Perineum and ischioanal fossa US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Perineum and ischioanal fossa. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Perineum and ischioanal fossa US Medical PG Question 1: A 32-year-old woman presents to the office with complaints of intense anal pain every time she has a bowel movement. The pain has been present for the past 4 weeks, and it is dull and throbbing in nature. It is associated with mild bright red bleeding from the rectum that is aggravated during defecation. She has no relevant past medical history. When asked about her sexual history, she reports practicing anal intercourse. The vital signs include heart rate 98/min, respiratory rate 16/min, temperature 37.6°C (99.7°F), and blood pressure 110/66 mm Hg. On physical examination, the anal sphincter tone is markedly increased, and it's impossible to introduce the finger due to severe pain. What is the most likely diagnosis?
- A. Local anal trauma (Correct Answer)
- B. Rectal prolapse and paradoxical contraction of the puborectalis muscle
- C. Inflammatory bowel disease
- D. Anorectal abscess
- E. Hemorrhoidal disease
Perineum and ischioanal fossa Explanation: ***Local anal trauma***
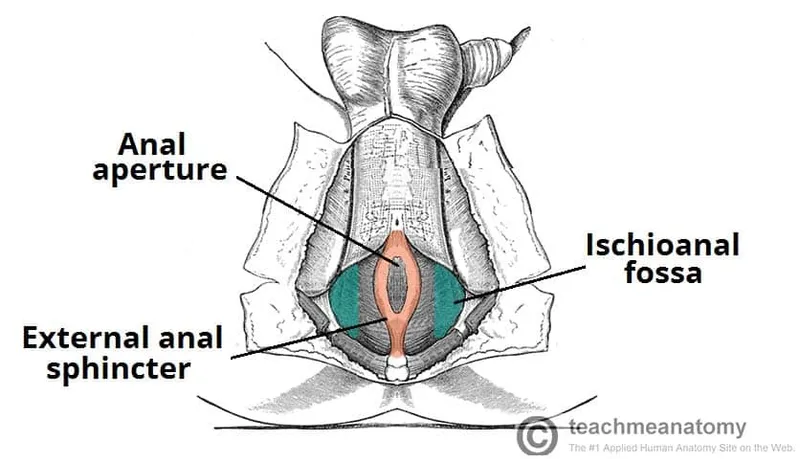
- The patient's history of **anal intercourse**, severe **anal pain** during bowel movements, **bright red bleeding**, and a markedly **increased anal sphincter tone** with inability to perform a DRE due to pain are highly indicative of an **anal fissure** caused by local trauma.
- The dull, throbbing pain suggests associated spasm of the internal anal sphincter, a common complication of anal fissures.
*Rectal prolapse and paradoxical contraction of the puborectalis muscle*
- **Rectal prolapse** typically presents with a sensation of a mass protruding from the anus and difficulty with bowel movements, not usually intense, sharp pain and bright red bleeding.
- **Paradoxical contraction of the puborectalis muscle** (anismus) causes difficult defecation and straining but is not typically associated with acute, severe pain and bright red bleeding as primary symptoms.
*Inflammatory bowel disease*
- While IBD can cause rectal bleeding and anal pain (e.g., in Crohn's disease with perianal fistulas or fissures), the presentation here is acute and highly suggestive of a mechanical cause, without other systemic symptoms of IBD like diarrhea, weight loss, or abdominal pain.
- The **isolated acute anal pain** and bleeding linked to defecation and anal intercourse are less typical for an initial presentation of IBD without other associated symptoms.
*Anorectal abscess*
- Anorectal abscesses typically present with severe, constant, throbbing **perianal pain** that is often worse when sitting, and may be accompanied by fever, chills, and localized swelling or erythema, which are not described here.
- While an abscess might cause throbbing pain, the association with **defecation-induced pain** and **bright red bleeding** from a visible source like an anal fissure is less characteristic.
*Hemorrhoidal disease*
- Hemorrhoids often cause **painless bright red bleeding** during defecation or can cause itching and discomfort. **Thrombosed external hemorrhoids** can cause acute, severe pain but usually present with a palpable, tender nodule.
- The description of **intense, sharp anal pain** during bowel movements, increased sphincter tone, and inability to perform a digital rectal exam are more consistent with an anal fissure than typical hemorrhoidal disease.
