Clinical correlations in pelvis/perineum US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Clinical correlations in pelvis/perineum. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Clinical correlations in pelvis/perineum US Medical PG Question 1: A 33-year-old woman comes to the emergency department because of a 1-hour history of severe pelvic pain and nausea. She was diagnosed with a follicular cyst in the left ovary 3 months ago. The cyst was found incidentally during a fertility evaluation. A pelvic ultrasound with Doppler flow shows an enlarged, edematous left ovary with no blood flow. Laparoscopic evaluation shows necrosis of the left ovary, and a left oophorectomy is performed. During the procedure, blunt dissection of the left infundibulopelvic ligament is performed. Which of the following structures is most at risk of injury during this step of the surgery?
- A. Bladder trigone
- B. Uterine artery
- C. Kidney
- D. Ureter (Correct Answer)
Clinical correlations in pelvis/perineum Explanation: ***Ureter***
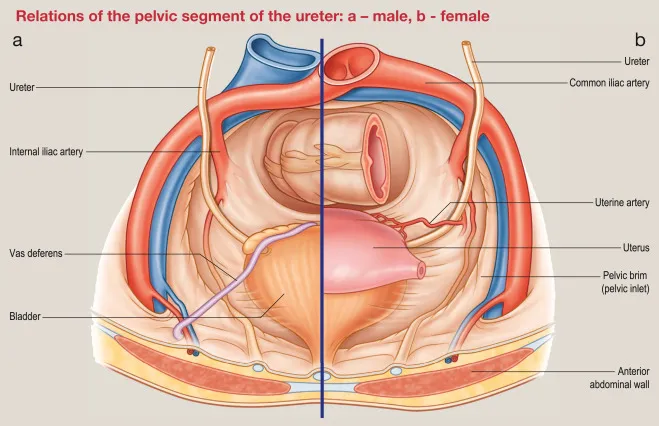
- The **infundibulopelvic ligament** (also known as the suspensory ligament of the ovary) contains the **ovarian artery and vein** and is in close proximity to the ureter as it crosses the pelvic brim.
- During dissection or clamping of this ligament, especially in an emergency setting or when anatomy is distorted (e.g., by an enlarged ovary or edema), the **ureter** is highly susceptible to injury.
*Bladder trigone*
- The **bladder trigone** is the smooth triangular region at the base of the bladder, formed by the openings of the ureters and the internal urethral orifice.
- It is not directly adjacent to the infundibulopelvic ligament and is therefore at a comparably lower risk of injury during dissection of this ligament.
*Uterine artery*
- The **uterine artery** travels within the cardinal ligament and supplies the uterus; it is located more medially and inferiorly within the broad ligament.
- While important in pelvic surgery, it is not in the immediate vicinity of the infundibulopelvic ligament dissection itself.
*Kidney*
- The **kidneys** are retroperitoneal organs located much higher in the abdominal cavity, far superior to the pelvis.
- They are not at risk of direct injury during pelvic surgery involving the infundibulopelvic ligament.
Clinical correlations in pelvis/perineum US Medical PG Question 2: A 67-year-old man comes to the physician because of a 3-month history of difficulty initiating urination. He wakes up at least 3–4 times at night to urinate. Digital rectal examination shows a symmetrically enlarged, nontender prostate with a rubbery consistency. Laboratory studies show a prostate-specific antigen level of 2.1 ng/mL (N < 4). Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Lymphocytic infiltration of anterior prostatic lobe stroma
- B. Hyperplasia of lateral prostatic lobe tissue
- C. Infiltrating dysplasia of posterior prostatic lobe epithelium
- D. Infiltrating neoplasia of bladder urothelium
- E. Hypertrophy of middle prostatic lobe tissue (Correct Answer)
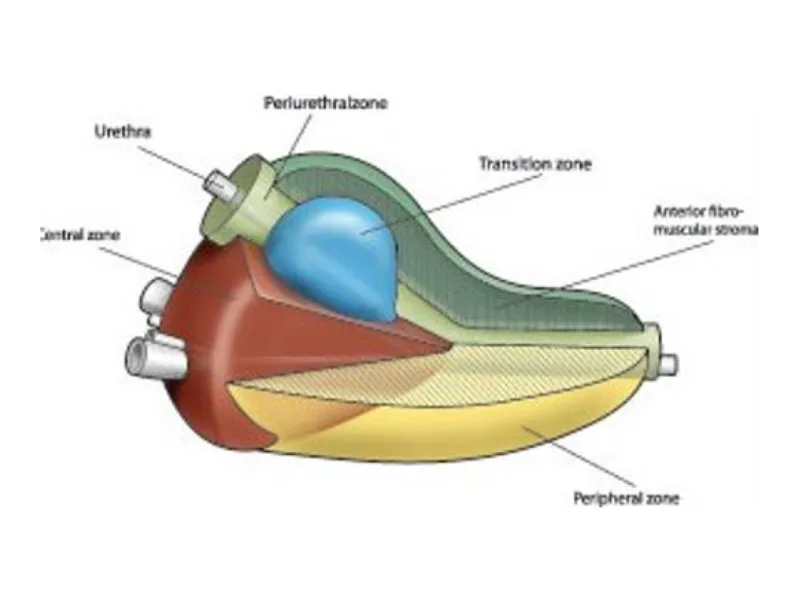
Clinical correlations in pelvis/perineum Explanation: ***Hypertrophy of middle prostatic lobe tissue***
- This patient's symptoms of **difficulty initiating urination** and **nocturia** are classic for **benign prostatic hyperplasia (BPH)**.
