Respiratory system histology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Respiratory system histology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Respiratory system histology US Medical PG Question 1: A 10-year-old boy is brought to the physician by his mother because of a 2-day history of fever and productive cough. He has had similar episodes sporadically in the past with frequent episodes of thick, discolored nasal discharge. Physical examination shows diffuse crackles and rhonchi. The most likely cause of recurrent infections in this patient is a dysfunction of which of the following cell types?
- A. Type I pneumocytes
- B. Club cells
- C. Alveolar macrophages
- D. Type II pneumocytes
- E. Ciliated columnar cells (Correct Answer)
Respiratory system histology Explanation: ***Ciliated columnar cells***
- The patient's presentation with **recurrent respiratory infections**, productive cough, and thick nasal discharge suggests a defect in mucociliary clearance, which is primarily mediated by **ciliated columnar cells**.
- Conditions like **primary ciliary dyskinesia** involve dysfunctional cilia unable to clear mucus and pathogens, leading to chronic infections.
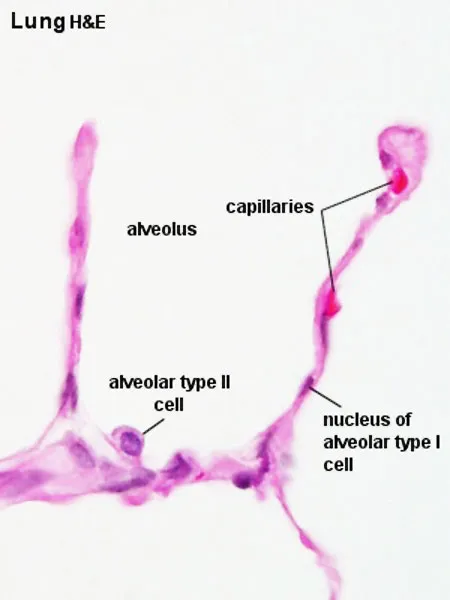
*Type I pneumocytes*
- These cells are responsible for **gas exchange** in the alveoli due to their thin, flat structure.
- Dysfunction of type I pneumocytes would primarily lead to **respiratory distress** and impaired oxygenation, not recurrent infections.
*Club cells*
- **Club cells** (formerly Clara cells) are found in the bronchioles and secrete components of the surfactant and detoxify harmful substances.
- While they contribute to airway defense, their primary role is not mucociliary clearance, and their dysfunction is less likely to cause recurrent productive cough and thick nasal discharge.
*Alveolar macrophages*
- **Alveolar macrophages** are crucial for phagocytosing inhaled particles and pathogens within the alveoli.
- Dysfunction of these cells would likely result in increased susceptibility to **pneumonia** and more severe lower respiratory tract infections, but is not typically associated with chronic productive cough and nasal discharge suggesting a primary mucociliary defect.
*Type II pneumocytes*
- **Type II pneumocytes** produce **surfactant** to reduce alveolar surface tension and are progenitors for type I pneumocytes.
- Dysfunction primarily leads to **atelectasis** and reduced lung compliance, not recurrent bacterial infections associated with impaired clearance.
Respiratory system histology US Medical PG Question 2: A baby is born after the 32nd gestational week by cesarean delivery. The mother suffered from gestational diabetes; however, she had no other pregnancy-related diseases and was otherwise healthy. The baby has a blood pressure of 100/58 mm Hg, heart rate of 104/min, and oxygen saturation of 88%. The child has tachypnea, subcostal and intercostal retractions, nasal flaring, and cyanosis. The cyanosis is responding well to initial administration of oxygen. The nasogastric tube was positioned without problems. Which of the following is the most likely diagnosis?
- A. Tracheoesophageal fistula
- B. Pneumonia
- C. Neonatal respiratory distress syndrome (NRDS) (Correct Answer)
- D. Sepsis
- E. Congenital heart anomaly with right-to-left shunt
Respiratory system histology Explanation: ***Neonatal respiratory distress syndrome (NRDS)***
- The premature birth (32nd week), presence of **tachypnea**, **retractions**, **nasal flaring**, **cyanosis** responding to oxygen, and maternal **gestational diabetes** are all highly suggestive of NRDS.
