Rectum and anal canal US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Rectum and anal canal. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Rectum and anal canal US Medical PG Question 1: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Rectum and anal canal Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
Rectum and anal canal US Medical PG Question 2: A 68-year-old man presents to his primary care physician complaining of a bulge in his scrotum that has enlarged over the past several months. He is found to have a right-sided inguinal hernia and undergoes elective hernia repair. At his first follow-up visit, he complains of a tingling sensation on his scrotum. Which of the following nerve roots communicates with the injured tissues?
- A. S1-S3
- B. L1-L2 (Correct Answer)
- C. S2-S4
- D. L4-L5
- E. L2-L3
Rectum and anal canal Explanation: ***L1-L2***
- The **ilioinguinal nerve** and **genitofemoral nerve**, which are commonly injured during inguinal hernia repair, arise from the **L1 and L2 spinal nerves**.
- These nerves provide sensory innervation to the **scrotum**, **inguinal region**, and **medial thigh**, explaining the patient's tingling sensation.
*S1-S3*
- These nerve roots typically contribute to the **sciatic nerve** and innervate the posterior thigh, leg, and foot, and are not directly involved in scrotal sensation relevant to an inguinal hernia repair.
- They also contribute to the **pudendal nerve**, which primarily supplies the perineum and external genitalia, but injury to this nerve is less common in routine inguinal hernia repair.
*S2-S4*
- These nerve roots primarily form the **pudendal nerve**, which innervates the **perineum** and external genitalia (including some scrotal sensation), but injury to these specific nerves is not a typical complication of routine inguinal hernia repair.
- They also contribute to the **pelvic splanchnic nerves**, controlling bladder and bowel function, which are unrelated to the described sensory deficit.
*L4-L5*
- These nerve roots primarily contribute to nerves supplying the **lower limb**, such as the **femoral nerve** and **sciatic nerve**, and do not directly innervate the scrotum.
- Injury to these roots would typically result in motor or sensory deficits of the **thigh and leg**, not isolated scrotal tingling.
*L2-L3*
- While L2 contributes to nerves supplying the inguinal region and scrotum (genitofemoral nerve), the **ilioinguinal nerve** originates from L1.
- The **lateral femoral cutaneous nerve**, which originates from L2-L3, innervates the **lateral thigh**, and its injury would cause tingling there, not in the scrotum.
Rectum and anal canal US Medical PG Question 3: A 45-year-old woman comes to the office with a 2-week history of rectal bleeding that occurs every day with her bowel movements. She denies any pain during defecation. Apart from this, she does not have any other complaints. Her past medical history is insignificant except for 5 normal vaginal deliveries. Her vitals are a heart rate of 72/min, a respiratory rate of 15/min, a temperature of 36.7°C (98.1°F), and a blood pressure of 115/85 mm Hg. On rectovaginal examination, there is a palpable, non-tender, prolapsed mass that can be pushed back by the examiner's finger into the anal sphincter. What is the most likely diagnosis?
- A. Rectal ulcer
- B. Anal fissure
- C. Hemorrhoids (Correct Answer)
- D. Proctitis
- E. Anorectal fistula
Rectum and anal canal Explanation: ***Hemorrhoids***
- The presentation of **painless rectal bleeding** with bowel movements and a **palpable, prolapsed, reducible mass** is classic for hemorrhoids, especially common in multiparous women.
- The absence of pain and the ability to reduce the prolapsed mass are key differentiating features from other perianal conditions.
*Rectal ulcer*
- Rectal ulcers typically present with **painful defecation** and may cause blood in the stool, but are not usually associated with a reducible prolapsed mass.
- They are often associated with other inflammatory conditions or trauma, which are not described here.
*Anal fissure*
- Anal fissures are characterized by **severe pain during and after defecation** due to a tear in the anal canal lining, and the bleeding is usually bright red and minimal.
- The primary symptom is pain, which this patient explicitly denies.
*Proctitis*
- Proctitis involves **inflammation of the rectal lining**, leading to symptoms like tenesmus, urgency, and bloody or purulent discharge, often with abdominal pain.
- It does not typically present with a palpable, prolapsed, reducible anal mass.