- The **middle lobe** enlargement is particularly significant because it can **protrude into the bladder neck**, directly causing **urethral obstruction** and the obstructive voiding symptoms seen here.
- The digital rectal exam finding of a **symmetrically enlarged, nontender prostate** with a **rubbery consistency** is characteristic of BPH.
- The **normal PSA level** (2.1 ng/mL) supports a benign process.
*Lymphocytic infiltration of anterior prostatic lobe stroma*
- **Lymphocytic infiltration** of the prostate is consistent with **prostatitis**, which would typically present with **pain, fever, and dysuria**, not just obstructive symptoms.
- The **nontender prostate** on examination argues against prostatitis.
*Hyperplasia of lateral prostatic lobe tissue*
- While **lateral lobe hyperplasia** (transition zone) is the **most common finding in BPH**, this option is less specific to the obstructive symptoms described.
- BPH typically involves both lateral and middle lobes, but **middle lobe** enlargement more directly causes **bladder outlet obstruction** by protruding into the bladder neck.
- Lateral lobe hyperplasia causes obstruction by compressing the prostatic urethra but is less likely to cause the severe obstructive symptoms without middle lobe involvement.
*Infiltrating dysplasia of posterior prostatic lobe epithelium*
- **Dysplasia** in the posterior lobe (peripheral zone) suggests a **premalignant condition** or **early prostate cancer**, which would more likely cause an **asymmetric, firm, or nodular prostate** on DRE.
- The **normal PSA** and **benign examination findings** do not suggest malignancy.
*Infiltrating neoplasia of bladder urothelium*
- **Bladder cancer** typically presents with **painless hematuria** as its primary symptom, which is not mentioned here.
- The **DRE findings** of prostatic enlargement point to prostatic, not bladder, pathology.
Clinical correlations in pelvis/perineum US Medical PG Question 3: A 56-year-old man comes to the clinic complaining of sexual dysfunction. He reports normal sexual function until 4 months ago when his relationship with his wife became stressful due to a death in the family. When asked about the details of his dysfunction, he claims that he is “able to get it up, but just can’t finish the job.” He denies any decrease in libido or erections, endorses morning erections, but an inability to ejaculate. He is an avid cyclist and exercises regularly. His past medical history includes depression and diabetes, for which he takes citalopram and metformin, respectively. A physical examination is unremarkable. What is the most likely explanation for this patient’s symptoms?
- A. Testosterone deficiency
- B. Autonomic neuropathy secondary to systemic disease
- C. Psychological stress
- D. Damage to the pudendal nerve
- E. Medication side effect (Correct Answer)
Clinical correlations in pelvis/perineum Explanation: ***Medication side effect***
- The patient's inability to ejaculate while maintaining normal libido, erections, and morning erections is highly suggestive of **ejaculatory dysfunction** caused by the **citalopram**, a selective serotonin reuptake inhibitor (SSRI).
- SSRIs, like citalopram, are known to commonly cause sexual side effects, including **delayed ejaculation** and **anorgasmia**, by increasing serotonin levels, which can inhibit the ejaculatory reflex.
*Testosterone deficiency*
- Testosterone deficiency usually presents with **decreased libido**, **erectile dysfunction**, and a reduction in **morning erections**, which are not reported by this patient.
- While it can impact sexual function, the specific symptom of inability to ejaculate with preserved erections points away from low testosterone.
