Pudendal nerve and internal pudendal vessels US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pudendal nerve and internal pudendal vessels. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pudendal nerve and internal pudendal vessels US Medical PG Question 1: Seven hours after undergoing left hip arthroplasty for chronic hip pain, a 67-year-old woman reports a prickling sensation in her left anteromedial thigh and lower leg. Neurologic examination shows left leg strength 3/5 on hip flexion and 2/5 on knee extension. Patellar reflex is decreased on the left. Sensation to pinprick and light touch are decreased on the anteromedial left thigh as well as medial lower leg. Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Femoral nerve injury (Correct Answer)
- B. L5 radiculopathy
- C. Sural nerve injury
- D. S1 radiculopathy
- E. Fibular nerve injury
Pudendal nerve and internal pudendal vessels Explanation: ***Femoral nerve injury***
- The patient's symptoms—weakness in **hip flexion** (iliopsoas via femoral nerve) and **knee extension** (quadriceps via femoral nerve), decreased **patellar reflex** (femoral nerve), and sensory loss in the **anteromedial thigh** (femoral nerve) and **medial lower leg** (saphenous nerve, a branch of the femoral nerve)—are all consistent with femoral nerve dysfunction.
- **Hip arthroplasty procedures** can sometimes lead to iatrogenic femoral nerve damage due to retraction, compression, or direct injury during surgery, especially when positioning or using surgical instruments.
*L5 radiculopathy*
- L5 radiculopathy typically causes weakness in **foot dorsiflexion**, **eversion**, and **toe extension**, along with sensory loss over the **dorsum of the foot** and lateral lower leg, which does not match the patient's presentation.
- While it can cause hip abductor weakness, it would not explain the prominent **quadriceps weakness** and **decreased patellar reflex**.
*Sural nerve injury*
- The sural nerve provides sensation to the **posterolateral aspect of the lower leg** and lateral malleolus, and has no motor function to the hip or knee.
- Injury to this nerve would not account for the patient's **proximal weakness** or sensory loss in the anteromedial thigh.
*S1 radiculopathy*
- S1 radiculopathy typically leads to weakness in **plantarflexion**, **hip extension**, and an absent **Achilles reflex**, along with sensory loss over the lateral foot and sole.
- It would not explain the significant **quadriceps weakness**, **decreased patellar reflex**, or sensory changes in the anteromedial thigh.
*Fibular nerve injury*
- Fibular (peroneal) nerve injury primarily results in **foot drop** (weakness in dorsiflexion and eversion of the foot) and sensory loss over the **dorsum of the foot** and anterolateral lower leg.
- It does not affect hip flexion, knee extension, or the patellar reflex, nor does it cause sensory loss in the anteromedial thigh.
Pudendal nerve and internal pudendal vessels US Medical PG Question 2: A 19-year-old man is brought to the emergency department following a high-speed motor vehicle collision in which he was a restrained passenger. He complains of pelvic pain and urinary retention with overflow incontinence, along with associated lower extremity weakness. Examination shows perineal bruising and there is pain with manual compression of the pelvis. Injury to which of the following structures is most likely responsible for this patient's urinary incontinence?
- A. Ilioinguinal nerve
- B. Obturator nerve
- C. Genitofemoral nerve
- D. Pelvic splanchnic nerves (Correct Answer)
- E. Superior gluteal nerve
Pudendal nerve and internal pudendal vessels Explanation: ***Pelvic splanchnic nerves***
- Urinary retention with overflow incontinence and lower extremity weakness following a pelvic trauma suggests damage to the **sacral spinal segments** or the **pelvic splanchnic nerves**.
- These nerves carry **parasympathetic fibers** that stimulate bladder contraction (detrusor muscle) and relaxation of the internal urethral sphincter, which are crucial for normal micturition.
*Ilioinguinal nerve*
- This nerve supplies sensory innervation to the **genitalia** and part of the inner thigh, and motor innervation to the internal oblique and transversus abdominis muscles.
- Damage to this nerve would primarily cause sensory deficits or abdominal muscle weakness, not urinary retention or lower extremity weakness.
*Obturator nerve*
- The obturator nerve primarily innervates the **adductor muscles of the thigh** and provides sensory innervation to the medial thigh.
- Injury would result in difficulty with hip adduction and sensory loss in the medial thigh, not bladder dysfunction or diffuse lower extremity weakness.