- Maternal gestational diabetes can delay fetal lung maturity, increasing the risk of **surfactant deficiency**, which is the primary cause of NRDS.
*Tracheoesophageal fistula*
- This condition typically presents with **choking**, **coughing**, and **regurgitation** during feeding, often with inability to pass a nasogastric tube into the stomach.
- The successful positioning of the **nasogastric tube** makes this diagnosis less likely.
*Pneumonia*
- While pneumonia can cause respiratory distress, the **early onset** in a premature infant with maternal gestational diabetes points more strongly towards **NRDS**.
- Pneumonia would typically have signs of **infection** such as fever, though early neonatal pneumonia can be atypical.
*Sepsis*
- Sepsis can cause respiratory distress, but it's usually accompanied by other signs of systemic infection, such as **fever or hypothermia**, **lethargy**, and poor feeding and often signs of **circulatory compromise**.
- The clinical picture provided primarily points towards a respiratory rather than a systemic infectious cause primarily.
*Congenital heart anomaly with right-to-left shunt*
- While this can cause **cyanosis** and respiratory distress, the prompt response to oxygen management makes a significant right-to-left shunt less likely.
- A significant right-to-left shunt would typically cause **cyanosis** that is refractory to oxygen administration.
Respiratory system histology US Medical PG Question 3: In which of the following pathological states would the oxygen content of the trachea resemble the oxygen content in the affected alveoli?
- A. Emphysema
- B. Exercise
- C. Pulmonary embolism (Correct Answer)
- D. Pulmonary fibrosis
- E. Foreign body obstruction distal to the trachea
Respiratory system histology Explanation: ***Pulmonary embolism***
- A pulmonary embolism blocks **blood flow** to a portion of the lung, creating **dead space ventilation** (high V/Q ratio).
- In the affected alveoli, **no blood perfusion** means no oxygen extraction occurs, so the alveolar oxygen content remains **high and similar to tracheal/inspired air**.
- This is the classic physiological state where ventilation continues but perfusion is absent, preventing gas exchange.
*Foreign body obstruction distal to the trachea*
- A complete obstruction **prevents fresh air** from reaching the affected alveoli.
- The trapped gas undergoes **resorption atelectasis**: oxygen is absorbed into capillary blood, CO2 diffuses in, and alveolar gas equilibrates with **venous blood** composition.
- Alveolar oxygen content becomes **very low**, not similar to tracheal air.
*Emphysema*
- Emphysema involves destruction of **alveolar walls** and enlargement of airspaces with impaired gas exchange.
- While V/Q mismatch occurs, oxygen is still extracted by perfusing blood.
- Alveolar oxygen content is **lower than tracheal air** due to ongoing (though inefficient) gas exchange.
*Exercise*
- During exercise, **oxygen consumption increases** dramatically with enhanced cardiac output and oxygen extraction.
- Alveolar oxygen content is **significantly lower** than tracheal air due to increased oxygen uptake by blood.
*Pulmonary fibrosis*
- Pulmonary fibrosis causes **thickening of the alveolar-capillary membrane**, impairing oxygen diffusion.
- Despite diffusion limitation, blood still perfuses the alveoli and extracts oxygen.
- Alveolar oxygen content is **lower than tracheal air**, though the A-a gradient is increased.
Respiratory system histology US Medical PG Question 4: A 21-year-old lacrosse player comes to the doctor for an annual health assessment. She does not smoke or drink alcohol. She is 160 cm (5 ft 3 in) tall and weighs 57 kg (125 lb); BMI is 22 kg/m2. Pulmonary function tests show an FEV1 of 90% and an FVC of 3600 mL. Whole body plethysmography is performed to measure airway resistance. Which of the following structures of the respiratory tree is likely to have the highest contribution to total airway resistance?
