Pelvic vasculature and lymphatics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pelvic vasculature and lymphatics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pelvic vasculature and lymphatics US Medical PG Question 1: During a surgical procedure to repair an abdominal aortic aneurysm, the surgeon must be careful to avoid injury to which of the following arterial structures that originates near the level of the renal vessels?
- A. Left renal artery (Correct Answer)
- B. Celiac trunk
- C. Right renal artery
- D. Superior mesenteric artery
Pelvic vasculature and lymphatics Explanation: ***Left renal artery***
- The **left renal artery** arises from the aorta usually just below the superior mesenteric artery, making it susceptible to injury during an **abdominal aortic aneurysm (AAA) repair** if the aneurysm extends proximally.
- Its proximity to the typical location of AAA, often near or involving the **infrarenal aorta**, necessitates careful identification and protection during clamping or graft placement.
*Celiac trunk*
- The **celiac trunk** originates higher up from the aorta, typically at the level of **T12-L1 vertebrae**, well above the common infrarenal AAA repair site.
- While important, it is generally less directly threatened during a typical infrarenal AAA repair compared to arteries immediately adjacent to or within the aneurysm sac.
*Right renal artery*
- The **right renal artery** also originates from the aorta near the level of the renal veins, but it is typically located more posteriorly and usually passes behind the inferior vena cava.
- Although it can be at risk, the left renal artery's course is often more anterior and directly in the field of dissection for the **aortic neck** during AAA repair.
*Superior mesenteric artery*
- The **superior mesenteric artery (SMA)** originates from the aorta proximal to the renal arteries, typically around the L1 vertebral level.
- While crucial, its origin is usually cephalad to the infrarenal aneurysm neck, making it generally less prone to direct injury during infrarenal AAA repair, though flow must be monitored.
Pelvic vasculature and lymphatics US Medical PG Question 2: A 17-year-old girl presents to her pediatrician for a wellness visit. She currently feels well but is concerned that she has not experienced menarche. She reports to recently developing headaches and describes them as pulsating, occurring on the left side of her head, associated with nausea, and relieved by ibuprofen. She is part of the school’s rugby team and competitively lifts weights. She is currently sexually active and uses condoms infrequently. She denies using any forms of contraception or taking any medications. Her temperature is 98.6°F (37°C), blood pressure is 137/90 mmHg, pulse is 98/min, and respirations are 17/min. On physical exam, she has normal breast development and pubic hair is present. A pelvic exam is performed. A urine hCG test is negative. Which of the following is the best next step in management?
- A. Serum testosterone
- B. Serum T3 and T4
- C. Serum estradiol
- D. MRI of the head
- E. Pelvic ultrasound (Correct Answer)
Pelvic vasculature and lymphatics Explanation: ***Pelvic ultrasound***
- A pelvic ultrasound is the **best initial step** to visualize the anatomy of the reproductive organs and rule out structural abnormalities like **Müllerian agenesis** or an imperforate hymen, which could explain primary amenorrhea despite normal secondary sexual characteristics.
- Given the patient's **primary amenorrhea** (absence of menarche by age 15 with secondary sexual characteristics) and active sexual life, a pelvic ultrasound can also help identify potential abnormalities such as a **cryptomenorrhea** due to outflow tract obstruction.
*MRI of the head*
- While an MRI of the head might be considered later to evaluate for **hypothalamic or pituitary causes** (e.g., tumors like craniopharyngioma or prolactinoma) of primary amenorrhea, it is not the initial imaging step.
- The patient's headaches, though concerning for migraine, are likely **unrelated** to her primary amenorrhea at this stage without other neurological signs or significantly elevated prolactin levels.
*Serum estradiol*
- Measuring serum estradiol levels is important in evaluating primary amenorrhea to assess **gonadal function** and differentiate between hypogonadotropic and hypergonadotropic hypogonadism.
- However, direct visualization of the reproductive tract and ruling out **anatomical obstructions** is typically a more immediate and critical first step in a patient with normal secondary sexual development.
*Serum T3 and T4*
- Thyroid hormone levels (T3 and T4) are assessed to rule out **thyroid dysfunction** (hypothyroidism or hyperthyroidism) as a cause of menstrual irregularities or primary amenorrhea.