*Autonomic neuropathy secondary to systemic disease*
- **Autonomic neuropathy**, often seen in patients with **diabetes**, can lead to ejaculatory dysfunction, including **retrograde ejaculation**.
- However, the patient's normal erections and libido, along with the recent onset coinciding with a stressful event and medication use, make medication a more likely primary cause in this scenario.
*Psychological stress*
- **Psychological stress** can certainly contribute to sexual dysfunction, leading to decreased libido or erectile difficulties.
- However, the patient explicitly states his erections and libido are normal, and he only experiences an inability to ejaculate, which is less commonly the sole manifestation of stress.
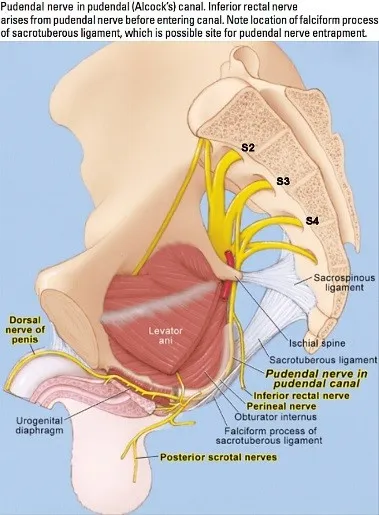
*Damage to the pudendal nerve*
- **Pudendal nerve damage** typically results in issues with **erectile function**, sensation in the perineum, and potentially urinary or fecal incontinence.
- This patient's preserved erections and specific issue with ejaculation make pudendal nerve damage an unlikely primary cause.
Clinical correlations in pelvis/perineum US Medical PG Question 4: A 42-year-old woman, gravida 5, para 5, comes to the physician because of a 6-month history of occasional involuntary urine loss that is exacerbated by coughing, sneezing, and laughing. She has no urgency or dysuria. Physical examination shows normal appearing external genitalia, vagina, and cervix. There is a loss of urine with the Valsalva maneuver. The physician recommends doing Kegel exercises. Which of the following muscles is strengthened by these exercises?
- A. Sphincter urethrae
- B. Compressor urethrae
- C. Levator ani (Correct Answer)
- D. Deep transverse perineal muscles
- E. Internal urethral sphincter
Clinical correlations in pelvis/perineum Explanation: ***Levator ani***
- **Kegel exercises** primarily target and strengthen the **levator ani muscles**, which are a crucial component of the **pelvic floor**.
- A strong pelvic floor, particularly the levator ani, provides support to the urethra and bladder neck, preventing **stress urinary incontinence** during increased intra-abdominal pressure.
*Sphincter urethrae*
- The **sphincter urethrae** (external urethral sphincter) contributes to voluntary urine control but is not the primary muscle strengthened by Kegel exercises; it works synergistically with the levator ani.
- While it helps in continence, its strengthening is typically secondary to exercises targeting the broader pelvic floor musculature.
*Compressor urethrae*
- The **compressor urethrae** is a part of the external urethral sphincter complex in females but is a smaller, accessory muscle.
- Its specific strengthening is not the main goal or direct outcome of general Kegel exercises, which focus on the larger pelvic floor muscles.
*Deep transverse perineal muscles*
- These muscles form part of the **urogenital diaphragm** but are not the principal muscles targeted by Kegel exercises for stress incontinence.
- They provide support to the perineum but have a less direct role in urethral continence compared to the levator ani.
*Internal urethral sphincter*
- The **internal urethral sphincter** is composed mainly of **smooth muscle** and is under **involuntary control** by the autonomic nervous system.
- Therefore, it cannot be directly strengthened through voluntary exercises like Kegel exercises.
Clinical correlations in pelvis/perineum US Medical PG Question 5: A 76-year-old female with a past medical history of obesity, coronary artery disease status post stent placement, hypertension, hyperlipidemia, and insulin dependent diabetes comes to your outpatient clinic for regular checkup. She has not been very adherent to her diabetes treatment regimen. She has not been checking her sugars regularly and frequently forgets to administer her mealtime insulin. Her Hemoglobin A1c three months ago was 14.1%. As a result of her diabetes, she has developed worsening diabetic retinopathy and neuropathy. Based on her clinical presentation, which of the following is the patient most at risk for developing?
- A. Stress incontinence
- B. Hemorrhoids
- C. Rectal prolapse
- D. Overflow incontinence (Correct Answer)
- E. Uterine prolapse
Clinical correlations in pelvis/perineum Explanation: ***Overflow incontinence***
- The patient's **poorly controlled diabetes** can lead to **diabetic autonomic neuropathy**, affecting bladder function and causing **neurogenic bladder**.
