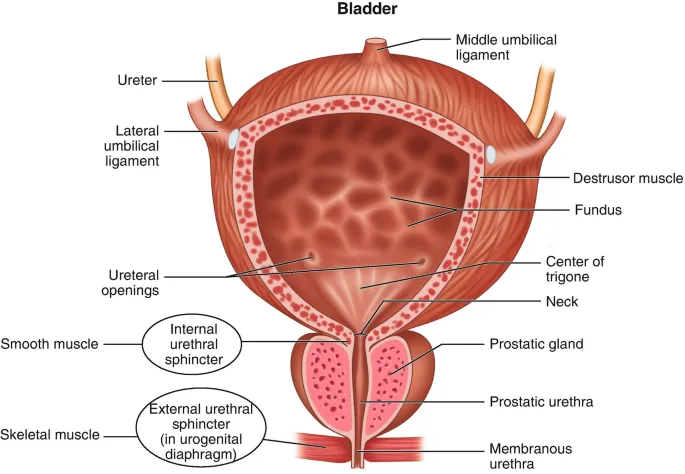
- The patient's symptoms of **increased urinary frequency**, **nocturia**, **difficulty initiating stream**, and **recurrent cystitis** in the context of a **symmetrically enlarged, firm prostate** are highly suggestive of **benign prostatic hyperplasia (BPH)** with progressive outflow obstruction.
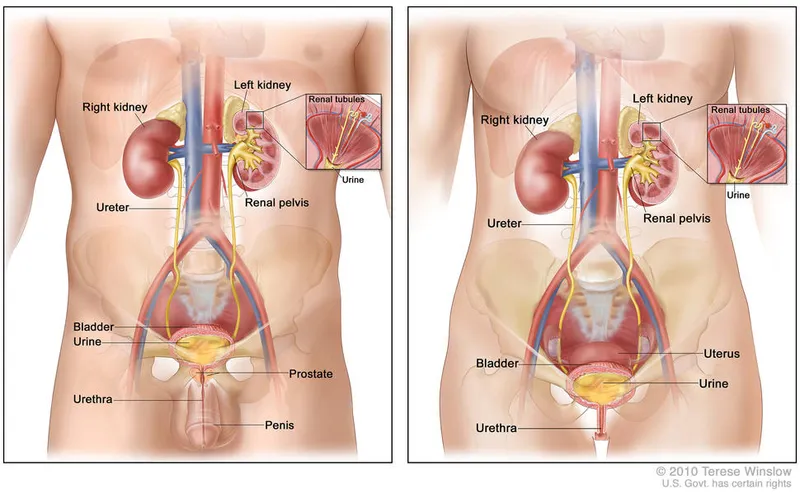
- Chronic urinary outflow obstruction can lead to **hydronephrosis** and **backpressure on the kidneys**, eventually causing **renal parenchymal damage** and an irreversible decrease in renal function.
*Inflammation of the renal interstitium*
- While chronic obstruction can lead to **chronic pyelonephritis**, which involves interstitial inflammation, **irreversible renal function decrease** is a more encompassing and severe long-term complication of sustained BPH with urinary retention.
- **Acute interstitial nephritis** is typically associated with drug reactions or systemic diseases, rather than primarily BPH.
*Blastic bone lesions*
- **Blastic bone lesions** are characteristic of **metastatic prostate cancer**, which typically presents with an **asymmetrically firm or nodular prostate** on DRE, unlike the symmetric enlargement described here.
- Although the patient's age and prostate exam warrant consideration of prostate cancer, the clinical picture strongly favors BPH, making blastic bone lesions less likely as the primary complication.
*Abscess formation in the prostate*
- **Prostatic abscesses** typically present with acute systemic symptoms like **fever, chills, and perineal pain**, which are not mentioned in this patient's presentation.
- While recurrent urinary tract infections can increase the risk of prostatic abscess, the dominant concern here is the long-term impact of chronic obstruction.
*Impaired intracavernosal blood flow*
- **Impaired intracavernosal blood flow** is a common cause of **erectile dysfunction**, which can coexist with BPH due to shared risk factors or age, but it's not a direct complication of the urinary outflow obstruction itself.