Perineum and ischioanal fossa US Medical PG Question 2: A 68-year-old man presents to his primary care physician complaining of a bulge in his scrotum that has enlarged over the past several months. He is found to have a right-sided inguinal hernia and undergoes elective hernia repair. At his first follow-up visit, he complains of a tingling sensation on his scrotum. Which of the following nerve roots communicates with the injured tissues?
- A. S1-S3
- B. L1-L2 (Correct Answer)
- C. S2-S4
- D. L4-L5
- E. L2-L3
Perineum and ischioanal fossa Explanation: ***L1-L2***
- The **ilioinguinal nerve** and **genitofemoral nerve**, which are commonly injured during inguinal hernia repair, arise from the **L1 and L2 spinal nerves**.
- These nerves provide sensory innervation to the **scrotum**, **inguinal region**, and **medial thigh**, explaining the patient's tingling sensation.
*S1-S3*
- These nerve roots typically contribute to the **sciatic nerve** and innervate the posterior thigh, leg, and foot, and are not directly involved in scrotal sensation relevant to an inguinal hernia repair.
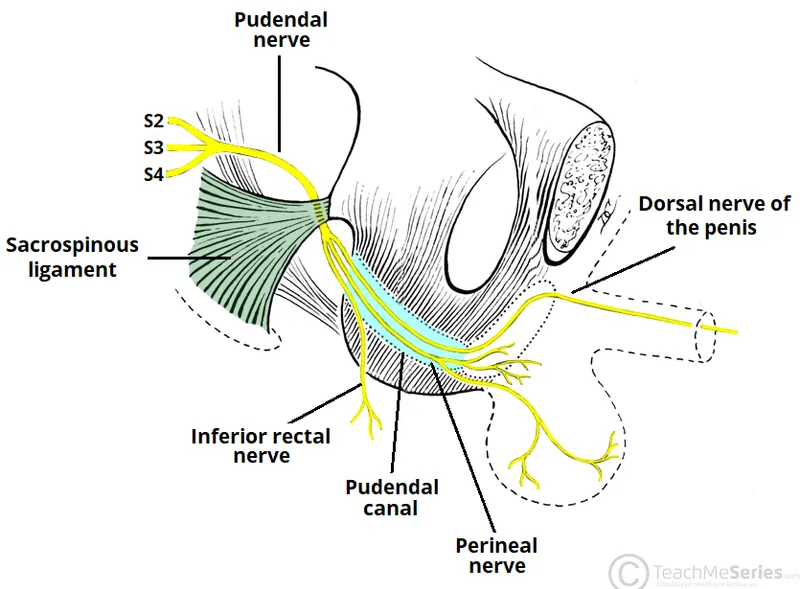
- They also contribute to the **pudendal nerve**, which primarily supplies the perineum and external genitalia, but injury to this nerve is less common in routine inguinal hernia repair.
*S2-S4*
- These nerve roots primarily form the **pudendal nerve**, which innervates the **perineum** and external genitalia (including some scrotal sensation), but injury to these specific nerves is not a typical complication of routine inguinal hernia repair.
- They also contribute to the **pelvic splanchnic nerves**, controlling bladder and bowel function, which are unrelated to the described sensory deficit.
*L4-L5*
- These nerve roots primarily contribute to nerves supplying the **lower limb**, such as the **femoral nerve** and **sciatic nerve**, and do not directly innervate the scrotum.
- Injury to these roots would typically result in motor or sensory deficits of the **thigh and leg**, not isolated scrotal tingling.
*L2-L3*
- While L2 contributes to nerves supplying the inguinal region and scrotum (genitofemoral nerve), the **ilioinguinal nerve** originates from L1.
- The **lateral femoral cutaneous nerve**, which originates from L2-L3, innervates the **lateral thigh**, and its injury would cause tingling there, not in the scrotum.
