Pelvic girdle and ligaments US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pelvic girdle and ligaments. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pelvic girdle and ligaments US Medical PG Question 1: A newborn girl is delivered vaginally at term to a healthy 25-year-old G1P1. The pregnancy was uncomplicated. On examination, she was found to have a slight anal invagination, but no opening. Further examination shows a vestibular fistula and normally developed external genitalia. Which of the following statements about this condition is correct?
- A. Such abnormal anatomy is formed after week 12 of intrauterine development.
- B. The presence of an associated perineal or vestibular fistula is more likely in females with trisomy 21.
- C. There is a failure of the division of the embryonic cloaca into the urogenital sinus and rectoanal canal.
- D. Other congenital abnormalities are extremely rare in patients with this condition.
- E. There is a failure of the rupture of the anal membrane (dorsal portion of the cloacal membrane). (Correct Answer)
Pelvic girdle and ligaments Explanation: ***There is a failure of the rupture of the anal membrane (dorsal portion of the cloacal membrane).***
- This clinical presentation describes an **imperforate anus** with a **vestibular fistula**, a type of anorectal malformation (ARM).
- During normal development, the **urorectal septum** divides the cloaca into the urogenital sinus (ventral) and anorectal canal (dorsal), and the **cloacal membrane** is similarly divided into the **urogenital membrane** and **anal membrane**.
- The **anal membrane** (the dorsal portion of the cloacal membrane) normally ruptures around week 8 to form the anal opening. Failure of this rupture results in **imperforate anus**.
- The presence of a **vestibular fistula** indicates an abnormal communication between the rectal pouch and the vestibule, reflecting incomplete separation of the urogenital and anorectal structures.
*Such abnormal anatomy is formed after week 12 of intrauterine development.*
- **Anorectal malformations (ARMs)**, including imperforate anus with fistula, arise from defects in the development of the **cloaca** and **urorectal septum**, which occurs between **weeks 4 and 7** of gestation.
- By week 12, organogenesis is largely complete, and such gross anatomical defects would have already occurred earlier in embryonic development.
*The presence of an associated perineal or vestibular fistula is more likely in females with trisomy 21.*
- While anorectal malformations can be associated with various chromosomal anomalies, **Trisomy 21 (Down syndrome)** is not specifically associated with a higher incidence of vestibular fistulas.
- Anorectal malformations are more commonly associated with **VACTERL association** (Vertebral defects, Anal atresia, Cardiac defects, Tracheoesophageal fistula, Esophageal atresia, Renal anomalies, and Limb defects), which typically occurs sporadically without a specific chromosomal abnormality.
*There is a failure of the division of the embryonic cloaca into the urogenital sinus and rectoanal canal.*
- While incomplete cloacal septation contributes to anorectal malformations, a **complete failure** of cloacal division typically results in a **persistent cloaca**, where there is a single common opening for the urinary, genital, and gastrointestinal tracts.
- The described presentation has normally developed external genitalia with a separate vestibular fistula, indicating that cloacal division occurred but was abnormal, and the primary defect is failure of anal membrane rupture.
*Other congenital abnormalities are extremely rare in patients with this condition.*
- **Anorectal malformations (ARMs)** are frequently associated with other congenital anomalies, with approximately **50-60%** of affected individuals having at least one additional defect.
- Associated anomalies commonly include components of **VACTERL association** and involve the genitourinary system (30-50%), vertebral/skeletal system (30%), cardiac system (10-20%), and gastrointestinal tract (esophageal atresia, duodenal atresia).
Pelvic girdle and ligaments US Medical PG Question 2: A 28-year-old man is admitted to the hospital for the evaluation of symmetric, ascending weakness that started in his feet and has become progressively worse over the past 5 days. A lumbar puncture is performed to confirm the diagnosis. As the needle is advanced during the procedure, there is resistance just before entering the epidural space. This resistance is most likely due to which of the following structures?
- A. Dura mater
- B. Supraspinous ligament
- C. Interspinous ligament
- D. Ligamentum flavum (Correct Answer)
- E. Superficial fascia
Pelvic girdle and ligaments Explanation: ***Ligamentum flavum***
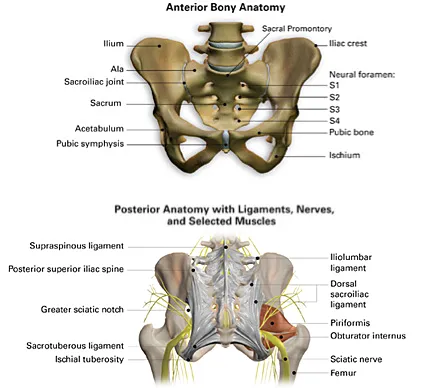
- The **ligamentum flavum** is encountered after the interspinous ligament and is the last major ligament traversed before entering the **epidural space**.