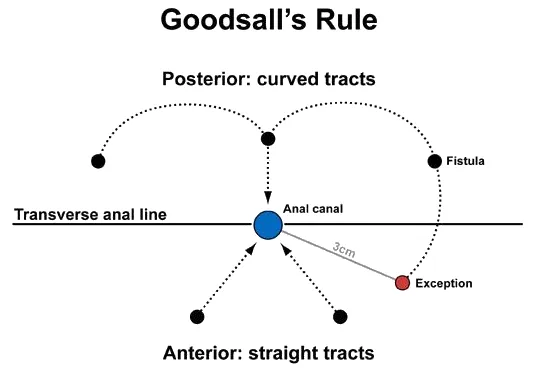
*Anorectal fistula*
- Anorectal fistulas are abnormal tracts between the anal canal or rectum and the perianal skin, usually causing **pain, swelling, and purulent discharge**.
- While bleeding can occur, the primary symptom is drainage, and they do not present as a reducible prolapsed mass.
Rectum and anal canal US Medical PG Question 4: A 65-year-old man comes to the physician because of progressive abdominal distension and swelling of his legs for 4 months. He has a history of ulcerative colitis. Physical examination shows jaundice. Abdominal examination shows shifting dullness and dilated veins in the periumbilical region. This patient's abdominal findings are most likely caused by increased blood flow in which of the following vessels?
- A. Hepatic vein
- B. Superior rectal vein
- C. Left gastric vein
- D. Superior epigastric vein (Correct Answer)
- E. Superior mesenteric vein
Rectum and anal canal Explanation: ***Superior epigastric vein***
- This patient presents with signs of **portal hypertension**, including **jaundice**, **abdominal distension** (ascites), and **dilated periumbilical veins** (caput medusae). The **superior epigastric vein** is part of the **portosystemic anastomoses**, specifically connecting the **portal system** (via the paraumbilical veins) to the **systemic circulation** (via the inferior epigastric vein).
- Increased blood flow through these anastomoses, particularly the **paraumbilical veins** that drain into the epigastric veins, causes the characteristic **caput medusae** observed as dilated veins around the umbilicus, due to the shunting of portal blood away from the obstructed liver.
*Hepatic vein*
- Obstruction or increased flow in the **hepatic veins** (e.g., Budd-Chiari syndrome) would typically cause acute liver congestion and ascites but would not cause prominent **caput medusae** from shunting through periumbilical veins.
- While it contributes to hepatic outflow, it is not directly involved in the formation of **caput medusae** through portosystemic shunting at the umbilical level.
*Superior rectal vein*
- Increased blood flow in the **superior rectal vein** would lead to **hemorrhoids** as part of portosystemic anastomoses at the rectoanal junction (portal system via inferior mesenteric vein to systemic via middle and inferior rectal veins).
- This does not explain the **periumbilical dilated veins** or **caput medusae** seen in the patient.
*Left gastric vein*
- The **left gastric vein** is a significant site of portosystemic anastomosis, connecting to the **azygos system**, and increased flow causes **esophageal varices**.
- While a crucial site of shunting in portal hypertension, it does not explain the **dilated periumbilical veins** observed.
*Superior mesenteric vein*
- The **superior mesenteric vein** is a major tributary of the **portal vein**; increased flow within it would lead to increased portal pressure but is not itself a site of portosystemic anastomosis that would result in **caput medusae**.
- Pathologies directly affecting the superior mesenteric vein (e.g., thrombosis) would lead to mesenteric ischemia or bowel congestion, rather than the specific periumbilical venous dilation.
Rectum and anal canal US Medical PG Question 5: A child is in the nursery one day after birth. A nurse notices a urine-like discharge being expressed through the umbilical stump. What two structures in the embryo are connected by the structure that failed to obliterate during the embryologic development of this child?
- A. Kidney - large bowel
- B. Liver - umbilical vein
- C. Bladder - small bowel
- D. Pulmonary artery - aorta
- E. Bladder - umbilicus (Correct Answer)
Rectum and anal canal Explanation: ***Bladder - umbilicus***
- A **urine-like discharge** from the umbilical stump indicates a **patent urachus**, which is the embryonic remnant of the allantois.
- The **allantois** (which becomes the urachus) is an embryonic structure that connects the **fetal bladder** to the **umbilicus** during development.
- Normally, the allantois obliterates after birth to form the **median umbilical ligament**, but failure to obliterate results in a patent urachus allowing urine to discharge through the umbilicus.
*Kidney - large bowel*
- These two structures are not directly connected by an obliterating embryonic structure relevant to urine discharge from an umbilical stump.
- The kidneys form urine, and the large bowel is part of the digestive tract, with no direct embryonic communication to the umbilicus for urine expression.