- A. Conducting bronchioles
- B. Terminal bronchioles
- C. Segmental bronchi (Correct Answer)
- D. Respiratory bronchioles
- E. Mainstem bronchi
Respiratory system histology Explanation: ***Segmental bronchi***
- In healthy individuals, **medium-sized bronchi** (including segmental and subsegmental bronchi, approximately generations 4-8) contribute approximately **80% of total airway resistance**.
- While **Poiseuille's Law** states resistance is inversely proportional to radius to the fourth power (R ∝ 1/r⁴), the key factor is the **total cross-sectional area** and **degree of branching**.
- Medium-sized bronchi have moderate individual resistance and **limited parallel branching**, making them the dominant site of resistance.
- This is why diseases affecting medium-sized airways (e.g., asthma, bronchitis) cause significant increases in airway resistance.
*Terminal bronchioles*
- Although individual terminal bronchioles have small radii and high individual resistance, there are **millions of them arranged in parallel**.
- With parallel resistances, total resistance decreases: 1/R_total = 1/R₁ + 1/R₂ + 1/R₃...
- The **massive number** of small airways means their collective resistance is actually quite **low** (~10-20% of total).
- This is why small airways disease is called the "**silent zone**" - significant pathology can occur before detection.
*Conducting bronchioles*
- These airways also benefit from extensive **parallel branching**, reducing their contribution to total resistance.
- They contribute less than medium-sized bronchi due to their large cumulative cross-sectional area.
*Respiratory bronchioles*
- Part of the **respiratory zone** with the largest total cross-sectional area in the lungs.
- Minimal contribution to airway resistance due to enormous parallel arrangement.
- Primary function is **gas exchange**, not air conduction.
*Mainstem bronchi*
- These large airways have **low individual resistance** due to large diameter.
- Together with the trachea, they contribute approximately **20% of total airway resistance**.
- Not the primary site despite being early in the airway tree.
Respiratory system histology US Medical PG Question 5: A 44-year-old man comes to the physician because of a 5-month history of persistent cough productive of thick, yellow sputum and worsening shortness of breath. One year ago, he had similar symptoms that lasted 4 months. He has smoked two packs of cigarettes daily for the past 20 years. Physical examination shows scattered expiratory wheezing and rhonchi throughout both lung fields. Microscopic examination of a lung biopsy specimen is most likely to show which of the following findings?
- A. Decreased smooth muscle cells
- B. Decreased alveolar macrophages
- C. Increased ciliated epithelial cells
- D. Increased goblet cells (Correct Answer)
- E. Increased club cells
Respiratory system histology Explanation: **Increased goblet cells**
- This patient's presentation of persistent cough with thick, yellow sputum, worsening shortness of breath, and a history of heavy smoking points towards **chronic bronchitis**.
- **Chronic bronchitis** is pathologically defined by **mucus gland hyperplasia** and **goblet cell hypertrophy** in the bronchial airways, leading to excessive mucus production.
*Decreased smooth muscle cells*
- Airway smooth muscle can undergo **hyperplasia** and **hypertrophy** in chronic obstructive pulmonary diseases (COPD) like chronic bronchitis, rather than a decrease.
- A decrease in smooth muscle cells is not a characteristic pathological finding in chronic bronchitis.
*Decreased alveolar macrophages*
- **Alveolar macrophages** are crucial for clearing inhaled particles and pathogens and are typically **increased** or functionally altered in chronic inflammatory lung conditions.
- A decrease in these immune cells would not be a typical finding in chronic bronchitis and would likely lead to increased susceptibility to infections.
*Increased ciliated epithelial cells*
- In chronic bronchitis, there is often a **loss of ciliated epithelial cells** as they are replaced by **goblet cells** and undergo **squamous metaplasia** due to chronic irritation.
- The remaining ciliated cells may be dysfunctional, impairing mucociliary clearance.