- While thyroid issues can affect menstruation, they are generally not the most common or immediate cause to investigate in a patient with **normal secondary sexual characteristics** and no other overt symptoms of thyroid disease.
*Serum testosterone*
- Serum testosterone levels are useful in evaluating for **hyperandrogenism**, which might be seen in conditions like **Polycystic Ovary Syndrome (PCOS)** or **androgen-secreting tumors**.
- However, in this patient with normal breast development and pubic hair but no menarche, the initial focus is on confirming the presence of a **uterus and ovaries** and ruling out anatomical obstructions, rather than immediately investigating androgen excess.
Pelvic vasculature and lymphatics US Medical PG Question 3: A 32-year-old man presents to his primary care physician complaining of pain accompanied by a feeling of heaviness in his scrotum. He is otherwise healthy except for a broken arm he obtained while skiing several years ago. Physical exam reveals an enlarged “bag of worms” upon palpation of the painful scrotal region. Shining a light over this area shows that the scrotum does not transilluminate. Which of the following statements is true about the most likely cause of this patient's symptoms?
- A. Equally common on both sides
- B. More common on left due to drainage into renal vein (Correct Answer)
- C. More common on right due to drainage into renal vein
- D. More common on right due to drainage into inferior vena cava
- E. More common on left due to drainage into inferior vena cava
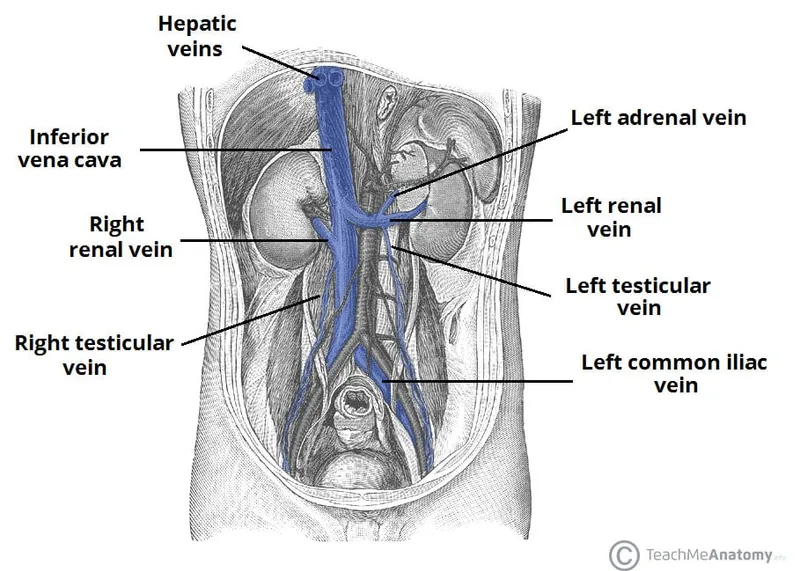
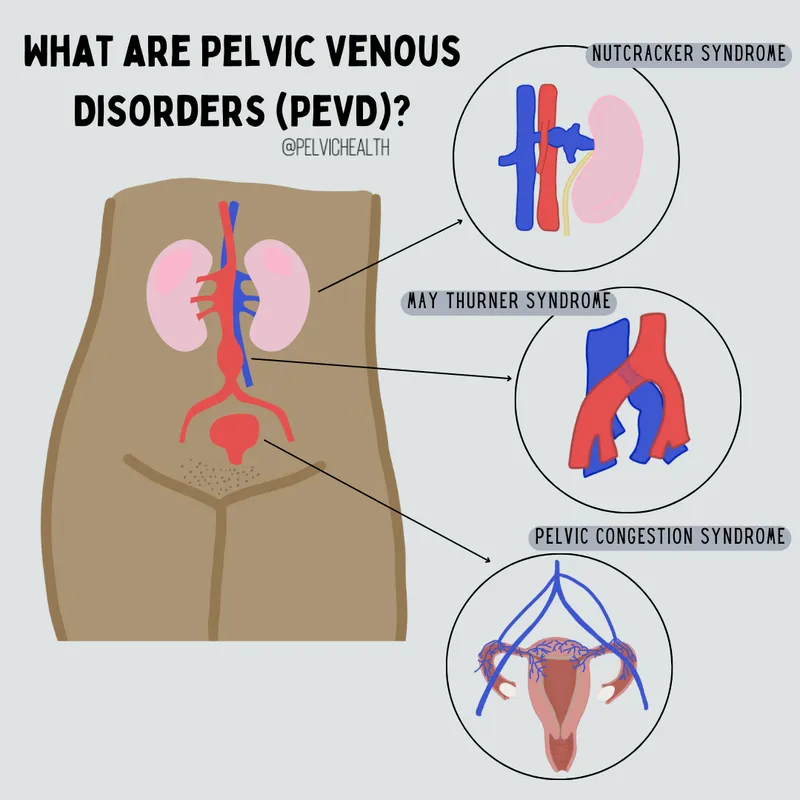
Pelvic vasculature and lymphatics Explanation: ***More common on left due to drainage into renal vein***
- The patient's symptoms of scrotal pain, "bag of worms" on palpation, and lack of transillumination are classic for a **left-sided varicocele**.