- The patient's reported symptoms are primarily related to urination and bladder emptying, not sexual function.
Urinary bladder and urethra US Medical PG Question 2: A 72-year-old multiparous woman comes to the physician for the evaluation of episodes of involuntary urine leakage for the past 6 months. She loses small amounts of urine without warning after laughing or sneezing. She also sometimes forgets the names of her grandchildren and friends. She is retired and lives at an assisted-living facility. She has insulin-dependent diabetes mellitus type 2. Her mother received a ventriculoperitoneal shunt around her age. She walks without any problems. Sensation to pinprick and light touch is normal. Which of the following is the primary underlying etiology for this patient's urinary incontinence?
- A. Urethral hypermobility (Correct Answer)
- B. Decreased cerebrospinal fluid absorption
- C. Detrusor-sphincter dyssynergia
- D. Impaired detrusor contractility
- E. Loss of sphincter control
Urinary bladder and urethra Explanation: ***Urethral hypermobility***
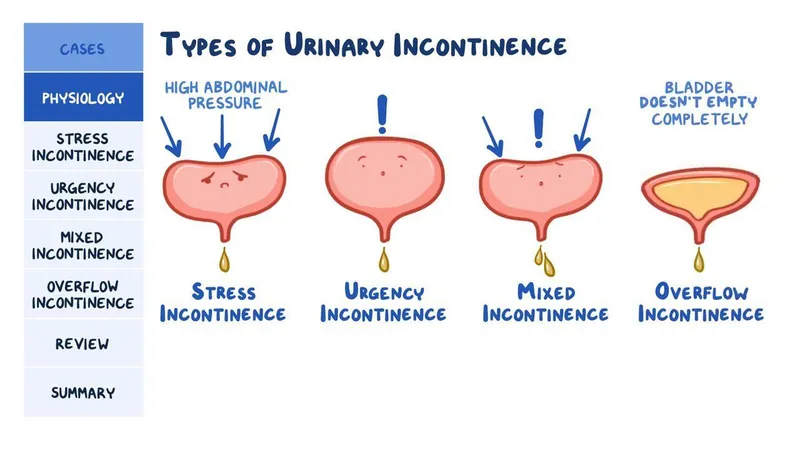
- This patient presents with **stress urinary incontinence**, characterized by involuntary urine leakage during activities that increase intra-abdominal pressure, such as **laughing or sneezing**.
- **Urethral hypermobility** is a common cause of stress incontinence, where the urethra and bladder neck rotate downward and backward during increased abdominal pressure, compromising sphincter function.
*Decreased cerebrospinal fluid absorption*
- This is linked to **normal pressure hydrocephalus**, presenting with a triad of **gait disturbance**, **urinary incontinence**, and **dementia**.
- While the patient has incontinence and memory issues, her normal gait and the absence of clear hydrocephalus symptoms makes this less likely to be the primary cause of her specific type of incontinence.
*Detrusor-sphincter dyssynergia*
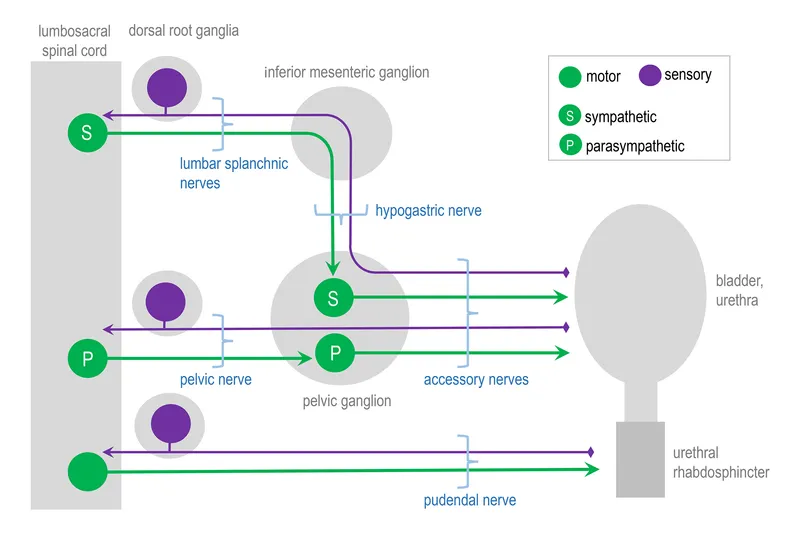
- This condition involves uncoordinated contraction of the **detrusor muscle** and external urethral sphincter, typically seen in individuals with **neurological disorders** like spinal cord injury.