*Increased club cells*
- **Club cells** (formerly Clara cells) are non-ciliated, secretory cells found in the small airways that protect the bronchiolar epithelium.
- While they play a role in airway defense, their significant increase is not a primary or characteristic pathological feature of chronic bronchitis.
Respiratory system histology US Medical PG Question 6: A 38-year-old man comes to the clinic complaining of recurrent abdominal pain for the past 2 months. He reports a gnawing, dull pain at the epigastric region that improves with oral ingestion. He has been taking calcium carbonate for the past few weeks; he claims that “it used to help a lot but it’s losing its effects now.” Laboratory testing demonstrated increased gastrin levels after the administration of secretin. A push endoscopy visualized several ulcers at the duodenum and proximal jejunum. What characteristics distinguish the jejunum from the duodenum?
- A. Lack of goblet cells
- B. Crypts of Lieberkuhn
- C. Lack of submucosal Brunner glands (Correct Answer)
- D. Peyer patches
- E. Plicae circulares
Respiratory system histology Explanation: ***Lack of submucosal Brunner glands***
- The **jejunum** lacks **Brunner glands**, which are characteristic of the **duodenum** and secrete alkaline mucus to neutralize acidic chyme from the stomach.
- The absence of these glands helps differentiate the jejunum from the duodenum histologically.
*Lack of goblet cells*
- **Goblet cells** are present throughout the small intestine, including both the duodenum and jejunum, though their density increases distally.
- Therefore, the **lack of goblet cells** does not distinguish the jejunum from the duodenum.
*Crypts of Lieberkuhn*
- **Crypts of Lieberkuhn** (intestinal crypts) are present throughout the entire small intestine, including both the **duodenum** and **jejunum**, where they house stem cells for epithelial renewal.
- Their presence is not a distinguishing feature between these two segments histologically.
*Peyer patches*
- **Peyer patches** are lymphoid aggregates primarily found in the **ileum**, not the jejunum or duodenum, and are involved in immune surveillance.
- They are a distinguishing feature of the ileum but not between the jejunum and duodenum.
*Plicae circulares*
- **Plicae circulares** (also known as valves of Kerckring or circular folds) are macroscopic folds of the mucosa and submucosa that are present in both the **duodenum** and **jejunum**.
- They are most prominent in the jejunum, but their mere presence does not distinguish the jejunum from the duodenum.
Respiratory system histology US Medical PG Question 7: A 55-year-old man comes to the physician because of heartburn for the past 2 years. He has no chest pain, dysphagia, weight loss, or fever. He has no history of any serious illnesses. He takes omeprazole daily. Vital signs are within normal limits. Body mass index (BMI) is 34 kg/m2. Physical exam shows no abnormalities. An endoscopic image of the lower esophageal sphincter is shown. Which of the following is the most important next step in management?
- A. Endoscopic mucosal ablation therapy
- B. Esophagectomy
- C. High-dose pantoprazole
- D. Multiple endoscopic biopsies (Correct Answer)
- E. Laparoscopic Nissen fundoplication
Respiratory system histology Explanation: ***Multiple endoscopic biopsies***
- The endoscopic image likely shows **Barrett's esophagus**, characterized by metaplastic columnar epithelium. This condition is a precursor to **esophageal adenocarcinoma**.
- **Biopsies** are crucial to assess for the presence and grade of **dysplasia**, which dictates further management strategies.
*Endoscopic mucosal ablation therapy*
- This therapy is typically reserved for patients with **high-grade dysplasia** or **intramucosal carcinoma** in Barrett's esophagus, after diagnosis has been confirmed by biopsy.
- It would be premature to consider ablation without a definitive histological diagnosis of dysplasia.
*Esophagectomy*
- **Esophagectomy** is a major surgical procedure reserved for advanced esophageal cancer or high-grade dysplasia refractory to endoscopic therapies.
- It is an overly aggressive and inappropriate initial step without histological confirmation and assessment of dysplasia or cancer.