*Genitofemoral nerve*
- This nerve provides sensory innervation to the **anterior compartment of the thigh** and the external genitalia, and motor innervation to the cremaster muscle.
- Damage would typically manifest as altered sensation in these areas or an absent cremasteric reflex, without directly affecting bladder function.
*Superior gluteal nerve*
- The superior gluteal nerve innervates the **gluteus medius, gluteus minimus, and tensor fasciae latae muscles**, which are crucial for hip abduction and stabilization during walking.
- Injury would lead to a characteristic **Trendelenburg gait**, but would not directly cause urinary incontinence or retention.
Pudendal nerve and internal pudendal vessels US Medical PG Question 3: A 58-year-old obese male has noticed the gradual development of a soft bulge on his right groin that has been present over the past year and occasionally becomes very tender. He notices that it comes out when he coughs and strains during bowel movements. He is able to push the bulge back in without issue. After examination, you realize that he has an inguinal hernia and recommend open repair with mesh placement. After surgery, the patient returns to clinic and complains of numbness and tingling in the upper part of the scrotum and base of the penis. What nerve was most likely injured during the procedure?
- A. Ilioinguinal nerve (Correct Answer)
- B. Iliohypogastric nerve
- C. Lateral femoral cutaneous nerve
- D. Obturator nerve
- E. Genitofemoral nerve
Pudendal nerve and internal pudendal vessels Explanation: **Ilioinguinal nerve**
- The **ilioinguinal nerve** supplies sensory innervation to the skin of the **scrotum** (or labia majora in females), the medial thigh, and the base of the penis.
- Injury to this nerve during an open inguinal hernia repair can cause **numbness and tingling** in these specific areas, consistent with the patient's symptoms.
*Iliohypogastric nerve*
- The **iliohypogastric nerve** primarily provides sensation to the skin over the **suprapubic region** and a small part of the buttock.
- Damage to this nerve would not typically result in numbness of the scrotum or base of the penis.
*Lateral femoral cutaneous nerve*
- This nerve is responsible for sensory innervation of the **lateral aspect of the thigh**.
- Its injury would lead to symptoms of numbness or pain on the lateral thigh (**meralgia paresthetica**), not the scrotum or penis.
*Obturator nerve*
- The **obturator nerve** is a motor nerve that innervates the **adductor muscles of the thigh** and provides sensory innervation to a small area of the medial thigh.
- Damage to this nerve would result in **adductor weakness** and sensory loss in the medial thigh, which does not match the patient's complaints.
*Genitofemoral nerve*
- The **genitofemoral nerve** has two branches: the genital branch (supplies the cremaster muscle and scrotal skin) and the femoral branch (supplies skin of the anterior thigh).
- While the genital branch does innervate the scrotum, injury to this nerve more commonly causes **cremasteric reflex loss** or pain radiating to the anterior thigh, and the described symptoms (base of penis) are more characteristic of ilioinguinal nerve involvement.
Pudendal nerve and internal pudendal vessels US Medical PG Question 4: A 71-year-old man with hypertension is taken to the emergency department after the sudden onset of stabbing abdominal pain that radiates to the back. He has smoked 1 pack of cigarettes daily for 20 years. His pulse is 120/min and thready, respirations are 18/min, and blood pressure is 82/54 mm Hg. Physical examination shows a periumbilical, pulsatile mass and abdominal bruit. There is epigastric tenderness. Which of the following is the most likely underlying mechanism of this patient's current condition?
- A. Mesenteric atherosclerosis
- B. Gastric mucosal ulceration
- C. Portal vein stasis
- D. Abdominal wall defect
- E. Aortic wall stress (Correct Answer)
Pudendal nerve and internal pudendal vessels Explanation: ***Aortic wall stress***
- The patient's presentation with **sudden onset of stabbing abdominal pain radiating to the back**, **hypotension** (BP 82/54 mm Hg), **tachycardia** (pulse 120/min), and a **pulsatile periumbilical mass** with an **abdominal bruit** is highly suggestive of a ruptured **abdominal aortic aneurysm (AAA)**.
- **Aortic wall stress**, often exacerbated by **hypertension** and **smoking**, leads to the progressive weakening and dilation of the aortic wall, eventually resulting in rupture.
*Mesenteric atherosclerosis*
- This condition typically causes **chronic abdominal pain** that is worse after eating (**postprandial angina**) due to inadequate blood supply to the intestines.
