Pelvic floor muscles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pelvic floor muscles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pelvic floor muscles US Medical PG Question 1: A 53-year-old multiparous woman is scheduled to undergo elective sling surgery for treatment of stress incontinence. She has frequent loss of small amounts of urine when she coughs or laughs, despite attempts at conservative treatment. The physician inserts trocars in the obturator foramen bilaterally to make the incision and passes a mesh around the pubic bones and underneath the urethra to form a sling. During the procedure, the physician accidentally injures a nerve in the obturator foramen. The function of which of the following muscles is most likely to be affected following the procedure?
- A. Obturator internus
- B. Tensor fascia latae
- C. Adductor longus (Correct Answer)
- D. Semitendinosus
- E. Transversus abdominis
Pelvic floor muscles Explanation: ***Adductor longus***
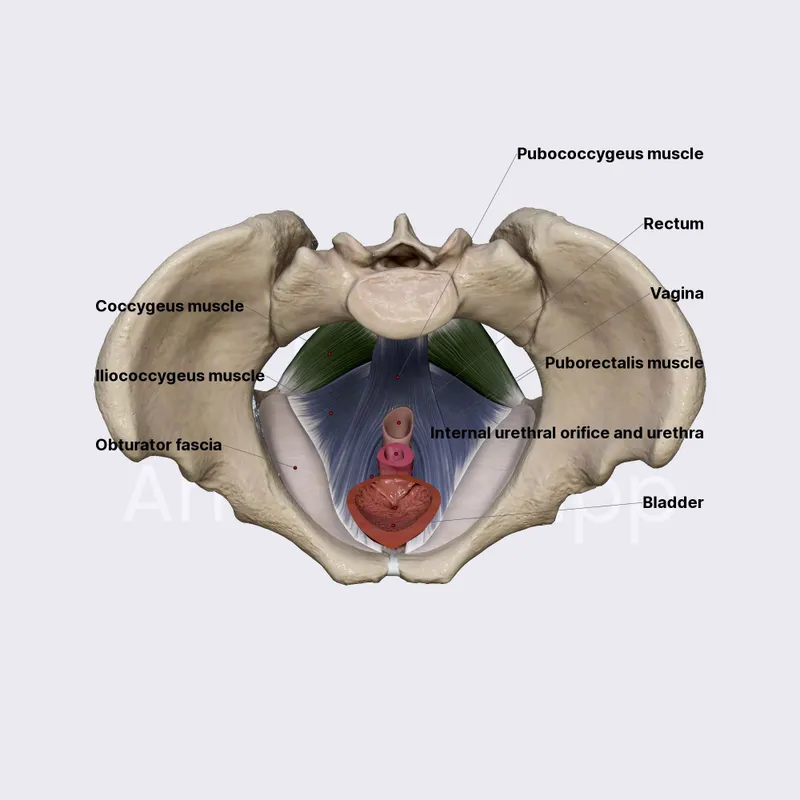
- The **obturator nerve** passes through the obturator foramen and innervates the **adductor muscles** of the thigh, including the **adductor longus**.
- Injury to the obturator nerve would therefore directly affect the function of the adductor longus, leading to impaired thigh adduction.
*Obturator internus*
- The **obturator internus** muscle is innervated by the **nerve to obturator internus**, which arises from the sacral plexus (L5-S2).
- This nerve does not pass through the obturator foramen, making injury to this muscle unlikely in this specific scenario.
*Tensor fascia latae*
- The **tensor fascia latae** is innervated by the **superior gluteal nerve** (L4-S1).
- The superior gluteal nerve is located deeper in the gluteal region and does not traverse the obturator foramen.
*Semitendinosus*
- The **semitendinosus** is one of the hamstring muscles and is innervated by the **tibial division of the sciatic nerve** (L5-S2).
- The sciatic nerve is located posteriorly in the thigh and does not pass through the obturator foramen.
*Transversus abdominis*
- The **transversus abdominis** muscle is innervated by the **thoracoabdominal nerves** (T7-T11) and the **subcostal nerve** (T12).