*High-dose pantoprazole*
- While proton pump inhibitors (PPIs) like pantoprazole are used to manage GERD symptoms and may help prevent progression of Barrett's esophagus, this patient is already on omeprazole daily.
- Simply increasing the dose of PPI does not address the need for **histological evaluation** of the abnormal-appearing mucosa for dysplasia or cancer.
*Laparoscopic Nissen fundoplication*
- This surgical procedure aims to strengthen the lower esophageal sphincter to treat severe GERD when medical management fails.
- While it addresses reflux, it does not directly evaluate or treat the potential **precancerous changes** in the esophageal lining seen on endoscopy, making biopsies a more immediate and critical next step.
Respiratory system histology US Medical PG Question 8: A 35-year-old woman presents to a pre-operative evaluation clinic prior to an elective cholecystectomy. She has a 5 pack-year smoking history. The anesthesiologist highly recommends to discontinue smoking for at least 8 weeks prior to the procedure for which she is compliant. What is the most likely histology of her upper respiratory tract's epithelial lining at the time of her surgery?
- A. Simple squamous
- B. Simple columnar
- C. Pseudostratified columnar (Correct Answer)
- D. Stratified squamous
- E. Stratified columnar
Respiratory system histology Explanation: ***Pseudostratified columnar***
- The upper respiratory tract is normally lined by **pseudostratified ciliated columnar epithelium** with goblet cells, which is crucial for mucociliary clearance.
- While smoking can initially cause **squamous metaplasia**, discontinuing smoking for 8 weeks allows for significant, if not complete, **reversal of these changes** back to the normal pseudostratified columnar epithelium.
*Simple squamous*
- This type of epithelium is found in areas designed for efficient **gas exchange** (e.g., alveoli of the lungs) and is not typical for the conductive airways of the upper respiratory tract.
- It lacks the **cilia and goblet cells** necessary for clearing inhaled particles and pathogens.
*Simple columnar*
- **Simple columnar epithelium** is found in regions like the lining of the gastrointestinal tract (e.g., stomach, small and large intestines) and is not characteristic of the upper respiratory tract.
- While it can have goblet cells, it typically lacks **cilia** for respiratory clearance.
*Stratified squamous*
- **Stratified squamous epithelium** is found in areas subject to friction and abrasion, such as the oral cavity, pharynx, and esophagus.
- While chronic smoking can induce **squamous metaplasia** in the respiratory tract, an 8-week cessation period would likely result in the reversal of this change back to the normal type.
*Stratified columnar*
- **Stratified columnar epithelium** is a relatively rare type found in specific locations like parts of the male urethra and some large excretory ducts.
- It is not the normal or even a common metaplastic lining for the human upper respiratory tract.
Respiratory system histology US Medical PG Question 9: A 26-year-old woman comes to the physician because she has not had a menstrual period for 5 weeks. Menarche was at the age of 14 years and menses occurred at regular 30-day intervals. She reports having unprotected sexual intercourse 3 weeks ago. A urine pregnancy test is positive. Which of the following best describes the stage of development of the embryo at this time?
