GI tract histology US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for GI tract histology. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
GI tract histology US Medical PG Question 1: A 38-year-old man comes to the clinic complaining of recurrent abdominal pain for the past 2 months. He reports a gnawing, dull pain at the epigastric region that improves with oral ingestion. He has been taking calcium carbonate for the past few weeks; he claims that “it used to help a lot but it’s losing its effects now.” Laboratory testing demonstrated increased gastrin levels after the administration of secretin. A push endoscopy visualized several ulcers at the duodenum and proximal jejunum. What characteristics distinguish the jejunum from the duodenum?
- A. Lack of goblet cells
- B. Crypts of Lieberkuhn
- C. Lack of submucosal Brunner glands (Correct Answer)
- D. Peyer patches
- E. Plicae circulares
GI tract histology Explanation: ***Lack of submucosal Brunner glands***
- The **jejunum** lacks **Brunner glands**, which are characteristic of the **duodenum** and secrete alkaline mucus to neutralize acidic chyme from the stomach.
- The absence of these glands helps differentiate the jejunum from the duodenum histologically.
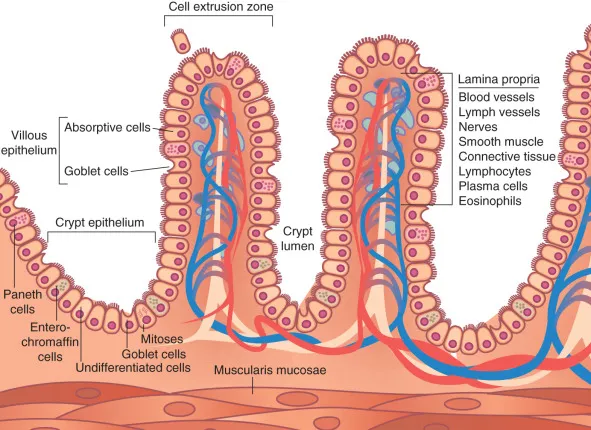
*Lack of goblet cells*
- **Goblet cells** are present throughout the small intestine, including both the duodenum and jejunum, though their density increases distally.
- Therefore, the **lack of goblet cells** does not distinguish the jejunum from the duodenum.
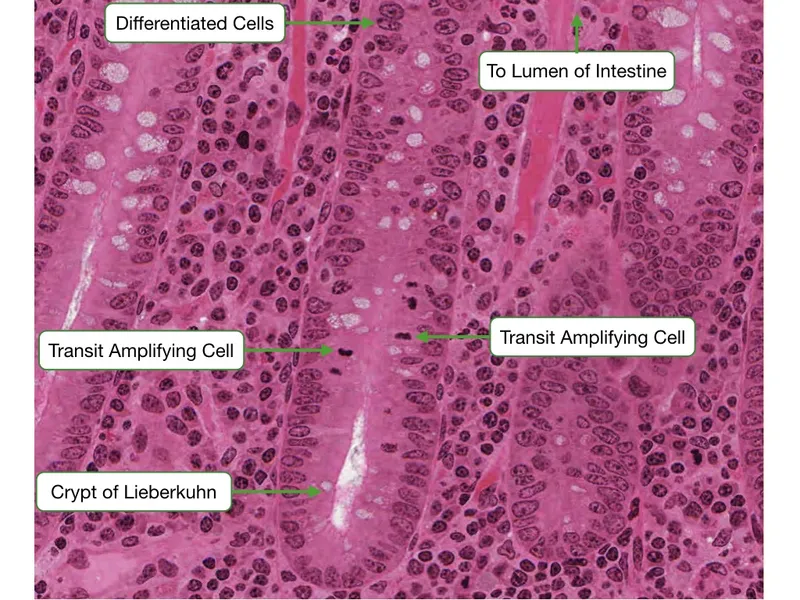
*Crypts of Lieberkuhn*
- **Crypts of Lieberkuhn** (intestinal crypts) are present throughout the entire small intestine, including both the **duodenum** and **jejunum**, where they house stem cells for epithelial renewal.
- Their presence is not a distinguishing feature between these two segments histologically.
*Peyer patches*
- **Peyer patches** are lymphoid aggregates primarily found in the **ileum**, not the jejunum or duodenum, and are involved in immune surveillance.
- They are a distinguishing feature of the ileum but not between the jejunum and duodenum.
*Plicae circulares*
- **Plicae circulares** (also known as valves of Kerckring or circular folds) are macroscopic folds of the mucosa and submucosa that are present in both the **duodenum** and **jejunum**.