- These nerves supply the abdominal wall and are anatomically distant from the obturator foramen, hence injury is not expected.
Pelvic floor muscles US Medical PG Question 2: A 68-year-old man presents to his primary care physician complaining of a bulge in his scrotum that has enlarged over the past several months. He is found to have a right-sided inguinal hernia and undergoes elective hernia repair. At his first follow-up visit, he complains of a tingling sensation on his scrotum. Which of the following nerve roots communicates with the injured tissues?
- A. S1-S3
- B. L1-L2 (Correct Answer)
- C. S2-S4
- D. L4-L5
- E. L2-L3
Pelvic floor muscles Explanation: ***L1-L2***
- The **ilioinguinal nerve** and **genitofemoral nerve**, which are commonly injured during inguinal hernia repair, arise from the **L1 and L2 spinal nerves**.
- These nerves provide sensory innervation to the **scrotum**, **inguinal region**, and **medial thigh**, explaining the patient's tingling sensation.
*S1-S3*
- These nerve roots typically contribute to the **sciatic nerve** and innervate the posterior thigh, leg, and foot, and are not directly involved in scrotal sensation relevant to an inguinal hernia repair.
- They also contribute to the **pudendal nerve**, which primarily supplies the perineum and external genitalia, but injury to this nerve is less common in routine inguinal hernia repair.
*S2-S4*
- These nerve roots primarily form the **pudendal nerve**, which innervates the **perineum** and external genitalia (including some scrotal sensation), but injury to these specific nerves is not a typical complication of routine inguinal hernia repair.
- They also contribute to the **pelvic splanchnic nerves**, controlling bladder and bowel function, which are unrelated to the described sensory deficit.
*L4-L5*
- These nerve roots primarily contribute to nerves supplying the **lower limb**, such as the **femoral nerve** and **sciatic nerve**, and do not directly innervate the scrotum.
- Injury to these roots would typically result in motor or sensory deficits of the **thigh and leg**, not isolated scrotal tingling.
*L2-L3*
- While L2 contributes to nerves supplying the inguinal region and scrotum (genitofemoral nerve), the **ilioinguinal nerve** originates from L1.
- The **lateral femoral cutaneous nerve**, which originates from L2-L3, innervates the **lateral thigh**, and its injury would cause tingling there, not in the scrotum.
Pelvic floor muscles US Medical PG Question 3: A 58-year-old obese male has noticed the gradual development of a soft bulge on his right groin that has been present over the past year and occasionally becomes very tender. He notices that it comes out when he coughs and strains during bowel movements. He is able to push the bulge back in without issue. After examination, you realize that he has an inguinal hernia and recommend open repair with mesh placement. After surgery, the patient returns to clinic and complains of numbness and tingling in the upper part of the scrotum and base of the penis. What nerve was most likely injured during the procedure?
- A. Ilioinguinal nerve (Correct Answer)
- B. Iliohypogastric nerve
- C. Lateral femoral cutaneous nerve
- D. Obturator nerve
- E. Genitofemoral nerve
Pelvic floor muscles Explanation: **Ilioinguinal nerve**
- The **ilioinguinal nerve** supplies sensory innervation to the skin of the **scrotum** (or labia majora in females), the medial thigh, and the base of the penis.
- Injury to this nerve during an open inguinal hernia repair can cause **numbness and tingling** in these specific areas, consistent with the patient's symptoms.
*Iliohypogastric nerve*
- The **iliohypogastric nerve** primarily provides sensation to the skin over the **suprapubic region** and a small part of the buttock.
- Damage to this nerve would not typically result in numbness of the scrotum or base of the penis.
*Lateral femoral cutaneous nerve*
- This nerve is responsible for sensory innervation of the **lateral aspect of the thigh**.
- Its injury would lead to symptoms of numbness or pain on the lateral thigh (**meralgia paresthetica**), not the scrotum or penis.
*Obturator nerve*
- The **obturator nerve** is a motor nerve that innervates the **adductor muscles of the thigh** and provides sensory innervation to a small area of the medial thigh.
- Damage to this nerve would result in **adductor weakness** and sensory loss in the medial thigh, which does not match the patient's complaints.