- It does not usually present with an acute, catastrophic event like **shock** and a **pulsatile mass**.
*Gastric mucosal ulceration*
- Ulceration can cause **epigastric pain**, but a ruptured ulcer would typically present with signs of **peritonitis** (rigidity, rebound tenderness) and potentially **hematemesis** or **melena**, which are not described.
- It would not cause a **pulsatile periumbilical mass** or the characteristic back pain of an AAA.
*Portal vein stasis*
- **Portal vein stasis** or **thrombosis** often leads to **portal hypertension**, **ascites**, and **gastrointestinal bleeding** from varices.
- It does not explain the acute onset of severe abdominal pain, hypotension, a pulsatile mass, or an abdominal bruit.
*Abdominal wall defect*
- An **abdominal wall defect**, such as a hernia, can cause localized pain and sometimes bowel obstruction.
- However, it does not account for the **hypotension**, **tachycardia**, **radiating pain to the back**, or the **pulsatile mass**, all of which point to a major vascular emergency.
Pudendal nerve and internal pudendal vessels US Medical PG Question 5: A 28-year-old woman, gravida 2, para 1, at 24 weeks gestation comes to the physician for a prenatal visit. She reports dull aching pain and paresthesia over her left hand during the last few weeks. The pain radiates to her shoulder and is worse at night. Her hand feels numb upon waking up in the morning. She has a sister who has multiple sclerosis. Her current medications include iron supplements and a multivitamin. Vital signs are within normal limits. When the wrist is passively held in full flexion, aggravation of paresthesia is perceived immediately. Which of the following is the most likely explanation for this patient's symptoms?
- A. Demyelinating disease of peripheral nerves
- B. Ulnar nerve compression
- C. Demyelinating disease of CNS
- D. Median nerve compression (Correct Answer)
- E. Cervical radiculopathy
Pudendal nerve and internal pudendal vessels Explanation: ***Median nerve compression***
- The patient's symptoms of **dull aching pain**, **paresthesia** in the hand radiating to the shoulder, and **nocturnal worsening** relieved by activity are classic for **carpal tunnel syndrome (CTS)**.
- The **Phalen's maneuver** (passive wrist flexion causing paresthesia) is a positive sign for CTS, indicating compression of the **median nerve** at the wrist, which is often exacerbated during pregnancy due to fluid retention and swelling.
*Demyelinating disease of peripheral nerves*
- While it can cause paresthesia, it typically presents with more diffuse and progressive sensory or motor deficits, and the specific pattern of hand symptoms and a positive Phalen's test are not characteristic.
- The symptoms are more localized and directly reproduced by a maneuver that specifically impinges the median nerve.
*Ulnar nerve compression*
- Compression of the ulnar nerve (e.g., at the **cubital tunnel**) would cause symptoms primarily in the **fourth and fifth digits**, which is not described here.
- A positive Phalen's maneuver specifically implicates the median nerve, not the ulnar nerve.
*Demyelinating disease of CNS*
- A demyelinating disease of the CNS, like **multiple sclerosis**, which runs in her family, would present with more widespread, fluctuating neurological deficits, often involving vision, balance, or motor weakness.
- The symptoms described are strictly localized to the hand and arm distribution, consistent with a peripheral nerve entrapment.
*Cervical radiculopathy*
- Cervical radiculopathy, caused by nerve root compression in the neck, would typically present with neck pain, and the pain and paresthesia would follow a **dermatomal pattern** corresponding to the affected nerve root.
- While it can radiate to the shoulder and arm, the positive Phalen's maneuver points specifically to a wrist-level median nerve compression, and the lack of neck pain makes it less likely.
Pudendal nerve and internal pudendal vessels US Medical PG Question 6: A 62-year-old female presents to her primary care physician complaining of bloody stool. She reports several episodes of bloody stools over the past two months as well as a feeling of a mass near her anus. She has one to two non-painful bowel movements per day. She has a history of alcohol abuse and hypertension. Anoscopy reveals engorged vessels. Which of the following vessels most likely drains blood from the affected region?
- A. Internal pudendal vein
- B. Left colic vein
- C. Inferior rectal vein (Correct Answer)
- D. Middle rectal vein
- E. Superior rectal vein
Pudendal nerve and internal pudendal vessels Explanation: ***Inferior rectal vein***
- The patient's symptoms (bloody stool, anal mass, engorged vessels on anoscopy) are classic for **external hemorrhoids**.