- The longer course and perpendicular drainage of the **left testicular vein** into the left renal vein create higher pressure, making varicocele formation more common on the left.
*Equally common on both sides*
- Varicoceles are distinctly asymmetrical, with a well-established higher incidence on the left side due to anatomical differences.
- Bilateral varicoceles can occur but are less common than isolated left-sided ones and do not support an "equally common" distribution.
*More common on right due to drainage into renal vein*
- The right testicular vein typically drains directly into the **inferior vena cava (IVC)**, not the renal vein, which is a lower pressure system compared to the left.
- Therefore, anatomical factors do not favor varicocele formation on the right side due to drainage into the renal vein.
*More common on right due to drainage into inferior vena cava*
- While the right testicular vein drains into the IVC, this direct drainage path is associated with good venous return and a lower risk of varicocele.
- A right-sided varicocele is less common and, if present, should prompt investigation for retroperitoneal mass obstructing the IVC or right testicular vein.
*More common on left due to drainage into inferior vena cava*
- The left testicular vein typically drains into the **left renal vein**, not directly into the inferior vena cava.
- This anatomical description is incorrect and does not explain the higher incidence of left-sided varicoceles.
Pelvic vasculature and lymphatics US Medical PG Question 4: A 39-year-old man presents with painless swelling of the right testis and a sensation of heaviness. The physical examination revealed an intra-testicular solid mass that could not be felt separately from the testis. After a thorough evaluation, he was diagnosed with testicular seminoma. Which of the following group of lymph nodes are most likely involved?
- A. Superficial inguinal lymph nodes (lateral group)
- B. Deep inguinal lymph nodes
- C. Superficial inguinal lymph nodes (medial group)
- D. Para-rectal lymph nodes
- E. Para-aortic lymph nodes (Correct Answer)
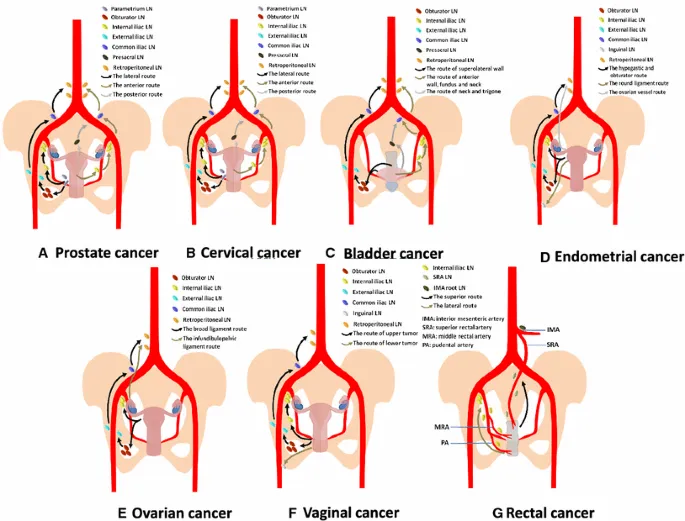
Pelvic vasculature and lymphatics Explanation: ***Para-aortic lymph nodes***
- The **testes** develop in the abdomen and descend into the scrotum, retaining their original lymphatic drainage. Therefore, **testicular cancer** typically metastasizes to the **para-aortic** (or retroperitoneal) lymph nodes, which are located near the renal veins at the level of L1-L2.