Perineum and ischioanal fossa US Medical PG Question 3: A 59-year-old truck driver presents to the emergency department after returning from his usual week-long trucking trip with excruciating pain around his anus. The patient admits to drinking beer when not working and notes that his meals usually consist of fast food. He has no allergies, takes no medications, and his vital signs are normal. On examination, he was found to have a tender lump on the right side of his anus that measures 1 cm in diameter. The lump is bluish and surrounded by edema. It is visible without the aid of an anoscope. It is soft and tender with palpation. The rest of the man’s history and physical examination are unremarkable. Which vein drains the vessels responsible for the formation of this lump?
- A. Inferior mesenteric
- B. Middle rectal
- C. Internal pudendal
- D. Superior rectal
- E. Inferior rectal (Correct Answer)
Perineum and ischioanal fossa Explanation: ***Inferior rectal***
- The description of a tender, bluish, edematous lump on the right side of the anus, visible externally, is characteristic of a **thrombosed external hemorrhoid**.
- **External hemorrhoids** develop in the inferior hemorrhoidal plexus, which is drained by the **inferior rectal veins**. These veins ultimately drain into the **internal iliac system**.
*Inferior mesenteric*
- The **inferior mesenteric vein** drains part of the large intestine, specifically the **descending colon, sigmoid colon, and superior rectum**.
- It drains into the **splenic vein** and is part of the **portal system**, not directly involved in draining external hemorrhoids.
*Middle rectal*
- The **middle rectal veins** drain the middle portion of the rectum and connect to the **internal iliac veins**.
- While they drain part of the rectum, they are primarily associated with the **internal hemorrhoidal plexus** (located proximal to the dentate line) or the rectal walls, not the external perianal area.
*Internal pudendal*
- The **internal pudendal vein** drains structures of the **perineum and external genitalia**.
- While it is located in the perineal region, it is not the primary drainage pathway for hemorrhoids, especially external ones which relate more to rectal venous plexuses.
*Superior rectal*
- The **superior rectal vein** drains the **superior part of the rectum** and the **internal hemorrhoidal plexus**.
- It is part of the **portal system**, draining into the **inferior mesenteric vein**, and is primarily associated with **internal hemorrhoids**, which are typically asymptomatic unless prolapsed or thrombosed and are located above the dentate line.
Perineum and ischioanal fossa US Medical PG Question 4: A 47-year-old man is brought to the emergency department 1 hour after injuring his genital area when he fell astride his backyard fence. He was trimming a tree from the fence when he lost his balance. His vital signs are within normal limits. Examination shows blood at the urethral meatus, perineal ecchymoses, and a scrotal hematoma. An x-ray of the pelvis shows swelling of the soft tissue but no other abnormalities. Which part of the urinary tract is most likely damaged in this patient?
- A. Penile urethra
- B. Bulbous urethra (Correct Answer)
- C. Anterior bladder wall
- D. Prostatic urethra
- E. Membranous urethra
Perineum and ischioanal fossa Explanation: ***Bulbous urethra***
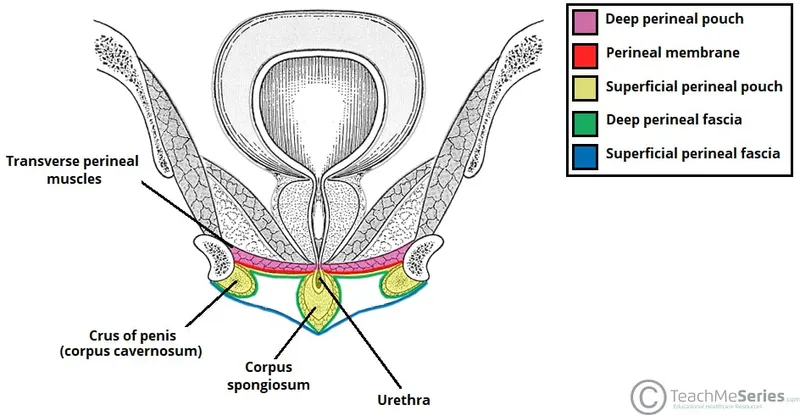
- Straddle injuries (falling astride an object) cause **direct compression of the bulbous urethra** against the inferior pubic ramus
- Classic triad: **blood at urethral meatus, perineal ecchymoses, and scrotal/perineal hematoma** (butterfly pattern)