*Genitofemoral nerve*
- The **genitofemoral nerve** has two branches: the genital branch (supplies the cremaster muscle and scrotal skin) and the femoral branch (supplies skin of the anterior thigh).
- While the genital branch does innervate the scrotum, injury to this nerve more commonly causes **cremasteric reflex loss** or pain radiating to the anterior thigh, and the described symptoms (base of penis) are more characteristic of ilioinguinal nerve involvement.
Pelvic floor muscles US Medical PG Question 4: One day after undergoing surgery for a traumatic right pelvic fracture, a 73-year-old man has pain over his buttocks and scrotum and urinary incontinence. Physical examination shows right-sided perineal hypesthesia and absence of anal sphincter contraction when the skin around the anus is touched. This patient is most likely to have which of the following additional neurological deficits?
- A. Impaired hip flexion
- B. Paralysis of hip adductors
- C. Absent cremasteric reflex
- D. Impaired psychogenic erection
- E. Absent reflex erection (Correct Answer)
Pelvic floor muscles Explanation: ***Absent reflex erection***
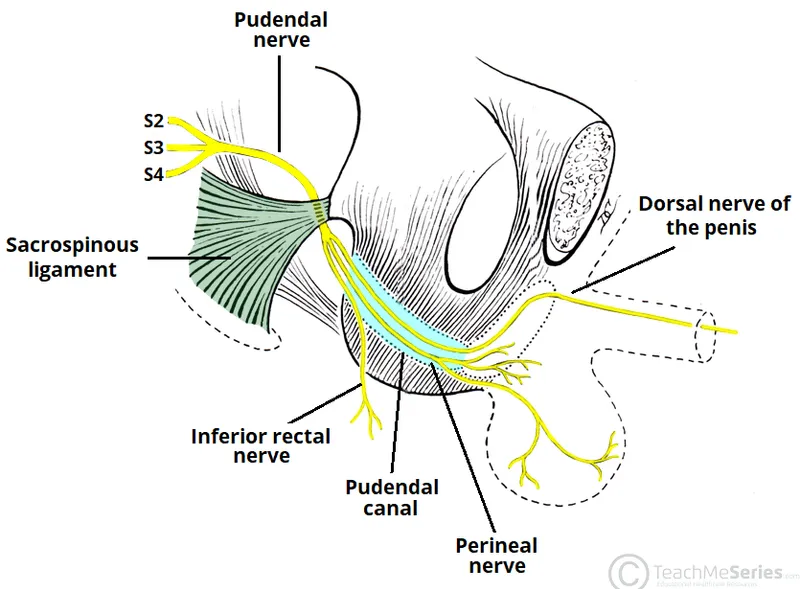
- The patient's symptoms (buttock/scrotal pain, perineal hypesthesia, urinary incontinence, absent anal sphincter contraction) suggest **damage to the sacral plexus and pudendal nerve**, consistent with a **cauda equina syndrome**.
- **Reflex erections** are primarily mediated by the **sacral parasympathetic outflow (S2-S4)**, which are likely compromised given the other sacral nerve deficits.
*Impaired hip flexion*
- **Hip flexion** is primarily controlled by the **L1-L3 nerve roots** (e.g., iliopsoas muscle), and while a severe pelvic fracture could cause widespread nerve damage, the current symptoms localize more strongly to the sacral region.
- The described symptoms are more indicative of **sacral nerve involvement** rather than higher lumbar segments that govern hip flexion.
*Paralysis of hip adductors*
- **Hip adduction** is mainly innervated by the **obturator nerve (L2-L4)**.
- The patient's symptoms point to **S2-S4 nerve dysfunction** (perineal sensation, anal sphincter, bladder), which are distinct from the obturator nerve's primary innervations.
*Absent cremasteric reflex*
- The **cremasteric reflex** is mediated by the **genitofemoral nerve (L1-L2)**.
- The symptoms presented are more consistent with **sacral nerve damage**, specifically S2-S4, rather than the higher lumbar segments responsible for the cremasteric reflex.