*Liver - umbilical vein*
- The umbilical vein connects the **placenta to the fetal liver** (and ductus venosus) to transport oxygenated blood, not urine.
- Failure of the umbilical vein to obliterate would result in a patent umbilical vein, typically presenting as a vascular anomaly, not urine discharge.
*Pulmonary artery - aorta*
- These structures are connected by the **ductus arteriosus** in fetal circulation, bypassing the pulmonary circulation.
- While important for fetal development, a patent ductus arteriosus (PDA) is a cardiovascular anomaly and would not manifest as urine discharge from the umbilical stump.
*Bladder - small bowel*
- While both structures are involved in waste elimination, there is no normal embryonic structure directly connecting the bladder and small bowel that obliterates to prevent urine discharge from the umbilicus.
- An abnormal connection between the bladder and bowel would typically involve a **fistula** and present with stool in urine or urine in stool, not umbilical discharge.
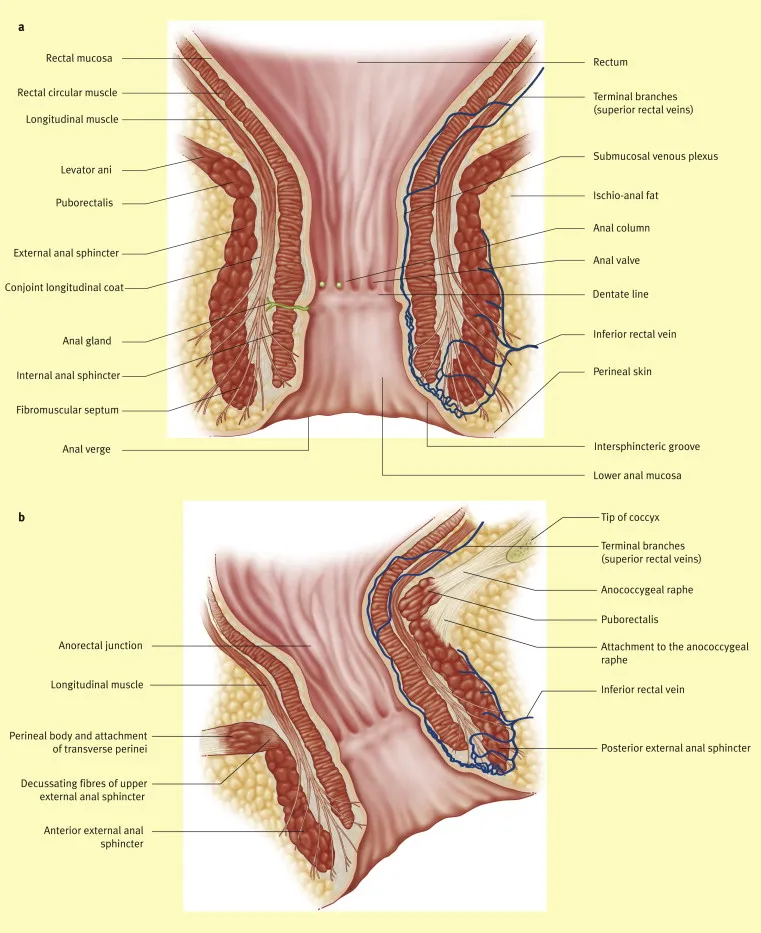
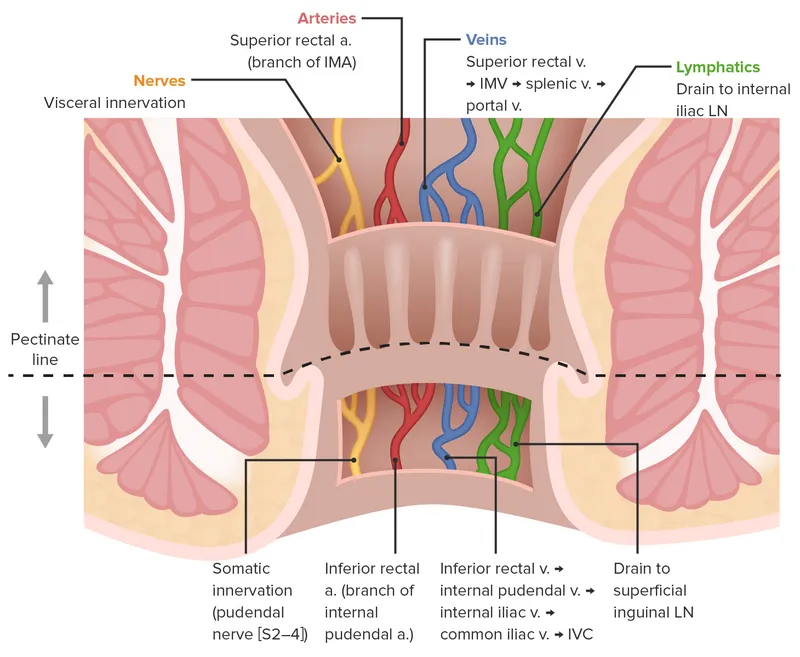
Rectum and anal canal US Medical PG Question 6: A 40-year-old woman comes to the physician because of a 2-week history of anal pain that occurs during defecation and lasts for several hours. She reports that she often strains during defecation and sees bright red blood on toilet paper after wiping. She typically has 3 bowel movements per week. Physical examination shows a longitudinal, perianal tear. This patient's symptoms are most likely caused by tissue injury in which of the following locations?