- The bulbous urethra is part of the **anterior urethra** and is most vulnerable in blunt perineal trauma
- This is a **Buck's fascia injury** with characteristic perineal and scrotal swelling
*Penile urethra*
- More distal portion of anterior urethra within the penis
- Typically injured by **direct penile trauma** (penile fracture, penetrating injury, instrumentation)
- Would not produce the perineal ecchymoses and scrotal hematoma seen in this case
*Membranous urethra*
- Part of **posterior urethra** located within the urogenital diaphragm
- Typically injured with **pelvic fractures** (pubic rami fractures), which are absent in this case
- Would present with high-riding prostate on rectal exam and inability to void
*Prostatic urethra*
- Most proximal portion of posterior urethra, well-protected within the prostate
- Injured in **severe pelvic trauma** with disruption of puboprostatic ligaments
- Also associated with pelvic fractures, not straddle injuries
*Anterior bladder wall*
- Requires **pelvic fracture** or penetrating trauma
- Would present with **gross hematuria** and suprapubic pain/tenderness
- Blood at meatus is not typical; more likely to have abdominal distension and peritoneal signs
Perineum and ischioanal fossa US Medical PG Question 5: A 47-year-old woman comes to the physician because of involuntary leakage of urine for the past 4 months, which she has experienced when bicycling to work and when laughing. She has not had any dysuria or urinary urgency. She has 4 children that were all delivered vaginally. She is otherwise healthy and takes no medications. The muscles most likely affected by this patient's condition receive efferent innervation from which of the following structures?
- A. S3–S4 nerve roots (Correct Answer)
- B. Obturator nerve
- C. Superior hypogastric plexus
- D. Superior gluteal nerve
- E. S1-S2 nerve roots
Perineum and ischioanal fossa Explanation: ***S3–S4 nerve roots***
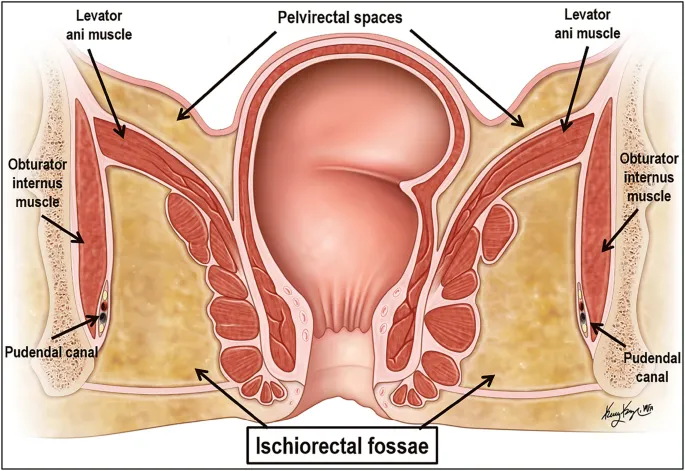
- The patient's symptoms of **involuntary urine leakage** during physical activity (**stress incontinence**) and a history of multiple vaginal deliveries strongly suggest **pelvic floor muscle weakness**.
- The **levator ani muscles**, which are crucial for maintaining urinary continence, receive their primary innervation from the **pudendal nerve**, which originates from the **S2-S4 spinal nerves** (though contributions from S3-S4 are often highlighted for pelvic floor efferent innervation).
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles of the thigh** (e.g., adductor longus, magnus, brevis, gracilis), as well as the obturator externus muscle.
- It does not significantly contribute to the innervation of the **pelvic floor muscles** responsible for urinary continence.
*Superior hypogastric plexus*
- The **superior hypogastric plexus** is part of the **autonomic nervous system** and primarily carries **sympathetic innervation** to the pelvic organs.
- While it plays a role in bladder function (e.g., bladder relaxation and internal urethral sphincter contraction), it does not provide **somatic efferent innervation** to the skeletal muscles of the pelvic floor.
*Superior gluteal nerve*
- The **superior gluteal nerve** innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae muscles**.
- These muscles are involved in **hip abduction** and **medial rotation** and are not directly involved in maintaining urinary continence through the pelvic floor.
*S1-S2 nerve roots*
- While the **S1-S2 nerve roots** contribute to the innervation of various lower limb muscles and sensory pathways, their primary efferent contributions related to pelvic floor continence are not as direct as S3-S4.