*Impaired psychogenic erection*
- **Psychogenic erections** are initiated by **supraspinal input** descending through the thoracolumbar spinal cord (T10-L2) to activate sympathetic pathways.
- While sacral nerve damage can affect the final efferent pathway for all erections, the direct impairment of psychogenic initiation is linked to higher centers and **thoracolumbar sympathetic outflow**, not purely sacral damage.
Pelvic floor muscles US Medical PG Question 5: A 47-year-old man is brought to the emergency department 1 hour after injuring his genital area when he fell astride his backyard fence. He was trimming a tree from the fence when he lost his balance. His vital signs are within normal limits. Examination shows blood at the urethral meatus, perineal ecchymoses, and a scrotal hematoma. An x-ray of the pelvis shows swelling of the soft tissue but no other abnormalities. Which part of the urinary tract is most likely damaged in this patient?
- A. Penile urethra
- B. Bulbous urethra (Correct Answer)
- C. Anterior bladder wall
- D. Prostatic urethra
- E. Membranous urethra
Pelvic floor muscles Explanation: ***Bulbous urethra***
- Straddle injuries (falling astride an object) cause **direct compression of the bulbous urethra** against the inferior pubic ramus
- Classic triad: **blood at urethral meatus, perineal ecchymoses, and scrotal/perineal hematoma** (butterfly pattern)
- The bulbous urethra is part of the **anterior urethra** and is most vulnerable in blunt perineal trauma
- This is a **Buck's fascia injury** with characteristic perineal and scrotal swelling
*Penile urethra*
- More distal portion of anterior urethra within the penis
- Typically injured by **direct penile trauma** (penile fracture, penetrating injury, instrumentation)
- Would not produce the perineal ecchymoses and scrotal hematoma seen in this case
*Membranous urethra*
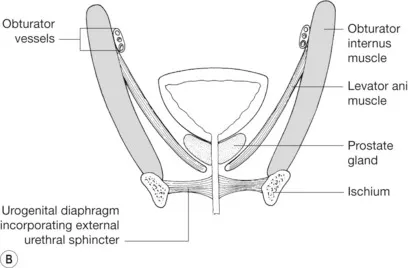
- Part of **posterior urethra** located within the urogenital diaphragm
- Typically injured with **pelvic fractures** (pubic rami fractures), which are absent in this case
- Would present with high-riding prostate on rectal exam and inability to void
*Prostatic urethra*
- Most proximal portion of posterior urethra, well-protected within the prostate
- Injured in **severe pelvic trauma** with disruption of puboprostatic ligaments
- Also associated with pelvic fractures, not straddle injuries
*Anterior bladder wall*
- Requires **pelvic fracture** or penetrating trauma
- Would present with **gross hematuria** and suprapubic pain/tenderness
- Blood at meatus is not typical; more likely to have abdominal distension and peritoneal signs
Pelvic floor muscles US Medical PG Question 6: A 57-year-old woman comes to the physician because of several years of recurrent pelvic pain and constipation. She has increased fecal urgency and a sensation of incomplete evacuation following defecation. She has had no problems associated with urination. Her last menstrual period was 6 years ago. She has had three uncomplicated vaginal deliveries. Physical examination shows normal external genitalia. Speculum examination of the vagina and the cervix shows bulging of the posterior vaginal wall during Valsalva maneuver. Weakness of which of the following structures is the most likely cause of this patient's symptoms?
- A. Cardinal ligament
- B. Uterosacral ligament
- C. Bulbospongiosus muscle
- D. Pubocervical fascia
- E. Rectovaginal fascia (Correct Answer)
Pelvic floor muscles Explanation: ***Rectovaginal fascia***
- The patient's symptoms of recurrent pelvic pain, constipation, increased fecal urgency, and incomplete evacuation, along with **posterior vaginal wall bulging** during Valsalva, are classic signs of a **rectocele**.
- A rectocele results from the weakening or tearing of the **rectovaginal fascia** (also known as the rectovaginal septum), which normally separates the rectum from the vagina and provides support.
*Cardinal ligament*
- The **cardinal ligament** (transverse cervical ligament) primarily provides support to the **cervix and uterus**, preventing uterine prolapse.