- They are most prominent in the jejunum, but their mere presence does not distinguish the jejunum from the duodenum.
GI tract histology US Medical PG Question 2: Which of the following cells in the body depends on dynein for its unique functioning?
- A. Small intestinal mucosal cell
- B. Skeletal muscle cell
- C. Adipocyte
- D. Lower esophageal mucosal cell
- E. Fallopian tube mucosal cell (Correct Answer)
GI tract histology Explanation: ***Fallopian tube mucosal cell***
- Dynein is a **motor protein** that facilitates the movement of **cilia** along microtubules.
- The ciliary action in fallopian tube mucosal cells is crucial for **transporting the ovum** from the ovary to the uterus.
*Small intestinal mucosal cell*
- These cells primarily depend on **microvilli** for absorption, which are actin-based structures and do not directly involve dynein for their primary function of absorption.
- While they have some cilia, their unique and defining function is nutrient absorption, not movement dependent on dynein.
*Skeletal muscle cell*
- Skeletal muscle cells rely on the interaction of **actin and myosin** filaments for **contraction**.
- Dynein is not directly involved in the mechanism of muscle contraction.
*Adipocyte*
- Adipocytes are specialized in **lipid storage** and release, a process that does not involve dynein.
- Their unique function does not depend on intracellular or extracellular movement facilitated by dynein.
*Lower esophageal mucosal cell*
- These cells primarily provide a **protective barrier** against gastric acid reflux.
- Their function involves **stratified squamous epithelium** and mucus production, not ciliary movement dependent on dynein.
GI tract histology US Medical PG Question 3: A 40-year-old female comes in with several months of unintentional weight loss, epigastric pain, and a sensation of abdominal pressure. She has diabetes well-controlled on metformin but no other prior medical history. She has not previously had any surgeries. On physical exam, her doctor notices brown velvety areas of pigmentation on her neck. Her doctor also notices an enlarged, left supraclavicular node. Endoscopic findings show a stomach wall that appears to be grossly thickened. Which of the following findings would most likely be seen on biopsy?
- A. Keratin pearls
- B. Noncaseating granulomas
- C. Peyer's patches
- D. Psammoma bodies
- E. Cells with central mucin pool (Correct Answer)
GI tract histology Explanation: ***Cells with central mucin pool***
- The patient's symptoms (unintentional weight loss, epigastric pain, abdominal pressure, **acanthosis nigricans**, and a **Virchow node**) are highly suggestive of **gastric adenocarcinoma**, particularly the **diffuse type**.
- **Signet ring cells**, characterized by a **large central mucin vacuole** that displaces the nucleus to the periphery, are pathognomonic for **diffuse gastric adenocarcinoma**.
*Keratin pearls*
- **Keratin pearls** are a hallmark feature of **squamous cell carcinoma**, which is a type of cancer arising from squamous epithelial cells.
- While squamous cell carcinoma can occur in the esophagus, it is an extremely rare finding in the stomach, which is lined by glandular epithelium.
*Noncaseating granulomas*
- **Noncaseating granulomas** are characteristic of conditions like **Crohn's disease** or **sarcoidosis**.
- These conditions do not typically present with the described aggressive features of gastric malignancy or the presence of acanthosis nigricans and a Virchow node.
*Peyer's patches*
- **Peyer's patches** are normal lymphoid structures found in the **ileum** of the small intestine, playing a role in immune surveillance.
- Their presence in a biopsy would indicate normal small intestinal tissue, not a malignant gastric lesion.
*Psammoma bodies*
- **Psammoma bodies** are concentric, laminated calcified structures typically seen in certain types of **cancers with serous or papillary differentiation**, such as **papillary thyroid carcinoma**, **meningioma**, and **serous ovarian carcinoma**.
- They are not a characteristic finding in gastric adenocarcinoma.
GI tract histology US Medical PG Question 4: A 34-year-old man presents with a 2-day history of loose stools, anorexia, malaise, and abdominal pain. He describes the pain as moderate, cramping in character, and diffusely localized to the periumbilical region. His past medical history is unremarkable. He works as a wildlife photographer and, 1 week ago, he was in the Yucatan peninsula capturing the flora and fauna for a magazine. The vital signs include blood pressure 120/60 mm Hg, heart rate 90/min, respiratory rate 18/min, and body temperature 38.0°C (100.4°F). Physical examination is unremarkable. Which of the following is a characteristic of the microorganism most likely responsible for this patient’s symptoms?