- This results in the bladder not emptying completely, leading to **urinary retention** and leakage as the bladder overfills, which defines **overflow incontinence**.
*Stress incontinence*
- This type of incontinence is typically caused by **weakening of pelvic floor muscles** and **urethral sphincter**, leading to leakage with increased abdominal pressure (e.g., coughing, sneezing).
- While obesity is a risk factor, the patient's severe, uncontrolled diabetes points more strongly to neuropathy affecting bladder emptying rather than just sphincter weakness.
*Hemorrhoids*
- Hemorrhoids are **swollen veins in the rectum or anus**, often associated with straining during bowel movements, chronic constipation, or obesity.
- While common in this demographic, there is no direct link between uncontrolled diabetes and the development of hemorrhoids.
*Rectal prolapse*
- Rectal prolapse involves the **protrusion of the rectum through the anus**, often due to weakened pelvic floor muscles or chronic straining.
- Although the patient's age and obesity could be contributing factors, poorly controlled diabetes does not directly cause rectal prolapse.
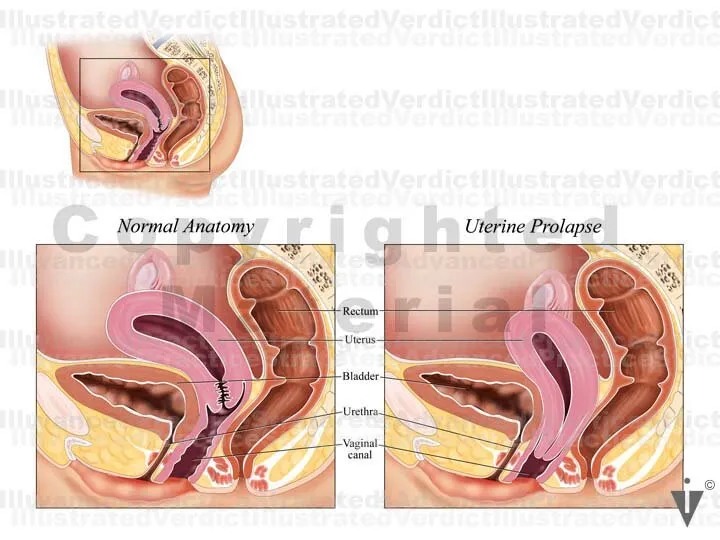
*Uterine prolapse*
- Uterine prolapse occurs when the **uterus descends into the vagina**, typically due to weakened pelvic floor muscles, often following childbirth or with age and obesity.
- Uncontrolled diabetes does not directly cause uterine prolapse, although shared risk factors like obesity might be present.
Clinical correlations in pelvis/perineum US Medical PG Question 6: A 42-year-old woman comes to the physician because of right flank pain that started 3 days following a procedure. Her vital signs are within normal limits. Physical examination shows right costovertebral angle tenderness. An intravenous pyelogram shows a dilated renal pelvis and ureter on the right with a lack of contrast proximal to the ureterovesical junction. This patient most likely recently underwent which of the following procedures?
- A. Hysterectomy (Correct Answer)
- B. Foley catheter insertion
- C. Cesarean delivery
- D. Appendectomy
- E. Inguinal hernia repair
Clinical correlations in pelvis/perineum Explanation: ***Hysterectomy***
- **Ureteral injury** is a known complication of hysterectomy due to the ureter's close proximity to the uterine arteries and adnexa, especially near the **ureterovesical junction**.
- The presented symptoms of flank pain, CVA tenderness, and hydronephrosis (dilated renal pelvis and ureter with lack of contrast flow) occurring post-procedure strongly indicate **ureteral obstruction** or injury during the surgery.
*Foley catheter insertion*
- While catheterization can cause trauma, it would typically lead to **urethral or bladder injury**, not a ureteral obstruction at the ureterovesical junction causing hydronephrosis.
- The symptoms are more consistent with an injury higher up in the urinary tract that is not usually associated with a Foley catheter.
*Cesarean delivery*
- A C-section involves opening the abdomen to deliver a baby, but it generally does not involve dissection near the ureters to the extent that a hysterectomy does, making ureteral injury less common.
- The primary surgical field during a C-section is the uterus, while ureteral injury is more characteristic of procedures involving extensive pelvic dissection, such as hysterectomy.