- A. Anterior midline of the anal canal, proximal to the pectinate line
- B. Posterior midline of the anal canal, distal to the pectinate line (Correct Answer)
- C. Posterior midline of the anal canal, proximal to the pectinate line
- D. Lateral aspect of the anal canal, distal to the pectinate line
- E. Anterior midline of the anal canal, distal to the pectinate line
Rectum and anal canal Explanation: ***Posterior midline of the anal canal, distal to the pectinate line***
- The described symptoms of severe **anal pain during and after defecation**, bright red blood on toilet paper, and straining with defecation are classic for an **anal fissure**.
- Anal fissures most commonly occur in the **posterior midline** of the anal canal, **distal to the pectinate (dentate) line**, due to reduced blood supply and increased mechanical stress in this area.
*Anterior midline of the anal canal, proximal to the pectinate line*
- Fissures can occur in the anterior midline but are less common than posterior midline fissures.
- Lesions proximal to the pectinate line are typically less painful as this area is innervated by the autonomic nervous system, unlike the highly sensitive somatic innervation distal to the pectinate line.
*Posterior midline of the anal canal, proximal to the pectinate line*
- While the posterior midline is a common location for fissures, involvement **proximal to the pectinate line** would likely present with less severe pain compared to the highly sensitive area distal to it.
- Lesions proximal to the pectinate line are more commonly internal hemorrhoids or proctitis, which present differently.
*Lateral aspect of the anal canal, distal to the pectinate line*
- Fissures in the lateral position are **atypical** and may suggest underlying conditions such as **Crohn's disease**, tuberculosis, or sexually transmitted infections, which are not indicated in this patient's presentation.
- The **midline** positions (anterior or posterior) are far more common for idiopathic anal fissures.
*Anterior midline of the anal canal, distal to the pectinate line*
- Though the anterior midline, distal to the pectinate line, is a possible location for fissures (especially in women), the **posterior midline** is the **most common** site due to anatomical factors.
- Given the classic presentation, the most frequent location is the most likely answer.
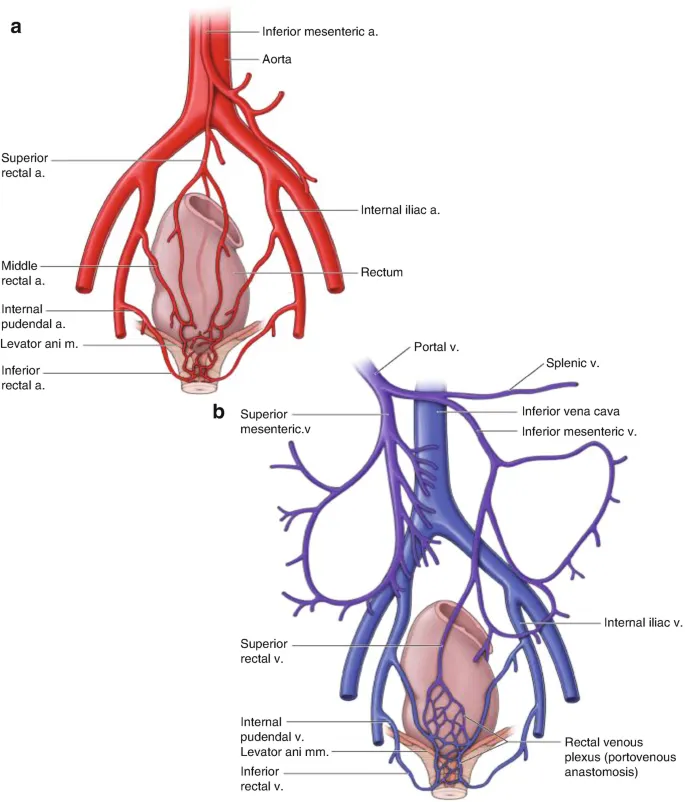
Rectum and anal canal US Medical PG Question 7: A 59-year-old truck driver presents to the emergency department after returning from his usual week-long trucking trip with excruciating pain around his anus. The patient admits to drinking beer when not working and notes that his meals usually consist of fast food. He has no allergies, takes no medications, and his vital signs are normal. On examination, he was found to have a tender lump on the right side of his anus that measures 1 cm in diameter. The lump is bluish and surrounded by edema. It is visible without the aid of an anoscope. It is soft and tender with palpation. The rest of the man’s history and physical examination are unremarkable. Which vein drains the vessels responsible for the formation of this lump?