- **External hemorrhoids** are distended veins located **below the dentate line** in the anal canal, which are drained by the **inferior rectal veins**.
- The inferior rectal veins drain into the **internal pudendal vein**, then to the **internal iliac vein** (part of the **systemic venous circulation**).
*Internal pudendal vein*
- The **internal pudendal vein** drains structures in the perineum and external genitalia, but it is not the **primary/direct drainage** for hemorrhoids.
- It receives blood from the inferior rectal veins but is one step removed from the hemorrhoidal plexus itself.
*Left colic vein*
- The **left colic vein** typically drains the distal transverse colon and descending colon.
- It is part of the **inferior mesenteric venous system** and is anatomically distant from the anorectal region, not involved in draining hemorrhoids.
*Middle rectal vein*
- The **middle rectal vein** drains the middle part of the rectum and connects both portal and systemic circulations.
- It drains the **muscularis layer** of the rectum but is not the primary drainage for the external hemorrhoidal plexus below the dentate line.
*Superior rectal vein*
- The **superior rectal vein** drains the upper part of the rectum and anal canal **above the dentate line**.
- Distention of these veins leads to **internal hemorrhoids**, which are typically painless unless prolapsed or thrombosed.
- It drains into the **inferior mesenteric vein** (part of the **portal venous circulation**).
Pudendal nerve and internal pudendal vessels US Medical PG Question 7: A researcher is investigating the blood supply of the adrenal gland. While performing an autopsy on a patient who died from unrelated causes, he identifies a vessel that supplies oxygenated blood to the inferior aspect of the right adrenal gland. Which of the following vessels most likely gave rise to the vessel in question?
- A. Inferior phrenic artery
- B. Abdominal aorta
- C. Renal artery (Correct Answer)
- D. Superior mesenteric artery
- E. Common iliac artery
Pudendal nerve and internal pudendal vessels Explanation: ***Renal artery***
- The **inferior suprarenal artery**, which supplies the inferior part of the adrenal gland, typically arises from the **renal artery**.
- The adrenal glands receive a rich blood supply from three main arterial sources: superior, middle, and inferior suprarenal arteries.
*Inferior phrenic artery*
- The **superior suprarenal arteries** typically arise from the **inferior phrenic arteries** and supply the superior aspect of the adrenal glands.
- While critical for adrenal blood supply, they do not typically contribute to the inferior aspect directly.
*Abdominal aorta*
- The **middle suprarenal artery** usually arises directly from the **abdominal aorta**.
- This vessel supplies the central part of the adrenal gland, but not primarily the inferior aspect.
*Superior mesenteric artery*
- The **superior mesenteric artery** primarily supplies structures of the midgut (e.g., small intestine, ascending colon) and does not typically give rise to vessels supplying the adrenal glands.
- It is located inferior to the origin of the renal arteries and the adrenal glands.
*Common iliac artery*
- The **common iliac arteries** supply the lower limbs and pelvic organs, originating from the abdominal aorta bifurcation.
- These arteries are located much too far inferior to supply the adrenal glands, which are retroperitoneal structures in the upper abdomen.
Pudendal nerve and internal pudendal vessels US Medical PG Question 8: During a physical examination, a physician tests the strength of hip adduction against resistance. Which of the following nerves innervates the primary muscles responsible for this action?
- A. Sciatic nerve
- B. Superior gluteal nerve
- C. Femoral nerve
- D. Obturator nerve (Correct Answer)
Pudendal nerve and internal pudendal vessels Explanation: ***Obturator nerve***
- The **obturator nerve** primarily innervates the **adductor muscles** of the thigh, including the adductor longus, adductor brevis, adductor magnus (adductor part), gracilis, and pectineus (variable innervation).
- These muscles are responsible for **adducting the hip**, which is the action tested when a physician checks hip adduction strength against resistance.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (semitendinosus, semimembranosus, biceps femoris) and all muscles below the knee.
- It does not significantly contribute to the innervation of the primary hip adductors.
*Superior gluteal nerve*
- The **superior gluteal nerve** mainly innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae** muscles.
- These muscles are primarily involved in **hip abduction** and medial rotation, not adduction.