- This is the primary lymphatic drainage pathway for the testes.
*Superficial inguinal lymph nodes (lateral group)*
- These lymph nodes primarily drain the skin of the **scrotum**, perineum, and lower limbs, but not the **testes** themselves.
- Involvement would suggest spread to the scrotal skin or compromised lymphatic flow due to prior scrotal surgery or infection, which is not indicated here.
*Deep inguinal lymph nodes*
- **Deep inguinal lymph nodes** drain structures deeper in the leg and gluteal region, as well as receiving efferent vessels from the superficial inguinal nodes.
- They are not the primary drainage site for the **testes**.
*Superficial inguinal lymph nodes (medial group)*
- Similar to the lateral group, the **medial superficial inguinal lymph nodes** primarily drain the external genitalia (excluding the testes), perineum, and lower abdominal wall.
- They are not the direct drainage route for **testicular cancer**.
*Para-rectal lymph nodes*
- **Para-rectal lymph nodes** are located near the rectum and are involved in the drainage of the rectum and lower sigmoid colon.
- They have no direct connection to the lymphatic drainage of the **testes**.
Pelvic vasculature and lymphatics US Medical PG Question 5: A child is in the nursery one day after birth. A nurse notices a urine-like discharge being expressed through the umbilical stump. What two structures in the embryo are connected by the structure that failed to obliterate during the embryologic development of this child?
- A. Kidney - large bowel
- B. Liver - umbilical vein
- C. Bladder - small bowel
- D. Pulmonary artery - aorta
- E. Bladder - umbilicus (Correct Answer)
Pelvic vasculature and lymphatics Explanation: ***Bladder - umbilicus***
- A **urine-like discharge** from the umbilical stump indicates a **patent urachus**, which is the embryonic remnant of the allantois.
- The **allantois** (which becomes the urachus) is an embryonic structure that connects the **fetal bladder** to the **umbilicus** during development.
- Normally, the allantois obliterates after birth to form the **median umbilical ligament**, but failure to obliterate results in a patent urachus allowing urine to discharge through the umbilicus.
*Kidney - large bowel*
- These two structures are not directly connected by an obliterating embryonic structure relevant to urine discharge from an umbilical stump.
- The kidneys form urine, and the large bowel is part of the digestive tract, with no direct embryonic communication to the umbilicus for urine expression.
*Liver - umbilical vein*
- The umbilical vein connects the **placenta to the fetal liver** (and ductus venosus) to transport oxygenated blood, not urine.
- Failure of the umbilical vein to obliterate would result in a patent umbilical vein, typically presenting as a vascular anomaly, not urine discharge.
*Pulmonary artery - aorta*
- These structures are connected by the **ductus arteriosus** in fetal circulation, bypassing the pulmonary circulation.
- While important for fetal development, a patent ductus arteriosus (PDA) is a cardiovascular anomaly and would not manifest as urine discharge from the umbilical stump.
*Bladder - small bowel*
- While both structures are involved in waste elimination, there is no normal embryonic structure directly connecting the bladder and small bowel that obliterates to prevent urine discharge from the umbilicus.
- An abnormal connection between the bladder and bowel would typically involve a **fistula** and present with stool in urine or urine in stool, not umbilical discharge.
Pelvic vasculature and lymphatics US Medical PG Question 6: A 28-year-old man comes to the physician because of a 2-week history of testicular swelling and dull lower abdominal discomfort. Physical examination shows a firm, nontender left testicular nodule. Ultrasonography of the scrotum shows a well-defined hypoechoic lesion of the left testicle. Serum studies show an elevated β-hCG concentration and a normal α-fetoprotein concentration. The patient undergoes a radical inguinal orchiectomy. Histopathologic examination of the surgical specimen shows a mixed germ cell tumor with invasion of adjacent lymphatic vessels. Further evaluation is most likely to show malignant cells in which of the following lymph node regions?
- A. External iliac
- B. Deep inguinal
- C. Para-aortic (Correct Answer)
- D. Mediastinal
- E. Internal iliac
Pelvic vasculature and lymphatics Explanation: ***Para-aortic***
- Testicular lymphatic drainage primarily follows the **gonadal vessels** back to the para-aortic lymph nodes (also known as retroperitoneal lymph nodes).