- While pelvic organ prolapse is possible, weakness of the cardinal ligament would typically manifest as **uterine prolapse** or anterior vaginal wall bulging (cystocele), not posterior vaginal bulging related to bowel symptoms.
*Uterosacral ligament*
- The **uterosacral ligaments** originate from the cervix and insert into the sacrum, primarily supporting the **uterus and upper vagina**.
- Weakness in these ligaments can contribute to **uterine prolapse** and some forms of vault prolapse after hysterectomy, which are not the primary issues described here.
*Bulbospongiosus muscle*
- The **bulbospongiosus muscle** is part of the superficial perineal pouch and surrounds the vaginal and urethral openings, contributing to **clitoral erection** and tightening the vaginal introitus.
- Weakness of this muscle is not directly associated with rectocele formation or the specific bowel symptoms reported by the patient.
*Pubocervical fascia*
- The **pubocervical fascia** supports the **bladder and urethra**, separating them from the vagina from the front.
- Weakness in this fascia leads to a **cystocele** (prolapse of the bladder into the vagina), which would typically cause urinary symptoms like stress incontinence, not bowel symptoms and posterior vaginal bulging.
Pelvic floor muscles US Medical PG Question 7: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Pelvic floor muscles Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Pelvic floor muscles US Medical PG Question 8: A 26-year-old woman presents to the obstetrics ward to deliver her baby. The obstetrician establishes a pudendal nerve block via intravaginal injection of lidocaine near the tip of the ischial spine. From which of the following nerve roots does the pudendal nerve originate?
- A. L4-L5
- B. S2-S4 (Correct Answer)
- C. L3-L4
- D. L5-S2
- E. L5-S1
Pelvic floor muscles Explanation: ***S2-S4***
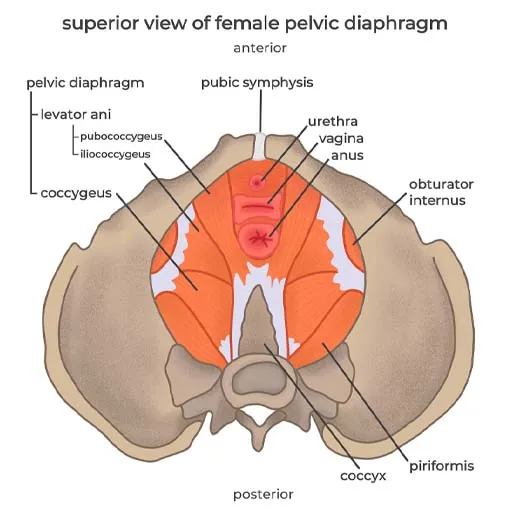
- The **pudendal nerve** originates from the **sacral plexus**, specifically from the ventral rami of spinal nerves **S2, S3, and S4**.
- Its origin from these segments is crucial for its function in innervating structures of the **perineum**, **external genitalia**, and the **anal and urethral sphincters**, making it highly relevant for procedures like **pudendal nerve blocks** during childbirth.
*L4-L5*
- Nerve roots **L4-L5** contribute significantly to the **lumbar plexus** and subsequently to nerves like the **femoral nerve** and portions of the **sciatic nerve**.
- These roots are primarily involved in innervating the **lower limbs** (e.g., quadriceps, tibialis anterior) and are not the primary origin of the pudendal nerve.
*L3-L4*
- The **L3-L4** nerve roots are also part of the **lumbar plexus**, chiefly contributing to the **femoral nerve**.
- They are essential for motor innervation of the **anterior thigh muscles** and sensation in this area, distinct from the pudendal nerve's role in the perineum.
*L5-S2*
- While **S2** is part of the pudendal nerve's origin, the inclusion of **L5** and **S1** primarily characterizes the origin of the **sciatic nerve** (which is formed by L4-S3) and its branches, such as the common fibular and tibial nerves.
- These roots are primarily concerned with the **posterior thigh** and **leg innervation**, not the perineum, which differentiates it from the pudendal nerve.