- It is a **thick, elastic, and strong ligament** that provides significant resistance to the needle, often described as a "pop" or "give" sensation as it is penetrated.
*Dura mater*
- The **dura mater** is the outermost membrane of the meninges and is encountered *after* the epidural space, surrounding the spinal cord.
- While it provides some resistance, the more significant resistance *just before* the epidural space is due to the ligamentum flavum.
*Supraspinous ligament*
- The **supraspinous ligament** is a strong fibrous cord that connects the tips of the spinous processes.
- It is located more superficially and is therefore encountered much earlier in the lumbar puncture procedure, not just before the epidural space.
*Interspinous ligament*
- The **interspinous ligament** connects adjacent spinous processes and is traversed *before* the ligamentum flavum.
- It offers some resistance, but it is typically less prominent than the resistance felt when penetrating the thicker ligamentum flavum.
*Superficial fascia*
- The **superficial fascia** is located immediately beneath the skin and subcutaneous tissue.
- It is encountered very early in the procedure and would not be the structure providing resistance just before the epidural space.
Pelvic girdle and ligaments US Medical PG Question 3: A 47-year-old woman comes to the physician because of involuntary leakage of urine for the past 4 months, which she has experienced when bicycling to work and when laughing. She has not had any dysuria or urinary urgency. She has 4 children that were all delivered vaginally. She is otherwise healthy and takes no medications. The muscles most likely affected by this patient's condition receive efferent innervation from which of the following structures?
- A. S3–S4 nerve roots (Correct Answer)
- B. Obturator nerve
- C. Superior hypogastric plexus
- D. Superior gluteal nerve
- E. S1-S2 nerve roots
Pelvic girdle and ligaments Explanation: ***S3–S4 nerve roots***
- The patient's symptoms of **involuntary urine leakage** during physical activity (**stress incontinence**) and a history of multiple vaginal deliveries strongly suggest **pelvic floor muscle weakness**.
- The **levator ani muscles**, which are crucial for maintaining urinary continence, receive their primary innervation from the **pudendal nerve**, which originates from the **S2-S4 spinal nerves** (though contributions from S3-S4 are often highlighted for pelvic floor efferent innervation).
*Obturator nerve*
- The **obturator nerve** primarily innervates the **adductor muscles of the thigh** (e.g., adductor longus, magnus, brevis, gracilis), as well as the obturator externus muscle.
- It does not significantly contribute to the innervation of the **pelvic floor muscles** responsible for urinary continence.
*Superior hypogastric plexus*
- The **superior hypogastric plexus** is part of the **autonomic nervous system** and primarily carries **sympathetic innervation** to the pelvic organs.
- While it plays a role in bladder function (e.g., bladder relaxation and internal urethral sphincter contraction), it does not provide **somatic efferent innervation** to the skeletal muscles of the pelvic floor.
*Superior gluteal nerve*
- The **superior gluteal nerve** innervates the **gluteus medius**, **gluteus minimus**, and **tensor fasciae latae muscles**.
- These muscles are involved in **hip abduction** and **medial rotation** and are not directly involved in maintaining urinary continence through the pelvic floor.
*S1-S2 nerve roots*
- While the **S1-S2 nerve roots** contribute to the innervation of various lower limb muscles and sensory pathways, their primary efferent contributions related to pelvic floor continence are not as direct as S3-S4.
- The **pudendal nerve**, critical for pelvic floor muscle function, originates predominantly from **S2-S4**, with S3-S4 being particularly important for the motor components.
Pelvic girdle and ligaments US Medical PG Question 4: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Pelvic girdle and ligaments Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Pelvic girdle and ligaments US Medical PG Question 5: Thirty minutes after normal vaginal delivery of twins, a 35-year-old woman, gravida 5, para 4, has heavy vaginal bleeding with clots. Physical examination shows a soft, enlarged, and boggy uterus. Despite bimanual uterine massage, administration of uterotonic drugs, and placement of an intrauterine balloon for tamponade, the bleeding continues. A hysterectomy is performed. Vessels running through which of the following structures must be ligated during the surgery to achieve hemostasis?