- This is the **most common site** for metastatic spread of testicular germ cell tumors.
*External iliac*
- The external iliac lymph nodes primarily drain structures in the pelvis and lower limbs, such as the bladder and vagina, not the testes.
- While they can be involved in advanced pelvic malignancies, they are not the primary drainage site for testicular cancer.
*Deep inguinal*
- The deep inguinal lymph nodes primarily drain the superficial inguinal lymph nodes, which receive lymphatic drainage from the penis, scrotum (superficial layers), and perineum.
- Testicular lymphatics bypass the inguinal nodes unless there is scrotal invasion or prior surgery involving the scrotum.
*Mediastinal*
- Mediastinal lymph nodes are involved in the lymphatic drainage of thoracic organs and can be affected in later stages of testicular cancer if there is widespread metastatic disease, particularly to the lungs.
- However, they are not the initial or primary site of lymphatic spread from testicular tumors.
*Internal iliac*
- The internal iliac lymph nodes primarily drain pelvic organs and the deep perineum.
- While they may be involved in some pelvic cancers, they are not the primary lymphatic drainage site for the testes.
Pelvic vasculature and lymphatics US Medical PG Question 7: A researcher is investigating the blood supply of the adrenal gland. While performing an autopsy on a patient who died from unrelated causes, he identifies a vessel that supplies oxygenated blood to the inferior aspect of the right adrenal gland. Which of the following vessels most likely gave rise to the vessel in question?
- A. Inferior phrenic artery
- B. Abdominal aorta
- C. Renal artery (Correct Answer)
- D. Superior mesenteric artery
- E. Common iliac artery
Pelvic vasculature and lymphatics Explanation: ***Renal artery***
- The **inferior suprarenal artery**, which supplies the inferior part of the adrenal gland, typically arises from the **renal artery**.
- The adrenal glands receive a rich blood supply from three main arterial sources: superior, middle, and inferior suprarenal arteries.
*Inferior phrenic artery*
- The **superior suprarenal arteries** typically arise from the **inferior phrenic arteries** and supply the superior aspect of the adrenal glands.
- While critical for adrenal blood supply, they do not typically contribute to the inferior aspect directly.
*Abdominal aorta*
- The **middle suprarenal artery** usually arises directly from the **abdominal aorta**.
- This vessel supplies the central part of the adrenal gland, but not primarily the inferior aspect.
*Superior mesenteric artery*
- The **superior mesenteric artery** primarily supplies structures of the midgut (e.g., small intestine, ascending colon) and does not typically give rise to vessels supplying the adrenal glands.
- It is located inferior to the origin of the renal arteries and the adrenal glands.
*Common iliac artery*
- The **common iliac arteries** supply the lower limbs and pelvic organs, originating from the abdominal aorta bifurcation.
- These arteries are located much too far inferior to supply the adrenal glands, which are retroperitoneal structures in the upper abdomen.
Pelvic vasculature and lymphatics US Medical PG Question 8: A father brings his 1-year-old son into the pediatrician's office for a routine appointment. He states that his son is well but mentions that he has noticed an intermittent bulge on the right side of his son's groin whenever he cries or strains for bowel movement. Physical exam is unremarkable. The physician suspects a condition that may be caused by incomplete obliteration of the processus vaginalis. Which condition is caused by the same defective process?
- A. Diaphragmatic hernia
- B. Femoral hernia
- C. Testicular torsion
- D. Hydrocele (Correct Answer)
- E. Varicocele
Pelvic vasculature and lymphatics Explanation: ***Hydrocele***
- The patient's symptoms (intermittent groin bulge with crying/straining) are classic for an **indirect inguinal hernia**, which, like a hydrocele, results from an **incompletely obliterated processus vaginalis**.
- A **hydrocele** involves the accumulation of **serous fluid** within the persistent processus vaginalis, as opposed to abdominal contents in a hernia.
*Diaphragmatic hernia*
- This condition involves the protrusion of abdominal contents into the chest cavity through a defect in the **diaphragm**.
- It is unrelated to the obliteration of the processus vaginalis but rather to **diaphragmatic development**.