*L5-S1*
- The nerve roots **L5-S1** are key components of the **lumbosacral plexus** and contribute significantly to the **sciatic nerve**, particularly its innervation of the **hamstrings** and certain lower leg muscles.
- This origin does not align with the known roots of the **pudendal nerve** which stems from S2-S4.
Pelvic floor muscles US Medical PG Question 9: A patient with second-degree cervical prolapse complains of dribbling of urine when coughing. What is the most likely diagnosis?
- A. Cystitis
- B. Stress incontinence (Correct Answer)
- C. Overflow incontinence
- D. Functional incontinence
Pelvic floor muscles Explanation: ***Stress incontinence***
- **Stress incontinence** is characterized by involuntary urine leakage due to increased intra-abdominal pressure (e.g., coughing, sneezing), which is common in association with **pelvic organ prolapse** like a second-degree cervical prolapse.
- The prolapse weakens the **pelvic floor muscles** and supporting structures around the urethra, diminishing its ability to maintain closure during sudden pressure changes.
*Cystitis*
- **Cystitis** is an inflammation of the bladder, typically presenting with symptoms like painful urination (dysuria), frequent urination, and urgency.
- While it can cause bladder irritation, it does not directly lead to urine dribbling with coughing in the absence of other typical infection symptoms.
*Overflow incontinence*
- **Overflow incontinence** occurs due to an **overfilled bladder** that can't empty completely, leading to constant dribbling or leakage.
- This typically results from a **bladder outlet obstruction** or an **underactive detrusor muscle**, not directly from increased abdominal pressure during coughing.
*Functional incontinence*
- **Functional incontinence** is when a person has control over their bladder but cannot reach the toilet in time due to **physical or cognitive impairments**.
- It does not involve a problem with the urinary tract itself but rather with the ability to respond to the urge to urinate.
Pelvic floor muscles US Medical PG Question 10: A 60-year-old post-menopausal female presents to her gynecologist with vaginal bleeding. Her last period was over 10 years ago. Dilation and curettage reveals endometrial carcinoma so she is scheduled to undergo a total abdominal hysterectomy and bilateral salpingo-oophorectomy. During surgery, the gynecologist visualizes paired fibrous structures arising from the cervix and attaching to the lateral pelvic walls at the level of the ischial spines. Which of the following vessels is found within each of the paired visualized structure?
- A. Vaginal artery
- B. Superior vesical artery
- C. Uterine artery (Correct Answer)
- D. Artery of Sampson
- E. Ovarian artery
Pelvic floor muscles Explanation: ***Uterine artery***
- The paired fibrous structures described are the **cardinal ligaments (transverse cervical ligaments)**, which contain the **uterine arteries** as they course towards the uterus.
- The uterine artery, a branch of the **internal iliac artery**, crosses over the **ureter** within the cardinal ligament—a critical anatomical relationship during gynecological surgery ("water under the bridge").
- This is the primary vessel within the cardinal ligament and the key vascular structure at risk during hysterectomy.
*Vaginal artery*
- The vaginal artery typically branches from the **uterine artery** or directly from the **internal iliac artery**, but it is not the main vessel found within the cardinal ligament.
- It primarily supplies the **vagina**, not contained within the cardinal ligament support structure.
*Superior vesical artery*
- The superior vesical artery supplies the **upper part of the bladder** and originates from the **umbilical artery** (a branch of the internal iliac artery).
- It is not anatomically associated with the cardinal ligament or uterine support structures.
*Artery of Sampson*
- The Artery of Sampson is a branch of the **uterine artery** that anastomoses with the **ovarian artery** within the **broad ligament**, not the cardinal ligament.
- It is a minor vessel involved in the dual blood supply to the ovaries and uterus, not a primary structure within the cardinal ligament.
*Ovarian artery*
- The ovarian artery originates directly from the **abdominal aorta** and travels within the **suspensory ligament of the ovary (infundibulopelvic ligament)**, not the cardinal ligament.
- It supplies the **ovaries and fallopian tubes**, with a trajectory that is anatomically distinct from structures within the cardinal ligament.
More Pelvic floor muscles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.