- A. Suspensory ligament
- B. Round ligament
- C. Ovarian ligament
- D. Uterosacral ligament
- E. Cardinal ligament (Correct Answer)
Pelvic girdle and ligaments Explanation: ***Cardinal ligament***
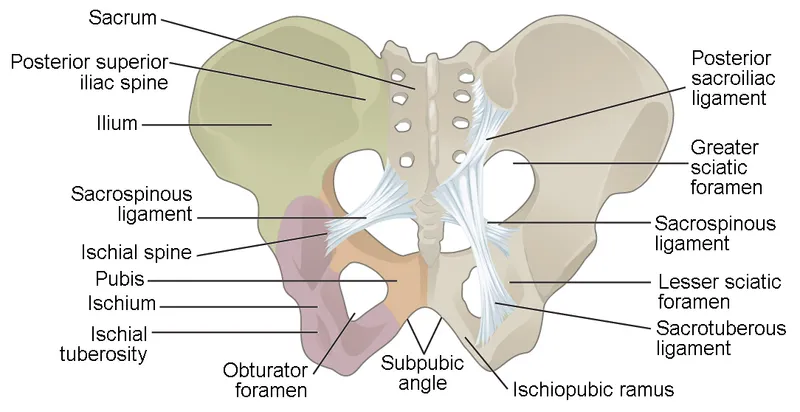
- The **uterine artery** and **uterine vein**, which supply the uterus, run through the **cardinal ligament** (also known as the transverse cervical ligament).
- Ligation of these vessels is crucial during a hysterectomy to control bleeding from the uterus.
*Suspensory ligament*
- The **suspensory ligament of the ovary** contains the **ovarian artery** and vein, which primarily supply the ovaries and fallopian tubes.
- While these may be ligated during a hysterectomy if the ovaries are removed, they are not the primary vessels causing uterine bleeding in postpartum hemorrhage.
*Round ligament*
- The **round ligament of the uterus** extends from the uterus to the labia majora and contains relatively small vessels, primarily contributing to uterine support.
- Ligation of this ligament alone would not effectively control heavy uterine bleeding.
*Ovarian ligament*
- The **ovarian ligament** connects the ovary to the uterus and contains small vessels that mainly supply the ovary.
- It does not house the major blood supply to the uterus itself.
*Uterosacral ligament*
- The **uterosacral ligaments** primarily provide support to the uterus by connecting it to the sacrum and contain small nerves and vessels.
- Ligation of these ligaments would not control the main arterial supply to the uterus.
Pelvic girdle and ligaments US Medical PG Question 6: An MRI of a patient with low back pain reveals compression of the L5 nerve root. Which of the following muscles would most likely show weakness during physical examination?
- A. Tibialis posterior
- B. Tibialis anterior (Correct Answer)
- C. Gastrocnemius
- D. Quadriceps femoris
Pelvic girdle and ligaments Explanation: ***Tibialis anterior***
- The **L5 nerve root** primarily innervates muscles responsible for **dorsiflexion** of the foot, with the **tibialis anterior** being the primary dorsiflexor.
- Weakness of the tibialis anterior would manifest as difficulty lifting the front of the foot, potentially leading to a **foot drop** gait.
*Tibialis posterior*
- The **tibialis posterior** is primarily innervated by the **tibial nerve** (S1-S2) and is responsible for **plantarflexion** and **inversion** of the foot.
- Weakness in this muscle would not be the most likely presentation of L5 nerve root compression.
*Gastrocnemius*
- The **gastrocnemius** muscle is primarily innervated by the **tibial nerve** (S1-S2) and is a powerful **plantarflexor** of the foot.
- Weakness in this muscle would indicate an S1 or S2 nerve root issue, not typically L5.
*Quadriceps femoris*
- The **quadriceps femoris** is innervated by the **femoral nerve**, predominantly originating from the **L2, L3, and L4 nerve roots**.
- Weakness would manifest as difficulty extending the knee, which is not characteristic of L5 compression.
Pelvic girdle and ligaments US Medical PG Question 7: A 45-year-old man is brought to the emergency department following a motor vehicle collision. He reports right hip pain and numbness along the right thigh. Physical examination shows decreased sensation to light touch over a small area of the proximal medial thigh. X-rays of the pelvis show a displaced pelvic ring fracture. Further evaluation of this patient is most likely to show which of the following findings?