- It results in incomplete bladder emptying and usually presents with urgency, frequency, and overflow incontinence, which does not match the patient's symptoms of leakage with straining.
*Impaired detrusor contractility*
- This leads to **overflow incontinence**, where the bladder is unable to empty completely and continuously leaks urine.
- Symptoms usually include a weak stream, hesitancy, and a feeling of incomplete emptying, which are not described in this patient.
*Loss of sphincter control*
- This can cause **stress incontinence**, but the term "loss of sphincter control" is a broad description. **Urethral hypermobility** specifically describes the mechanical mechanism leading to the loss of effective sphincter closure during exertion.
- While related, urethral hypermobility is a more specific and accurate primary etiology for stress incontinence in this context.
Urinary bladder and urethra US Medical PG Question 3: A 63-year-old woman visits her family physician because she has been experiencing difficulty to get her urine stream started in the past 8 months with many occasions needing extra effort to pass the urine. She describes the stream as intermittent and slow, and comments that she needs to go to the restroom again immediately after urinating. Her personal medical history is negative for malignancies, and all of her cytologies have been reported as normal. The only medication she takes is an angiotensin receptor blocker to treat essential hypertension diagnosed 5 years ago. Physical examination is unremarkable except for herniation of the anterior wall of the vagina that goes beyond the hymen. Which of the following types of incontinence is affecting the patient?
- A. Overflow incontinence (Correct Answer)
- B. Functional incontinence
- C. Mixed incontinence
- D. Stress incontinence
- E. Urgency incontinence
Urinary bladder and urethra Explanation: ***Overflow incontinence***
- The patient's symptoms of **difficulty initiating a urine stream**, **intermittent and slow stream**, **needing extra effort to pass urine**, and **feeling the need to urinate again immediately after** are classic signs of **urinary retention** and **overflow incontinence**.
- The presence of an **anterior vaginal wall herniation beyond the hymen** suggests a significant cystocele, which can obstruct the bladder outlet, leading to chronic incomplete bladder emptying and overflow.
*Functional incontinence*
- This type of incontinence occurs when a person has **normal bladder control** but is unable to reach the toilet in time due to **physical or cognitive impairments**, such as mobility issues, dementia, or severe depression.
- The patient's presentation does not describe any such physical or cognitive limitations preventing her from accessing the toilet.
*Mixed incontinence*
- Mixed incontinence is characterized by the presence of **both stress and urgency incontinence symptoms**.
- While it's a common type, the patient's primary symptoms are more indicative of outlet obstruction and incomplete emptying, rather than involuntary leakage with exertion or a sudden, strong urge.
*Stress incontinence*
- **Stress incontinence** is defined by involuntary urine leakage that occurs with **physical exertion** such as coughing, sneezing, laughing, or lifting.
- The patient's symptoms are primarily related to difficulty voiding and incomplete emptying, not leakage during physical activity.
*Urgency incontinence*
- **Urgency incontinence** is characterized by a **sudden, strong, and uncontrollable urge to urinate** that leads to involuntary urine leakage.
- While the patient mentions needing to go to the restroom again, her main symptoms revolve around obstructive voiding and incomplete emptying, rather than uncontrollable urges.
Urinary bladder and urethra US Medical PG Question 4: A 58-year-old obese male has noticed the gradual development of a soft bulge on his right groin that has been present over the past year and occasionally becomes very tender. He notices that it comes out when he coughs and strains during bowel movements. He is able to push the bulge back in without issue. After examination, you realize that he has an inguinal hernia and recommend open repair with mesh placement. After surgery, the patient returns to clinic and complains of numbness and tingling in the upper part of the scrotum and base of the penis. What nerve was most likely injured during the procedure?