*Appendectomy*
- An appendectomy is a procedure to remove the appendix and typically involves the right lower quadrant of the abdomen, away from the course of the ureter and ureterovesical junction.
- Injury to the ureter is a very rare complication of appendectomy and would not typically manifest as this type of obstruction.
*Inguinal hernia repair*
- Inguinal hernia repair involves structures in the groin region, anterior to the peritoneal cavity, and is far removed from the ureters and bladder.
- Ureteral injury is not a recognized complication of inguinal hernia repair.
Clinical correlations in pelvis/perineum US Medical PG Question 7: A 60-year-old post-menopausal female presents to her gynecologist with vaginal bleeding. Her last period was over 10 years ago. Dilation and curettage reveals endometrial carcinoma so she is scheduled to undergo a total abdominal hysterectomy and bilateral salpingo-oophorectomy. During surgery, the gynecologist visualizes paired fibrous structures arising from the cervix and attaching to the lateral pelvic walls at the level of the ischial spines. Which of the following vessels is found within each of the paired visualized structure?
- A. Vaginal artery
- B. Superior vesical artery
- C. Uterine artery (Correct Answer)
- D. Artery of Sampson
- E. Ovarian artery
Clinical correlations in pelvis/perineum Explanation: ***Uterine artery***
- The paired fibrous structures described are the **cardinal ligaments (transverse cervical ligaments)**, which contain the **uterine arteries** as they course towards the uterus.
- The uterine artery, a branch of the **internal iliac artery**, crosses over the **ureter** within the cardinal ligament—a critical anatomical relationship during gynecological surgery ("water under the bridge").
- This is the primary vessel within the cardinal ligament and the key vascular structure at risk during hysterectomy.
*Vaginal artery*
- The vaginal artery typically branches from the **uterine artery** or directly from the **internal iliac artery**, but it is not the main vessel found within the cardinal ligament.
- It primarily supplies the **vagina**, not contained within the cardinal ligament support structure.
*Superior vesical artery*
- The superior vesical artery supplies the **upper part of the bladder** and originates from the **umbilical artery** (a branch of the internal iliac artery).
- It is not anatomically associated with the cardinal ligament or uterine support structures.
*Artery of Sampson*
- The Artery of Sampson is a branch of the **uterine artery** that anastomoses with the **ovarian artery** within the **broad ligament**, not the cardinal ligament.
- It is a minor vessel involved in the dual blood supply to the ovaries and uterus, not a primary structure within the cardinal ligament.
*Ovarian artery*
- The ovarian artery originates directly from the **abdominal aorta** and travels within the **suspensory ligament of the ovary (infundibulopelvic ligament)**, not the cardinal ligament.
- It supplies the **ovaries and fallopian tubes**, with a trajectory that is anatomically distinct from structures within the cardinal ligament.
Clinical correlations in pelvis/perineum US Medical PG Question 8: A 32-year-old man comes to the physician because of episodic tingling and numbness in his right hand for the past 3 months. His symptoms are worse in the evening. There is no history of trauma. He is employed as a carpenter. He has smoked 1 pack of cigarettes daily for the past 10 years. He drinks a pint of vodka daily. He does not use illicit drugs. His vital signs are within normal limits. Physical examination shows decreased pinch strength in the right hand. Sensations are decreased over the little finger and both the dorsal and palmar surfaces of the medial aspect of the right hand. Which of the following is the most likely site of nerve compression?
- A. Guyon canal
- B. Quadrilateral space
- C. Carpal tunnel
- D. Cubital tunnel (Correct Answer)
- E. Radial groove
Clinical correlations in pelvis/perineum Explanation: ***Cubital tunnel***
- Compression of the **ulnar nerve** at the cubital tunnel typically presents with paresthesias and numbness in the **little finger** and medial half of the ring finger, along with weakness in **intrinsic hand muscles** (decreased pinch strength).
- The carpenter's occupation may involve repetitive elbow flexion, exacerbating **ulnar nerve compression** at the elbow.
*Guyon canal*
- Compression in the **Guyon canal** affects the **ulnar nerve** at the wrist.
- While it can cause similar sensory and motor deficits in the hand, the cubital tunnel is a more common site of compression for the ulnar nerve, and symptoms worsen with **elbow flexion**.
*Carpal tunnel*
- **Carpal tunnel syndrome** involves compression of the **median nerve** and causes numbness and tingling in the thumb, index, middle, and radial half of the ring finger, sparing the little finger.
- It does not cause decreased sensation over the **little finger**.