- A. Sensory deficit of the dorsal foot
- B. Absent cremasteric reflex
- C. Impaired hip extension
- D. Impaired adduction of the hip (Correct Answer)
- E. Impaired extension of the knee
Pelvic girdle and ligaments Explanation: ***Impaired adduction of the hip***
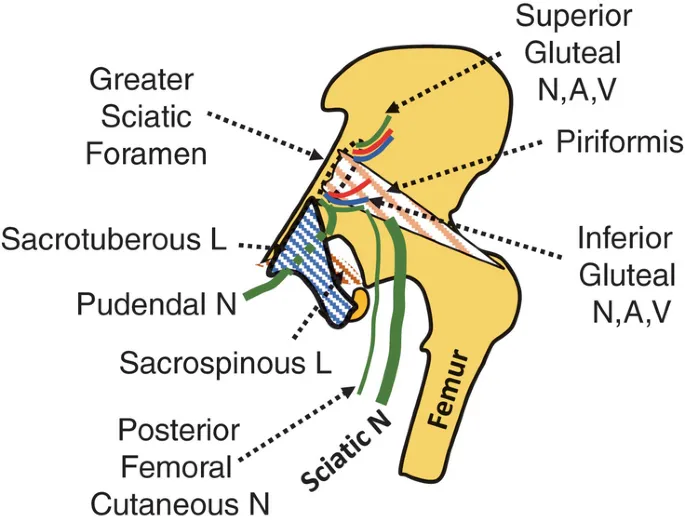
- The patient's **numbness along the right thigh** and **decreased sensation to light touch over the proximal medial thigh**, combined with a **pelvic ring fracture**, points to probable injury of the **obturator nerve**.
- The **obturator nerve** innervates the **adductor muscles** of the hip, and its injury would result in impaired hip adduction and sensory deficits in the medial thigh.
*Sensory deficit of the dorsal foot*
- A sensory deficit on the **dorsal foot** is typically associated with injury to the **peroneal nerve**, which is less likely to be affected by a pelvic ring fracture leading to medial thigh numbness.
- Peroneal nerve injury often results from trauma to the **lateral knee** or prolonged compression.
*Absent cremasteric reflex*
- An absent **cremasteric reflex** suggests injury to the **ilioinguinal** or **genitofemoral nerves**, or spinal cord injury at the L1-L2 level.
- While these nerves can be affected by pelvic trauma, the specific sensory deficit described (proximal medial thigh) aligns more with obturator nerve involvement.
*Impaired hip extension*
- **Hip extension** is primarily controlled by the **gluteus maximus** and **hamstrings**, which are innervated by the **inferior gluteal nerve** and **sciatic nerve**, respectively.
- Injury to these nerves or muscles would not typically cause numbness in the proximal medial thigh.
*Impaired extension of the knee*
- **Knee extension** is mediated by the **quadriceps femoris** muscle group, innervated by the **femoral nerve**.
- While the femoral nerve can be injured in severe pelvic trauma, the sensory distribution described does not match the typical sensory deficits of femoral nerve injury (anterior and medial thigh, medial leg).
Pelvic girdle and ligaments US Medical PG Question 8: A 26-year-old woman presents to the obstetrics ward to deliver her baby. The obstetrician establishes a pudendal nerve block via intravaginal injection of lidocaine near the tip of the ischial spine. From which of the following nerve roots does the pudendal nerve originate?
- A. L4-L5
- B. S2-S4 (Correct Answer)
- C. L3-L4
- D. L5-S2
- E. L5-S1
Pelvic girdle and ligaments Explanation: ***S2-S4***
- The **pudendal nerve** originates from the **sacral plexus**, specifically from the ventral rami of spinal nerves **S2, S3, and S4**.
- Its origin from these segments is crucial for its function in innervating structures of the **perineum**, **external genitalia**, and the **anal and urethral sphincters**, making it highly relevant for procedures like **pudendal nerve blocks** during childbirth.
*L4-L5*
- Nerve roots **L4-L5** contribute significantly to the **lumbar plexus** and subsequently to nerves like the **femoral nerve** and portions of the **sciatic nerve**.
- These roots are primarily involved in innervating the **lower limbs** (e.g., quadriceps, tibialis anterior) and are not the primary origin of the pudendal nerve.
*L3-L4*
- The **L3-L4** nerve roots are also part of the **lumbar plexus**, chiefly contributing to the **femoral nerve**.
- They are essential for motor innervation of the **anterior thigh muscles** and sensation in this area, distinct from the pudendal nerve's role in the perineum.
*L5-S2*
- While **S2** is part of the pudendal nerve's origin, the inclusion of **L5** and **S1** primarily characterizes the origin of the **sciatic nerve** (which is formed by L4-S3) and its branches, such as the common fibular and tibial nerves.
- These roots are primarily concerned with the **posterior thigh** and **leg innervation**, not the perineum, which differentiates it from the pudendal nerve.
*L5-S1*
- The nerve roots **L5-S1** are key components of the **lumbosacral plexus** and contribute significantly to the **sciatic nerve**, particularly its innervation of the **hamstrings** and certain lower leg muscles.