- A. Inferior mesenteric
- B. Middle rectal
- C. Internal pudendal
- D. Superior rectal
- E. Inferior rectal (Correct Answer)
Rectum and anal canal Explanation: ***Inferior rectal***
- The description of a tender, bluish, edematous lump on the right side of the anus, visible externally, is characteristic of a **thrombosed external hemorrhoid**.
- **External hemorrhoids** develop in the inferior hemorrhoidal plexus, which is drained by the **inferior rectal veins**. These veins ultimately drain into the **internal iliac system**.
*Inferior mesenteric*
- The **inferior mesenteric vein** drains part of the large intestine, specifically the **descending colon, sigmoid colon, and superior rectum**.
- It drains into the **splenic vein** and is part of the **portal system**, not directly involved in draining external hemorrhoids.
*Middle rectal*
- The **middle rectal veins** drain the middle portion of the rectum and connect to the **internal iliac veins**.
- While they drain part of the rectum, they are primarily associated with the **internal hemorrhoidal plexus** (located proximal to the dentate line) or the rectal walls, not the external perianal area.
*Internal pudendal*
- The **internal pudendal vein** drains structures of the **perineum and external genitalia**.
- While it is located in the perineal region, it is not the primary drainage pathway for hemorrhoids, especially external ones which relate more to rectal venous plexuses.
*Superior rectal*
- The **superior rectal vein** drains the **superior part of the rectum** and the **internal hemorrhoidal plexus**.
- It is part of the **portal system**, draining into the **inferior mesenteric vein**, and is primarily associated with **internal hemorrhoids**, which are typically asymptomatic unless prolapsed or thrombosed and are located above the dentate line.
Rectum and anal canal US Medical PG Question 8: A 62-year-old female presents to her primary care physician complaining of bloody stool. She reports several episodes of bloody stools over the past two months as well as a feeling of a mass near her anus. She has one to two non-painful bowel movements per day. She has a history of alcohol abuse and hypertension. Anoscopy reveals engorged vessels. Which of the following vessels most likely drains blood from the affected region?
- A. Internal pudendal vein
- B. Left colic vein
- C. Inferior rectal vein (Correct Answer)
- D. Middle rectal vein
- E. Superior rectal vein
Rectum and anal canal Explanation: ***Inferior rectal vein***
- The patient's symptoms (bloody stool, anal mass, engorged vessels on anoscopy) are classic for **external hemorrhoids**.
- **External hemorrhoids** are distended veins located **below the dentate line** in the anal canal, which are drained by the **inferior rectal veins**.
- The inferior rectal veins drain into the **internal pudendal vein**, then to the **internal iliac vein** (part of the **systemic venous circulation**).
*Internal pudendal vein*
- The **internal pudendal vein** drains structures in the perineum and external genitalia, but it is not the **primary/direct drainage** for hemorrhoids.
- It receives blood from the inferior rectal veins but is one step removed from the hemorrhoidal plexus itself.
*Left colic vein*
- The **left colic vein** typically drains the distal transverse colon and descending colon.
- It is part of the **inferior mesenteric venous system** and is anatomically distant from the anorectal region, not involved in draining hemorrhoids.
*Middle rectal vein*
- The **middle rectal vein** drains the middle part of the rectum and connects both portal and systemic circulations.
- It drains the **muscularis layer** of the rectum but is not the primary drainage for the external hemorrhoidal plexus below the dentate line.
*Superior rectal vein*
- The **superior rectal vein** drains the upper part of the rectum and anal canal **above the dentate line**.