- A. Ilioinguinal nerve (Correct Answer)
- B. Iliohypogastric nerve
- C. Lateral femoral cutaneous nerve
- D. Obturator nerve
- E. Genitofemoral nerve
Urinary bladder and urethra Explanation: **Ilioinguinal nerve**
- The **ilioinguinal nerve** supplies sensory innervation to the skin of the **scrotum** (or labia majora in females), the medial thigh, and the base of the penis.
- Injury to this nerve during an open inguinal hernia repair can cause **numbness and tingling** in these specific areas, consistent with the patient's symptoms.
*Iliohypogastric nerve*
- The **iliohypogastric nerve** primarily provides sensation to the skin over the **suprapubic region** and a small part of the buttock.
- Damage to this nerve would not typically result in numbness of the scrotum or base of the penis.
*Lateral femoral cutaneous nerve*
- This nerve is responsible for sensory innervation of the **lateral aspect of the thigh**.
- Its injury would lead to symptoms of numbness or pain on the lateral thigh (**meralgia paresthetica**), not the scrotum or penis.
*Obturator nerve*
- The **obturator nerve** is a motor nerve that innervates the **adductor muscles of the thigh** and provides sensory innervation to a small area of the medial thigh.
- Damage to this nerve would result in **adductor weakness** and sensory loss in the medial thigh, which does not match the patient's complaints.
*Genitofemoral nerve*
- The **genitofemoral nerve** has two branches: the genital branch (supplies the cremaster muscle and scrotal skin) and the femoral branch (supplies skin of the anterior thigh).
- While the genital branch does innervate the scrotum, injury to this nerve more commonly causes **cremasteric reflex loss** or pain radiating to the anterior thigh, and the described symptoms (base of penis) are more characteristic of ilioinguinal nerve involvement.
Urinary bladder and urethra US Medical PG Question 5: A child is in the nursery one day after birth. A nurse notices a urine-like discharge being expressed through the umbilical stump. What two structures in the embryo are connected by the structure that failed to obliterate during the embryologic development of this child?
- A. Kidney - large bowel
- B. Liver - umbilical vein
- C. Bladder - small bowel
- D. Pulmonary artery - aorta
- E. Bladder - umbilicus (Correct Answer)
Urinary bladder and urethra Explanation: ***Bladder - umbilicus***
- A **urine-like discharge** from the umbilical stump indicates a **patent urachus**, which is the embryonic remnant of the allantois.
- The **allantois** (which becomes the urachus) is an embryonic structure that connects the **fetal bladder** to the **umbilicus** during development.
- Normally, the allantois obliterates after birth to form the **median umbilical ligament**, but failure to obliterate results in a patent urachus allowing urine to discharge through the umbilicus.
*Kidney - large bowel*
- These two structures are not directly connected by an obliterating embryonic structure relevant to urine discharge from an umbilical stump.
- The kidneys form urine, and the large bowel is part of the digestive tract, with no direct embryonic communication to the umbilicus for urine expression.
*Liver - umbilical vein*
- The umbilical vein connects the **placenta to the fetal liver** (and ductus venosus) to transport oxygenated blood, not urine.
- Failure of the umbilical vein to obliterate would result in a patent umbilical vein, typically presenting as a vascular anomaly, not urine discharge.
*Pulmonary artery - aorta*
- These structures are connected by the **ductus arteriosus** in fetal circulation, bypassing the pulmonary circulation.
- While important for fetal development, a patent ductus arteriosus (PDA) is a cardiovascular anomaly and would not manifest as urine discharge from the umbilical stump.
*Bladder - small bowel*
- While both structures are involved in waste elimination, there is no normal embryonic structure directly connecting the bladder and small bowel that obliterates to prevent urine discharge from the umbilicus.
- An abnormal connection between the bladder and bowel would typically involve a **fistula** and present with stool in urine or urine in stool, not umbilical discharge.