- The **pudendal nerve**, critical for pelvic floor muscle function, originates predominantly from **S2-S4**, with S3-S4 being particularly important for the motor components.
Perineum and ischioanal fossa US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Perineum and ischioanal fossa Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Perineum and ischioanal fossa US Medical PG Question 7: During a physical examination, a physician tests the strength of hip adduction against resistance. Which of the following nerves innervates the primary muscles responsible for this action?
- A. Sciatic nerve
- B. Superior gluteal nerve
- C. Femoral nerve
- D. Obturator nerve (Correct Answer)
Perineum and ischioanal fossa Explanation: ***Obturator nerve***
- The **obturator nerve** primarily innervates the **adductor muscles** of the thigh, including the adductor longus, adductor brevis, adductor magnus (adductor part), gracilis, and pectineus (variable innervation).
- These muscles are responsible for **adducting the hip**, which is the action tested when a physician checks hip adduction strength against resistance.
*Sciatic nerve*
- The **sciatic nerve** innervates the **hamstring muscles** (semitendinosus, semimembranosus, biceps femoris) and all muscles below the knee.
- It does not significantly contribute to the innervation of the primary hip adductors.
*Superior gluteal nerve*
- The **superior gluteal nerve** mainly innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae** muscles.
- These muscles are primarily involved in **hip abduction** and medial rotation, not adduction.
*Femoral nerve*
- The **femoral nerve** innervates the **quadriceps femoris muscles** (rectus femoris, vastus lateralis, vastus medialis, vastus intermedius) and the sartorius.
- Its primary actions are **knee extension** and hip flexion, with no direct role in hip adduction.
Perineum and ischioanal fossa US Medical PG Question 8: A male newborn is born at 37 weeks' gestation after spontaneous vaginal delivery. The mother had no prenatal care. Physical examination shows a urethral opening on the dorsal aspect of the penis, 4 mm proximal to the glans. There is a 3-cm defect in the midline abdominal wall superior to the pubic symphysis with exposure of moist, erythematous mucosa. Which of the following is the most likely underlying cause of this patient's findings?
- A. Abnormal development of the gubernaculum
- B. Persistence of the urogenital membrane
- C. Failed fusion of the urethral folds
- D. Incomplete union of the labioscrotal swellings
- E. Malpositioning of the genital tubercle (Correct Answer)
Perineum and ischioanal fossa Explanation: ***Malpositioning of the genital tubercle***
- This condition describes **epispadias** (urethral opening on the dorsal aspect) and **bladder exstrophy** (abdominal wall defect with exposed bladder mucosa), which are frequently co-occurring and caused by a **ventral displacement of the genital tubercle**.
- A defect in the **abdominal wall closure** allows the bladder to remain exposed, and the abnormal positioning of the genital tubercle leads to an improperly formed urethra.
*Abnormal development of the gubernaculum*
- The gubernaculum is crucial for **testicular descent**; abnormal development would typically lead to **cryptorchidism** (undescended testes).
- It does not explain the urethral opening on the dorsal penis or the abdominal wall defect.
*Persistence of the urogenital membrane*
- Persistent urogenital membrane typically results in conditions like an **imperforate hymen** in females or **urogenital sinus anomalies**, but not epispadias or bladder exstrophy.
- This membrane normally ruptures, creating the definitive openings for the urethra and vagina.
*Failed fusion of the urethral folds*
- Failed fusion of the urethral folds in males can lead to **hypospadias**, where the urethral opening is on the **ventral** aspect of the penis.
- It does not account for the **dorsal urethral opening (epispadias)** described or the associated bladder exstrophy.
*Incomplete union of the labioscrotal swellings*
- Incomplete union of the labioscrotal swellings in males results in **bifid scrotum** or **hypospadias**.
- This doesn't explain the characteristic dorsal urethral defect of epispadias or the large abdominal wall defect associated with bladder exstrophy.