- Distention of these veins leads to **internal hemorrhoids**, which are typically painless unless prolapsed or thrombosed.
- It drains into the **inferior mesenteric vein** (part of the **portal venous circulation**).
Rectum and anal canal US Medical PG Question 9: A slipped disc at the level shown in the image would most likely involve which nerve root?
- A. L4
- B. L5 (Correct Answer)
- C. S1
- D. L3
- E. L2
Rectum and anal canal Explanation: ***L5***
- The image shows a **disc herniation** at the L4-L5 level. In cases of disc herniation, it is the **nerve root exiting below the level of the disc** that is typically compressed.
- For an L4-L5 disc herniation, the **L5 nerve root** is the one most commonly affected because it passes directly behind the L4 vertebral body and the L4-L5 disc before exiting the neural foramen at the L5-S1 level.
*L4*
- An L4 nerve root compression would typically occur with a disc herniation at the **L3-L4 level**. The L4 nerve root usually exits above the L4-L5 disc.
- While sometimes L4 nerve root can be involved in a massive central L4-L5 herniation, it is less common than L5 involvement for a typical posterolateral herniation at this level.
*S1*
- The S1 nerve root would be involved in a **disc herniation at the L5-S1 level**, as it exits below the L5-S1 disc.
- The disc herniation visible in the image is clearly above the L5-S1 intervertebral space.
*L3*
- Compression of the L3 nerve root usually results from a disc herniation at the **L2-L3 level**, which is higher than the level depicted in the image.
- The L3 nerve root is anatomically shielded from an L4-L5 disc herniation.
*L2*
- The L2 nerve root would be affected by a disc herniation at the **L1-L2 level**, which is significantly higher than the level shown in the image.
- L2 nerve root involvement would present with different clinical features (primarily hip flexion weakness and sensory changes in the anterior thigh).
Rectum and anal canal US Medical PG Question 10: An 11-year-old girl is brought in to her pediatrician by her parents due to developmental concerns. The patient developed normally throughout childhood, but she has not yet menstruated and has noticed that her voice is getting deeper. The patient has no other health issues. On exam, her temperature is 98.6°F (37.0°C), blood pressure is 110/68 mmHg, pulse is 74/min, and respirations are 12/min. The patient is noted to have Tanner stage I breasts and Tanner stage II pubic hair. On pelvic exam, the patient is noted to have a blind vagina with slight clitoromegaly as well as two palpable testes. Through laboratory workup, the patient is found to have 5-alpha-reductase deficiency. Which of the following anatomic structures are correctly matched homologues between male and female genitalia?
- A. Corpus spongiosum and the clitoral crura
- B. Scrotum and the labia majora (Correct Answer)
- C. Corpus spongiosum and the greater vestibular glands
- D. Corpus cavernosum of the penis and the vestibular bulbs
- E. Bulbourethral glands and the urethral/paraurethral glands
Rectum and anal canal Explanation: ***Scrotum and the labia majora***
- Both the **scrotum** in males and the **labia majora** in females develop from the **labioscrotal folds**.
- These structures serve to protect the underlying reproductive organs and are homologous due to their shared embryonic origin.
*Corpus spongiosum and the clitoral crura*
- The **corpus spongiosum** in males forms the glans penis and surrounds the urethra, while the **clitoral crura** are part of the corpus cavernosum homologues.
- The clitoral crura are homologous to the penile crura (part of the corpus cavernosum), not the corpus spongiosum.
*Corpus spongiosum and the greater vestibular glands*
- The **corpus spongiosum** is erectile tissue, while the **greater vestibular glands** (Bartholin's glands) are secretory glands.
- Greater vestibular glands are homologous to the **bulbourethral glands (Cowper's glands)** in males, which are also secretory.
*Corpus cavernosum of the penis and the vestibular bulbs*
- The **corpus cavernosum of the penis** is erectile tissue that forms the shaft of the penis and is homologous to the **corpus cavernosum of the clitoris (clitoral crura and body)**.
- The **vestibular bulbs** are masses of erectile tissue surrounding the vaginal opening, which are homologous to the **corpus spongiosum** in males, specifically the bulb of the penis.
*Bulbourethral glands and the urethral/paraurethral glands*
- The **bulbourethral glands** (Cowper's glands) are exocrine glands that secrete pre-ejaculate and are homologous to the **greater vestibular glands (Bartholin's glands)** in females.
- The **urethral/paraurethral glands (Skene's glands)** in females are homologous to the **prostate gland** in males.
More Rectum and anal canal US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.