Urinary bladder and urethra US Medical PG Question 6: A 47-year-old man is brought to the emergency department 1 hour after injuring his genital area when he fell astride his backyard fence. He was trimming a tree from the fence when he lost his balance. His vital signs are within normal limits. Examination shows blood at the urethral meatus, perineal ecchymoses, and a scrotal hematoma. An x-ray of the pelvis shows swelling of the soft tissue but no other abnormalities. Which part of the urinary tract is most likely damaged in this patient?
- A. Penile urethra
- B. Bulbous urethra (Correct Answer)
- C. Anterior bladder wall
- D. Prostatic urethra
- E. Membranous urethra
Urinary bladder and urethra Explanation: ***Bulbous urethra***
- Straddle injuries (falling astride an object) cause **direct compression of the bulbous urethra** against the inferior pubic ramus
- Classic triad: **blood at urethral meatus, perineal ecchymoses, and scrotal/perineal hematoma** (butterfly pattern)
- The bulbous urethra is part of the **anterior urethra** and is most vulnerable in blunt perineal trauma
- This is a **Buck's fascia injury** with characteristic perineal and scrotal swelling
*Penile urethra*
- More distal portion of anterior urethra within the penis
- Typically injured by **direct penile trauma** (penile fracture, penetrating injury, instrumentation)
- Would not produce the perineal ecchymoses and scrotal hematoma seen in this case
*Membranous urethra*
- Part of **posterior urethra** located within the urogenital diaphragm
- Typically injured with **pelvic fractures** (pubic rami fractures), which are absent in this case
- Would present with high-riding prostate on rectal exam and inability to void
*Prostatic urethra*
- Most proximal portion of posterior urethra, well-protected within the prostate
- Injured in **severe pelvic trauma** with disruption of puboprostatic ligaments
- Also associated with pelvic fractures, not straddle injuries
*Anterior bladder wall*
- Requires **pelvic fracture** or penetrating trauma
- Would present with **gross hematuria** and suprapubic pain/tenderness
- Blood at meatus is not typical; more likely to have abdominal distension and peritoneal signs
Urinary bladder and urethra US Medical PG Question 7: A 40-year-old sailor is brought to a military treatment facility 20 minutes after being involved in a navy ship collision. He appears ill. He reports a sensation that he needs to urinate but is unable to void. His pulse is 140/min, respirations are 28/min, and blood pressure is 104/70 mm Hg. Pelvic examination shows ecchymoses over the scrotum and perineum. There is tenderness over the suprapubic region and blood at the urethral meatus. Digital rectal examination shows a high-riding prostate. Abdominal ultrasound shows a moderately distended bladder. X-rays of the pelvis show fractures of all four pubic rami. Which of the following is the most likely cause of this patient's symptoms?
- A. Tearing of the anterior urethra
- B. Rupture of the corpus cavernosum
- C. Tearing of the posterior urethra (Correct Answer)
- D. Tearing of the ureter
- E. Rupture of the bladder
Urinary bladder and urethra Explanation: ***Tearing of the posterior urethra***
- The combination of **pelvic fractures**, **blood at the urethral meatus**, inability to void despite a sensation to do so, and a **high-riding prostate** are classic signs of posterior urethral injury.
- The posterior urethra, particularly the membranous portion, is vulnerable to shear forces and tearing during severe pelvic trauma.
*Tearing of the anterior urethra*
- Anterior urethral injuries are typically associated with a **straddle injury** or direct trauma to the perineum, not necessarily pelvic fractures.
- While blood at the meatus can occur, the **high-riding prostate** and extensive pelvic fractures point away from an isolated anterior injury.
*Rupture of the corpus cavernosum*
- This is usually a result of "penile fracture" during sexual intercourse and presents with sudden pain, detumescence, and a characteristic "eggplant" deformity, which are not described here.
- It does not explain the inability to void, high-riding prostate, or association with pelvic fractures.
*Tearing of the ureter*
- Ureteral injuries are typically associated with penetrating trauma or iatrogenic injury during surgery; they rarely occur with blunt pelvic trauma of this nature.