*Quadrilateral space*
- **Quadrilateral space syndrome** involves compression of the **axillary nerve** and presents with shoulder pain, paresthesias over the lateral shoulder, and weakness in abduction and external rotation.
- This does not align with the patient's hand symptoms.
*Radial groove*
- Compression of the **radial nerve** in the radial groove (spiral groove) of the humerus typically results in **wrist drop**, weakness in forearm and hand extensors, and sensory loss over the dorsum of the hand, not the ulnar distribution described.
- This is not consistent with the patient's sensory and motor deficits.
Clinical correlations in pelvis/perineum US Medical PG Question 9: A 19-year-old man is brought to the emergency department following a high-speed motor vehicle collision in which he was a restrained passenger. He complains of pelvic pain and urinary retention with overflow incontinence, along with associated lower extremity weakness. Examination shows perineal bruising and there is pain with manual compression of the pelvis. Injury to which of the following structures is most likely responsible for this patient's urinary incontinence?
- A. Ilioinguinal nerve
- B. Obturator nerve
- C. Genitofemoral nerve
- D. Pelvic splanchnic nerves (Correct Answer)
- E. Superior gluteal nerve
Clinical correlations in pelvis/perineum Explanation: ***Pelvic splanchnic nerves***
- Urinary retention with overflow incontinence and lower extremity weakness following a pelvic trauma suggests damage to the **sacral spinal segments** or the **pelvic splanchnic nerves**.
- These nerves carry **parasympathetic fibers** that stimulate bladder contraction (detrusor muscle) and relaxation of the internal urethral sphincter, which are crucial for normal micturition.
*Ilioinguinal nerve*
- This nerve supplies sensory innervation to the **genitalia** and part of the inner thigh, and motor innervation to the internal oblique and transversus abdominis muscles.
- Damage to this nerve would primarily cause sensory deficits or abdominal muscle weakness, not urinary retention or lower extremity weakness.
*Obturator nerve*
- The obturator nerve primarily innervates the **adductor muscles of the thigh** and provides sensory innervation to the medial thigh.
- Injury would result in difficulty with hip adduction and sensory loss in the medial thigh, not bladder dysfunction or diffuse lower extremity weakness.
*Genitofemoral nerve*
- This nerve provides sensory innervation to the **anterior compartment of the thigh** and the external genitalia, and motor innervation to the cremaster muscle.
- Damage would typically manifest as altered sensation in these areas or an absent cremasteric reflex, without directly affecting bladder function.
*Superior gluteal nerve*
- The superior gluteal nerve innervates the **gluteus medius, gluteus minimus, and tensor fasciae latae muscles**, which are crucial for hip abduction and stabilization during walking.
- Injury would lead to a characteristic **Trendelenburg gait**, but would not directly cause urinary incontinence or retention.
Clinical correlations in pelvis/perineum US Medical PG Question 10: A slipped disc at the level shown in the image would most likely involve which nerve root?
- A. L4
- B. L5 (Correct Answer)
- C. S1
- D. L3
- E. L2
Clinical correlations in pelvis/perineum Explanation: ***L5***
- The image shows a **disc herniation** at the L4-L5 level. In cases of disc herniation, it is the **nerve root exiting below the level of the disc** that is typically compressed.
- For an L4-L5 disc herniation, the **L5 nerve root** is the one most commonly affected because it passes directly behind the L4 vertebral body and the L4-L5 disc before exiting the neural foramen at the L5-S1 level.
*L4*
- An L4 nerve root compression would typically occur with a disc herniation at the **L3-L4 level**. The L4 nerve root usually exits above the L4-L5 disc.
- While sometimes L4 nerve root can be involved in a massive central L4-L5 herniation, it is less common than L5 involvement for a typical posterolateral herniation at this level.
*S1*
- The S1 nerve root would be involved in a **disc herniation at the L5-S1 level**, as it exits below the L5-S1 disc.
- The disc herniation visible in the image is clearly above the L5-S1 intervertebral space.
*L3*
- Compression of the L3 nerve root usually results from a disc herniation at the **L2-L3 level**, which is higher than the level depicted in the image.
- The L3 nerve root is anatomically shielded from an L4-L5 disc herniation.
*L2*
- The L2 nerve root would be affected by a disc herniation at the **L1-L2 level**, which is significantly higher than the level shown in the image.
- L2 nerve root involvement would present with different clinical features (primarily hip flexion weakness and sensory changes in the anterior thigh).
More Clinical correlations in pelvis/perineum US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.