- This origin does not align with the known roots of the **pudendal nerve** which stems from S2-S4.
Pelvic girdle and ligaments US Medical PG Question 9: A 60-year-old post-menopausal female presents to her gynecologist with vaginal bleeding. Her last period was over 10 years ago. Dilation and curettage reveals endometrial carcinoma so she is scheduled to undergo a total abdominal hysterectomy and bilateral salpingo-oophorectomy. During surgery, the gynecologist visualizes paired fibrous structures arising from the cervix and attaching to the lateral pelvic walls at the level of the ischial spines. Which of the following vessels is found within each of the paired visualized structure?
- A. Vaginal artery
- B. Superior vesical artery
- C. Uterine artery (Correct Answer)
- D. Artery of Sampson
- E. Ovarian artery
Pelvic girdle and ligaments Explanation: ***Uterine artery***
- The paired fibrous structures described are the **cardinal ligaments (transverse cervical ligaments)**, which contain the **uterine arteries** as they course towards the uterus.
- The uterine artery, a branch of the **internal iliac artery**, crosses over the **ureter** within the cardinal ligament—a critical anatomical relationship during gynecological surgery ("water under the bridge").
- This is the primary vessel within the cardinal ligament and the key vascular structure at risk during hysterectomy.
*Vaginal artery*
- The vaginal artery typically branches from the **uterine artery** or directly from the **internal iliac artery**, but it is not the main vessel found within the cardinal ligament.
- It primarily supplies the **vagina**, not contained within the cardinal ligament support structure.
*Superior vesical artery*
- The superior vesical artery supplies the **upper part of the bladder** and originates from the **umbilical artery** (a branch of the internal iliac artery).
- It is not anatomically associated with the cardinal ligament or uterine support structures.
*Artery of Sampson*
- The Artery of Sampson is a branch of the **uterine artery** that anastomoses with the **ovarian artery** within the **broad ligament**, not the cardinal ligament.
- It is a minor vessel involved in the dual blood supply to the ovaries and uterus, not a primary structure within the cardinal ligament.
*Ovarian artery*
- The ovarian artery originates directly from the **abdominal aorta** and travels within the **suspensory ligament of the ovary (infundibulopelvic ligament)**, not the cardinal ligament.
- It supplies the **ovaries and fallopian tubes**, with a trajectory that is anatomically distinct from structures within the cardinal ligament.
Pelvic girdle and ligaments US Medical PG Question 10: A 32-year-old man comes to the physician because of episodic tingling and numbness in his right hand for the past 3 months. His symptoms are worse in the evening. There is no history of trauma. He is employed as a carpenter. He has smoked 1 pack of cigarettes daily for the past 10 years. He drinks a pint of vodka daily. He does not use illicit drugs. His vital signs are within normal limits. Physical examination shows decreased pinch strength in the right hand. Sensations are decreased over the little finger and both the dorsal and palmar surfaces of the medial aspect of the right hand. Which of the following is the most likely site of nerve compression?
- A. Guyon canal
- B. Quadrilateral space
- C. Carpal tunnel
- D. Cubital tunnel (Correct Answer)
- E. Radial groove
Pelvic girdle and ligaments Explanation: ***Cubital tunnel***
- Compression of the **ulnar nerve** at the cubital tunnel typically presents with paresthesias and numbness in the **little finger** and medial half of the ring finger, along with weakness in **intrinsic hand muscles** (decreased pinch strength).
- The carpenter's occupation may involve repetitive elbow flexion, exacerbating **ulnar nerve compression** at the elbow.
*Guyon canal*
- Compression in the **Guyon canal** affects the **ulnar nerve** at the wrist.
- While it can cause similar sensory and motor deficits in the hand, the cubital tunnel is a more common site of compression for the ulnar nerve, and symptoms worsen with **elbow flexion**.
*Carpal tunnel*
- **Carpal tunnel syndrome** involves compression of the **median nerve** and causes numbness and tingling in the thumb, index, middle, and radial half of the ring finger, sparing the little finger.
- It does not cause decreased sensation over the **little finger**.
*Quadrilateral space*
- **Quadrilateral space syndrome** involves compression of the **axillary nerve** and presents with shoulder pain, paresthesias over the lateral shoulder, and weakness in abduction and external rotation.
- This does not align with the patient's hand symptoms.
*Radial groove*
- Compression of the **radial nerve** in the radial groove (spiral groove) of the humerus typically results in **wrist drop**, weakness in forearm and hand extensors, and sensory loss over the dorsum of the hand, not the ulnar distribution described.
- This is not consistent with the patient's sensory and motor deficits.
More Pelvic girdle and ligaments US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.