- A. Fetal heart is beating, but cardiac activity is not yet visible on ultrasound
- B. Limb buds have formed, but fetal movements have not begun
- C. Sexual differentiation has begun, but fetal movement has not started
- D. Neural crest has formed, but limb buds have not yet formed (Correct Answer)
- E. Implantation has occurred, but notochord has not yet formed
Respiratory system histology Explanation: ***Neural crest has formed, but limb buds have not yet formed***
- At **5 weeks gestational age (3 weeks post-fertilization)**, neurulation is completing or recently completed
- **Neural crest cells** migrate from the neural folds during weeks 3-4 post-fertilization and are definitely present by this time
- **Limb buds** appear later, around week 4-5 post-fertilization (week 6-7 gestational age), making this the most accurate description for the current developmental stage
*Fetal heart is beating, but cardiac activity is not yet visible on ultrasound*
- The primitive heart tube begins contracting around day 22-23 post-fertilization (early week 4)
- At 3 weeks post-fertilization (5 weeks gestational age), the heart may just be starting to beat, but this timing is less precise
- Cardiac activity becomes visible on transvaginal ultrasound around 5.5-6 weeks gestational age, so this option is close but less precise than the correct answer
*Limb buds have formed, but fetal movements have not begun*
- **Limb buds** typically appear around week 4-5 post-fertilization (week 6-7 gestational age)
- This is **too advanced** for 3 weeks post-fertilization
- While fetal movements aren't perceptible to the mother until 16-20 weeks, they begin much later than the current stage
*Sexual differentiation has begun, but fetal movement has not started*
- **Sexual differentiation** of the gonads begins around week 7 post-fertilization (week 9 gestational age)
- External genitalia differentiation occurs even later (weeks 9-12 post-fertilization)
- This stage is **far too advanced** for the current 3-week post-fertilization timeframe
*Implantation has occurred, but notochord has not yet formed*
- **Implantation** occurs 6-12 days after fertilization, which is approximately 2-3 weeks before a positive pregnancy test
- The **notochord** forms during gastrulation in the **3rd week post-fertilization** (5th week gestational age)
- By the time of this positive pregnancy test (5 weeks gestational age), the notochord has **already formed**, making this statement incorrect
Respiratory system histology US Medical PG Question 10: A 4-week-old boy is brought to the emergency department with a 2-day history of projectile vomiting after feeding. His parents state that he is their firstborn child and that he was born healthy. He developed normally for several weeks but started to eat less 1 week ago. Physical exam reveals a small, round mass in the right upper quadrant of the abdomen close to the midline. The infant throws up in the emergency department, and the vomitus is observed to be watery with no traces of bile. Which of the following is associated with the most likely cause of this patient's symptoms?
- A. Chloride transport defect
- B. Recanalization defect
- C. Vascular accident
- D. Failure of neural crest migration
- E. Nitric oxide synthase deficiency (Correct Answer)
Respiratory system histology Explanation: ***Nitric oxide synthase deficiency***
- This symptom constellation points to **pyloric stenosis**, which is characterized by smooth muscle hypertrophy and concurrent deficiency of **nitric oxide synthase** and possibly **interstitial cells of Cajal** in the pylorus.
- The thickened pylorus creates an obstruction, leading to non-bilious projectile vomiting, an "olive-like" mass, and subsequent electrolyte imbalances.
*Chloride transport defect*
- A chloride transport defect, particularly in the **CFTR (cystic fibrosis transmembrane conductance regulator) gene**, is characteristic of cystic fibrosis.
- While cystic fibrosis can cause gastrointestinal symptoms like **meconium ileus** or malabsorption, it does not typically present with projectile vomiting and a palpable abdominal mass in this age group, nor is it the primary cause of pyloric stenosis.
*Recanalization defect*
- **Recanalization defects** refer to issues in the development of a lumen in structures that are initially solid during embryogenesis, such as the gut tube.
- This can lead to conditions like **duodenal atresia**, which typically presents with **bilious vomiting** (due to obstruction distal to the ampulla of Vater) and often a "double-bubble" sign on imaging, which is not described here.
*Vascular accident*
- A **vascular accident** in the gut can lead to conditions such as **necrotizing enterocolitis** in neonates or **bowel ischemia/infarction**.
- These conditions would typically present with symptoms like bloody stools, abdominal distension, lethargy, and systemic signs of illness, rather than isolated projectile vomiting and an abdominal mass.
*Failure of neural crest migration*
- **Failure of neural crest cell migration** is the underlying cause of **Hirschsprung disease**, where there is an absence of ganglion cells in the distal colon.
- This typically presents with **constipation**, abdominal distension, and failure to pass meconium, rather than projectile vomiting, and usually affects the large intestine.
More Respiratory system histology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.