Perineum and ischioanal fossa US Medical PG Question 9: A 24-year-old woman comes to the physician for an annual routine examination. Menses occur at regular 28-day intervals and last for 4 days with normal flow. Her last menstrual period was 3 weeks ago. She is sexually active with one male partner and they use condoms consistently. The patient is 160 cm (5 ft 3 in) tall and weighs 72 kg (150 lb); BMI is 28.1 kg/m2. She feels well. Pelvic examination shows a smooth, mobile right adnexal mass. A subsequent ultrasound of the pelvis shows a single, 2-cm large, round, hypoechoic mass with a thin, smooth wall in the right ovary. The mass has posterior wall enhancement, and there are no signs of blood flow or septae within the mass. Which of the following is the most appropriate next step in management?
- A. Diagnostic laparoscopy
- B. CT scan of the pelvis
- C. Oral contraceptive
- D. CA-125 level
- E. Follow-up examination (Correct Answer)
Perineum and ischioanal fossa Explanation: ***Follow-up examination***
- The ultrasound findings of a **small (2-cm)**, **simple (hypoechoic, thin-walled, no septations, no blood flow)** adnexal cyst in a **premenopausal woman** are characteristic of a functional ovarian cyst.
- Functional cysts are typically benign and resolve spontaneously, making **expectant management with follow-up** the most appropriate initial step.
*Diagnostic laparoscopy*
- This is an **invasive surgical procedure** indicated for suspicious or persistent ovarian masses that require histological evaluation or removal.
- It is **not warranted for a small, simple cyst** with benign features found incidentally in an asymptomatic, premenopausal woman.
*CT scan of the pelvis*
- A CT scan provides additional imaging but exposes the patient to **radiation** and is generally reserved for masses with **complex features** or when evaluating for metastasis.
- It is **not necessary for a simple cyst** that has already been well-characterized by ultrasound.
*Oral contraceptive*
- While oral contraceptives can **suppress ovulation** and potentially prevent the formation of new functional cysts, they generally do **not hasten the resolution of existing cysts**.
- They are sometimes used in cases of recurrent functional cysts but are not the primary management for an initial, asymptomatic simple cyst.
*CA-125 level*
- **CA-125** is a tumor marker primarily used for monitoring ovarian cancer, especially in **postmenopausal women** or those with highly suspicious masses.
- Its levels can be elevated in various benign conditions, and it is **not indicated for a small, simple cyst** in a premenopausal woman, where the risk of malignancy is very low.
Perineum and ischioanal fossa US Medical PG Question 10: A 62-year-old female presents to her primary care physician complaining of bloody stool. She reports several episodes of bloody stools over the past two months as well as a feeling of a mass near her anus. She has one to two non-painful bowel movements per day. She has a history of alcohol abuse and hypertension. Anoscopy reveals engorged vessels. Which of the following vessels most likely drains blood from the affected region?
- A. Internal pudendal vein
- B. Left colic vein
- C. Inferior rectal vein (Correct Answer)
- D. Middle rectal vein
- E. Superior rectal vein
Perineum and ischioanal fossa Explanation: ***Inferior rectal vein***
- The patient's symptoms (bloody stool, anal mass, engorged vessels on anoscopy) are classic for **external hemorrhoids**.
- **External hemorrhoids** are distended veins located **below the dentate line** in the anal canal, which are drained by the **inferior rectal veins**.
- The inferior rectal veins drain into the **internal pudendal vein**, then to the **internal iliac vein** (part of the **systemic venous circulation**).
*Internal pudendal vein*
- The **internal pudendal vein** drains structures in the perineum and external genitalia, but it is not the **primary/direct drainage** for hemorrhoids.
- It receives blood from the inferior rectal veins but is one step removed from the hemorrhoidal plexus itself.
*Left colic vein*
- The **left colic vein** typically drains the distal transverse colon and descending colon.
- It is part of the **inferior mesenteric venous system** and is anatomically distant from the anorectal region, not involved in draining hemorrhoids.
*Middle rectal vein*
- The **middle rectal vein** drains the middle part of the rectum and connects both portal and systemic circulations.
- It drains the **muscularis layer** of the rectum but is not the primary drainage for the external hemorrhoidal plexus below the dentate line.
*Superior rectal vein*
- The **superior rectal vein** drains the upper part of the rectum and anal canal **above the dentate line**.
- Distention of these veins leads to **internal hemorrhoids**, which are typically painless unless prolapsed or thrombosed.
- It drains into the **inferior mesenteric vein** (part of the **portal venous circulation**).
More Perineum and ischioanal fossa US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.