- Symptoms would include flank pain, hematuria, or urine leakage into the retroperitoneum, not significant urethral bleeding or a high-riding prostate.
*Rupture of the bladder*
- Bladder rupture can be intra- or extraperitoneal and is often associated with pelvic fractures. However, it typically causes gross hematuria and often free fluid in the peritoneum (intraperitoneal rupture) or extravasation into the space of Retzius (extraperitoneal rupture).
- While a distended bladder is noted, the presence of **blood at the urethral meatus** and a **high-riding prostate** strongly implicate urethral injury rather than primarily bladder rupture.
Urinary bladder and urethra US Medical PG Question 8: A 28-year-old man is brought to the emergency department after being struck by a car an hour ago as he was crossing the street. He did not lose consciousness. He is complaining of pain in his right arm, forehead, and pelvis. He also has the urge to urinate, but has been unable to do so since the accident. He takes no medications. His temperature is 37.1°C (98.9°F), pulse is 72/min, respirations are 18/min, and blood pressure is 118/82 mm Hg. There are abrasions over his scalp and face and a 1x3 cm area of ecchymosis above his right eye. Abdominal examination shows suprapubic tenderness. There is a scant amount of blood at the urethral meatus. There is no cervical spinal tenderness. Musculoskeletal examination shows tenderness and ecchymosis over his right distal forearm. An x-ray of the pelvis shows a fracture of the pelvic ramus. A CT scan of the head and neck show no abnormalities. Which of the following is the best next step in the management of this patient?
- A. IV pyelogram
- B. Foley catheterization
- C. Contrast-enhanced CT scan of the abdomen
- D. Retrograde urethrogram (Correct Answer)
- E. Retroperitoneal ultrasound
Urinary bladder and urethra Explanation: ***Retrograde urethrogram***
- The presence of **blood at the urethral meatus**, **difficulty urinating**, and a **pelvic fracture** are highly suggestive of a **urethral injury**.
- A retrograde urethrogram is the appropriate diagnostic step to evaluate the integrity of the urethra before any attempt at catheterization.
*IV pyelogram*
- An IV pyelogram primarily assesses the **kidneys and ureters** for injury, which is not the immediate concern given the signs of urethral trauma.
- It would not provide the necessary detail to evaluate the **urethra** itself.
*Foley catheterization*
- Attempting Foley catheterization in the presence of suspected urethral injury is **contraindicated** as it can worsen the injury or create a false passage.
- The urethra needs to be assessed for integrity first to guide safe bladder drainage.
*Contrast-enhanced CT scan of the abdomen*
- While a CT scan of the abdomen might be performed later to assess other possible abdominal injuries, it is **not the primary imaging modality for urethral trauma**.
- A CT scan would not adequately visualize the **urethra** to rule out an injury.
*Retroperitoneal ultrasound*
- A retroperitoneal ultrasound evaluates for **fluid collections** or **organ injury** in the retroperitoneum, but it is not the most effective method for diagnosing **urethral tears**.
- It provides insufficient detail to assess the integrity of the urethra.
Urinary bladder and urethra US Medical PG Question 9: A 32-year-old woman comes to the physician because of a 2-week history of involuntary loss of urine. She loses small amounts of urine in the absence of an urge to urinate and for no apparent reason. She also reports that she has an intermittent urinary stream. Two years ago, she was diagnosed with multiple sclerosis. Current medications include glatiramer acetate and a multivitamin. She works as a librarian. She has 2 children who attend middle school. Vital signs are within normal limits. The abdomen is soft and nontender. Pelvic examination shows no abnormalities. Neurologic examination shows a slight hypesthesia in the lower left arm and absent abdominal reflex, but otherwise no abnormalities. Her post-void residual urine volume is 131 mL. Bladder size is normal. Which of the following is the most likely cause of the patient's urinary incontinence?
- A. Cognitive impairment
- B. Vesicovaginal fistula
- C. Bladder outlet obstruction
- D. Detrusor sphincter dyssynergia (Correct Answer)
- E. Impaired detrusor contractility
Urinary bladder and urethra Explanation: ***Detrusor sphincter dyssynergia***
- This condition is characterized by **involuntary contraction of the external urethral sphincter** during bladder contraction, leading to an **intermittent urinary stream** and incomplete bladder emptying, often seen in neurological conditions like **multiple sclerosis**.