*Femoral nerve*
- The **femoral nerve** innervates the **quadriceps femoris muscles** (rectus femoris, vastus lateralis, vastus medialis, vastus intermedius) and the sartorius.
- Its primary actions are **knee extension** and hip flexion, with no direct role in hip adduction.
Pudendal nerve and internal pudendal vessels US Medical PG Question 9: A 26-year-old woman comes to the physician because of painful paresthesias in her foot. Examination shows decreased sensation in the first interdigital space and a hallux valgus deformity. This patient's paresthesias are most likely caused by compression of which of the following nerves?
- A. Saphenous nerve
- B. Sural nerve
- C. Superficial peroneal nerve
- D. Medial plantar nerve
- E. Deep peroneal nerve (Correct Answer)
Pudendal nerve and internal pudendal vessels Explanation: ***Deep peroneal nerve***
- The **deep peroneal nerve** provides sensation to the **first interdigital space** of the foot, and its compression would explain the described paresthesias.
- A **hallux valgus deformity** can alter foot mechanics and contribute to compression of this nerve.
*Saphenous nerve*
- The **saphenous nerve** provides sensory innervation to the **medial aspect of the lower leg and foot**, not specifically the interdigital spaces.
- Its compression is typically associated with pain or paresthesias in the medial calf or ankle.
*Sural nerve*
- The **sural nerve** provides sensation to the **lateral aspect of the foot and ankle**.
- Compression of this nerve would cause symptoms in a different distribution than described.
*Superficial peroneal nerve*
- The **superficial peroneal nerve** innervates the **dorsum of the foot**, excluding the first interdigital space and the area between the first and second toes.
- Compression would typically result in sensory changes over the top of the foot.
*Medial plantar nerve*
- The **medial plantar nerve** provides sensation to the **medial two-thirds of the plantar foot** and the **first 3.5 toes** on the plantar surface, not the dorsal interdigital space.
- Compression is often associated with symptoms similar to tarsal tunnel syndrome.
Pudendal nerve and internal pudendal vessels US Medical PG Question 10: A 59-year-old truck driver presents to the emergency department after returning from his usual week-long trucking trip with excruciating pain around his anus. The patient admits to drinking beer when not working and notes that his meals usually consist of fast food. He has no allergies, takes no medications, and his vital signs are normal. On examination, he was found to have a tender lump on the right side of his anus that measures 1 cm in diameter. The lump is bluish and surrounded by edema. It is visible without the aid of an anoscope. It is soft and tender with palpation. The rest of the man’s history and physical examination are unremarkable. Which vein drains the vessels responsible for the formation of this lump?
- A. Inferior mesenteric
- B. Middle rectal
- C. Internal pudendal
- D. Superior rectal
- E. Inferior rectal (Correct Answer)
Pudendal nerve and internal pudendal vessels Explanation: ***Inferior rectal***
- The description of a tender, bluish, edematous lump on the right side of the anus, visible externally, is characteristic of a **thrombosed external hemorrhoid**.
- **External hemorrhoids** develop in the inferior hemorrhoidal plexus, which is drained by the **inferior rectal veins**. These veins ultimately drain into the **internal iliac system**.
*Inferior mesenteric*
- The **inferior mesenteric vein** drains part of the large intestine, specifically the **descending colon, sigmoid colon, and superior rectum**.
- It drains into the **splenic vein** and is part of the **portal system**, not directly involved in draining external hemorrhoids.
*Middle rectal*
- The **middle rectal veins** drain the middle portion of the rectum and connect to the **internal iliac veins**.
- While they drain part of the rectum, they are primarily associated with the **internal hemorrhoidal plexus** (located proximal to the dentate line) or the rectal walls, not the external perianal area.
*Internal pudendal*
- The **internal pudendal vein** drains structures of the **perineum and external genitalia**.
- While it is located in the perineal region, it is not the primary drainage pathway for hemorrhoids, especially external ones which relate more to rectal venous plexuses.
*Superior rectal*
- The **superior rectal vein** drains the **superior part of the rectum** and the **internal hemorrhoidal plexus**.
- It is part of the **portal system**, draining into the **inferior mesenteric vein**, and is primarily associated with **internal hemorrhoids**, which are typically asymptomatic unless prolapsed or thrombosed and are located above the dentate line.