*Femoral hernia*
- A femoral hernia involves protrusion through the **femoral canal**, inferior to the inguinal ligament.
- It does not involve the processus vaginalis and is more common in **multiparous women**.
*Testicular torsion*
- This condition is a surgical emergency caused by the **twisting of the spermatic cord**, compromising blood supply to the testis.
- It is not related to the processus vaginalis but often involves an inadequately fixed testis (bell-clapper deformity).
*Varicocele*
- A varicocele is an abnormal dilation of the **pampiniform venous plexus** within the spermatic cord.
- It is caused by incompetent valves in the testicular veins and not by a patent processus vaginalis.
Pelvic vasculature and lymphatics US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Pelvic vasculature and lymphatics Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Pelvic vasculature and lymphatics US Medical PG Question 10: Thirty minutes after normal vaginal delivery of twins, a 35-year-old woman, gravida 5, para 4, has heavy vaginal bleeding with clots. Physical examination shows a soft, enlarged, and boggy uterus. Despite bimanual uterine massage, administration of uterotonic drugs, and placement of an intrauterine balloon for tamponade, the bleeding continues. A hysterectomy is performed. Vessels running through which of the following structures must be ligated during the surgery to achieve hemostasis?
- A. Suspensory ligament
- B. Round ligament
- C. Ovarian ligament
- D. Uterosacral ligament
- E. Cardinal ligament (Correct Answer)
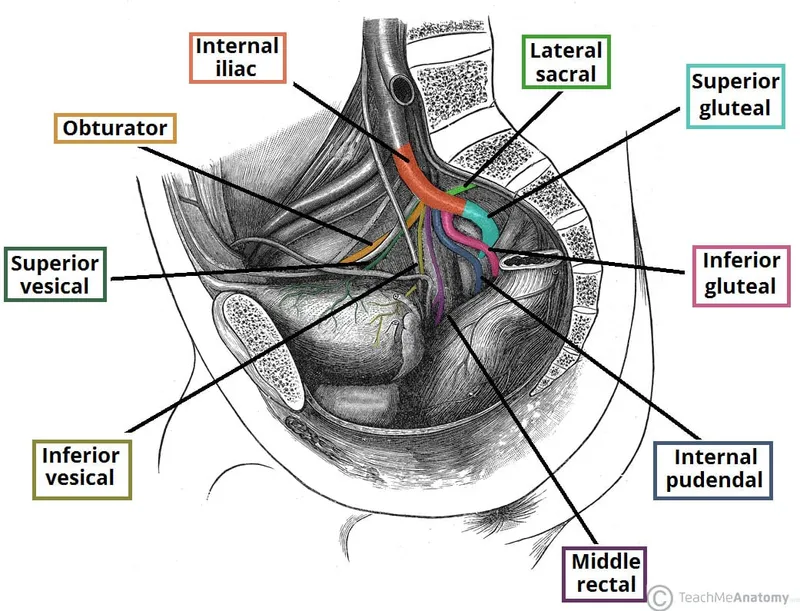
Pelvic vasculature and lymphatics Explanation: ***Cardinal ligament***
- The **uterine artery** and **uterine vein**, which supply the uterus, run through the **cardinal ligament** (also known as the transverse cervical ligament).
- Ligation of these vessels is crucial during a hysterectomy to control bleeding from the uterus.
*Suspensory ligament*
- The **suspensory ligament of the ovary** contains the **ovarian artery** and vein, which primarily supply the ovaries and fallopian tubes.
- While these may be ligated during a hysterectomy if the ovaries are removed, they are not the primary vessels causing uterine bleeding in postpartum hemorrhage.
*Round ligament*
- The **round ligament of the uterus** extends from the uterus to the labia majora and contains relatively small vessels, primarily contributing to uterine support.
- Ligation of this ligament alone would not effectively control heavy uterine bleeding.
*Ovarian ligament*
- The **ovarian ligament** connects the ovary to the uterus and contains small vessels that mainly supply the ovary.
- It does not house the major blood supply to the uterus itself.
*Uterosacral ligament*
- The **uterosacral ligaments** primarily provide support to the uterus by connecting it to the sacrum and contain small nerves and vessels.
- Ligation of these ligaments would not control the main arterial supply to the uterus.
More Pelvic vasculature and lymphatics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.