- The **post-void residual urine volume of 131 mL** confirms incomplete bladder emptying, and the loss of small amounts of urine without urge suggests **overflow incontinence** due to chronic retention.
*Cognitive impairment*
- While cognitive impairment can cause urinary incontinence, typically it leads to **functional incontinence** where the patient is unable to recognize the need to urinate or is unable to reach the toilet in time.
- The patient's presentation of an **intermittent urinary stream** and high post-void residual is not characteristic of incontinence solely due to cognitive issues.
*Vesicovaginal fistula*
- A vesicovaginal fistula involves an **abnormal connection between the bladder and vagina**, causing **continuous leakage of urine** from the vagina, often following childbirth or surgery.
- The patient's symptoms of an **intermittent urinary stream** and neurological history are inconsistent with a fistula, and the pelvic exam was normal.
*Bladder outlet obstruction*
- Common causes include **benign prostatic hyperplasia** in men or **pelvic organ prolapse** in women, leading to difficulty emptying the bladder and symptoms like dribbling and straining.
- While it can cause incomplete emptying and overflow, without any evidence of prolapse on pelvic exam or other obstructive factors, and given her **multiple sclerosis**, a neurological cause like DSD is more likely.
*Impaired detrusor contractility*
- This condition results in the bladder being **unable to effectively contract** to empty urine, leading to incomplete emptying and overflow incontinence.
- While the patient has a high post-void residual volume, the presence of an **intermittent urinary stream** suggests that the detrusor *is* contracting, but facing resistance from a dyssynergic sphincter, rather than having impaired contractility itself.
Urinary bladder and urethra US Medical PG Question 10: A 19-year-old man is brought to the emergency department following a high-speed motor vehicle collision in which he was a restrained passenger. He complains of pelvic pain and urinary retention with overflow incontinence, along with associated lower extremity weakness. Examination shows perineal bruising and there is pain with manual compression of the pelvis. Injury to which of the following structures is most likely responsible for this patient's urinary incontinence?
- A. Ilioinguinal nerve
- B. Obturator nerve
- C. Genitofemoral nerve
- D. Pelvic splanchnic nerves (Correct Answer)
- E. Superior gluteal nerve
Urinary bladder and urethra Explanation: ***Pelvic splanchnic nerves***
- Urinary retention with overflow incontinence and lower extremity weakness following a pelvic trauma suggests damage to the **sacral spinal segments** or the **pelvic splanchnic nerves**.
- These nerves carry **parasympathetic fibers** that stimulate bladder contraction (detrusor muscle) and relaxation of the internal urethral sphincter, which are crucial for normal micturition.
*Ilioinguinal nerve*
- This nerve supplies sensory innervation to the **genitalia** and part of the inner thigh, and motor innervation to the internal oblique and transversus abdominis muscles.
- Damage to this nerve would primarily cause sensory deficits or abdominal muscle weakness, not urinary retention or lower extremity weakness.
*Obturator nerve*
- The obturator nerve primarily innervates the **adductor muscles of the thigh** and provides sensory innervation to the medial thigh.
- Injury would result in difficulty with hip adduction and sensory loss in the medial thigh, not bladder dysfunction or diffuse lower extremity weakness.
*Genitofemoral nerve*
- This nerve provides sensory innervation to the **anterior compartment of the thigh** and the external genitalia, and motor innervation to the cremaster muscle.
- Damage would typically manifest as altered sensation in these areas or an absent cremasteric reflex, without directly affecting bladder function.
*Superior gluteal nerve*
- The superior gluteal nerve innervates the **gluteus medius, gluteus minimus, and tensor fasciae latae muscles**, which are crucial for hip abduction and stabilization during walking.
- Injury would lead to a characteristic **Trendelenburg gait**, but would not directly cause urinary incontinence or retention.
More Urinary bladder and urethra US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.