More Pudendal nerve and internal pudendal vessels US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
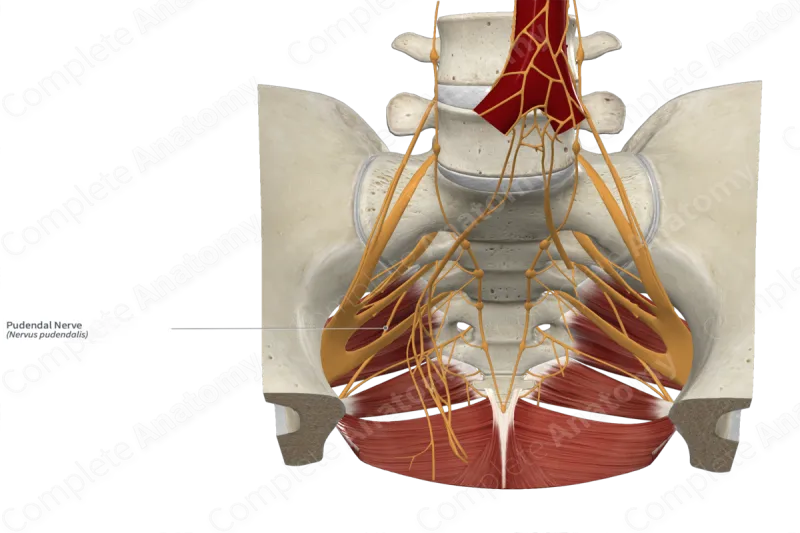
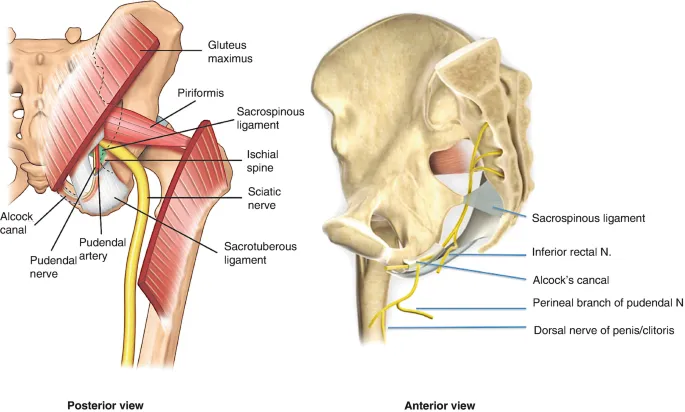
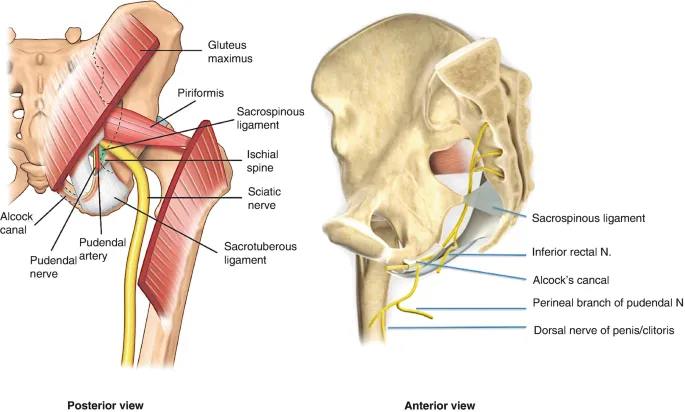
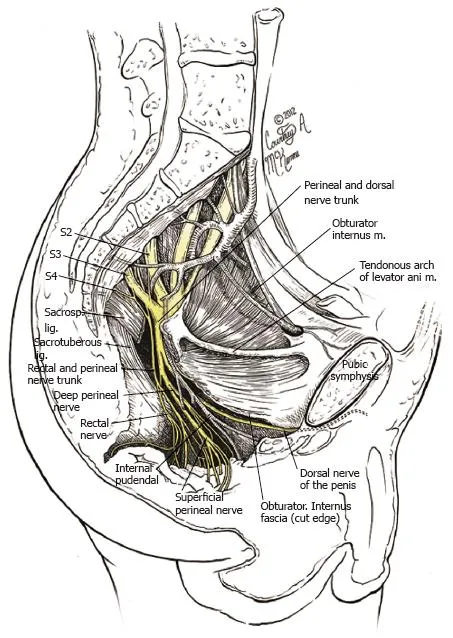 and its contents: pudendal nerve, artery, and vein)
and its contents: pudendal nerve, artery, and vein)