- A. Disabling Gi alpha subunit
- B. Production of lecithinase
- C. Overactivation of guanylate cyclase (Correct Answer)
- D. Inactivation of the 60S ribosomal subunit
- E. Presynaptic vesicle dysregulation
GI tract histology Explanation: ***Overactivation of guanylate cyclase***
- The patient's symptoms (loose stools, abdominal cramping, recent travel to the Yucatan Peninsula) are highly suggestive of **traveler's diarrhea**, most commonly caused by **enterotoxigenic E. coli (ETEC)**.
- ETEC produces a **heat-stable toxin (ST)** that binds to the **guanylate cyclase C receptor** on intestinal epithelial cells, leading to **increased intracellular cGMP** and subsequent **chloride and water secretion**.
*Disabling Gi alpha subunit*
- This mechanism is characteristic of **pertussis toxin** (from *Bordetella pertussis*), which **ADP-ribosylates and inactivates the Gi protein**, preventing inhibition of adenylate cyclase.
- Pertussis toxin is associated with **whooping cough**, not gastrointestinal disease or traveler's diarrhea.
- Note: **Cholera toxin** works via a different mechanism—it **activates Gs alpha subunit** to increase cAMP, causing severe watery diarrhea, but the clinical presentation here (mild symptoms, travel to endemic area) favors ETEC over cholera.
*Production of lecithinase*
- **Lecithinase (alpha-toxin)** is a characteristic virulence factor of **Clostridium perfringens**, causing gas gangrene and some food poisoning, not the watery diarrhea described here.
- It acts as a phospholipase, disrupting cell membranes.
*Inactivation of the 60S ribosomal subunit*
- This mechanism is associated with **Shiga toxin** produced by **enterohemorrhagic E. coli (EHEC)** and **Shigella dysenteriae**.
- These typically cause **bloody diarrhea** and **hemolytic uremic syndrome (HUS)**, which are not described in this patient.
*Presynaptic vesicle dysregulation*
- This mechanism is characteristic of **botulinum toxin** (from *Clostridium botulinum*), which **cleaves SNARE proteins** and prevents acetylcholine release, causing flaccid paralysis.
- It is not involved in bacterial gastroenteritis causing diarrhea.
GI tract histology US Medical PG Question 5: A 48-year-old female visits your office complaining that she has trouble swallowing solids and liquids, has persistent bad breath, and sometimes wakes up with food on her pillow. Manometry studies show an absence of functional peristalsis and a failure of the lower esophageal sphincter to relax upon swallowing. The patient's disorder is associated with damage to which of the following?
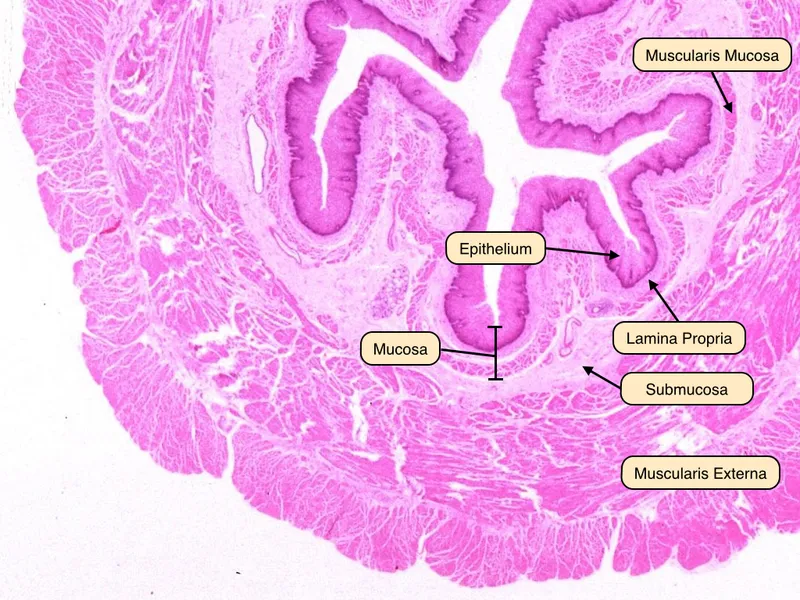
- A. Submucosal (Meissner’s) plexus
- B. Muscularis mucosa
- C. Myenteric (Auerbach’s) plexus (Correct Answer)
- D. Lamina propria
- E. Submucosa
GI tract histology Explanation: ***Myenteric (Auerbach’s) plexus***
- The clinical presentation, including **dysphagia for solids and liquids**, **regurgitation**, bad breath, and findings from manometry (absence of functional peristalsis, failure of LES relaxation), is classic for **achalasia**.
- Achalasia is characterized by the degeneration of ganglion cells in the **myenteric (Auerbach's) plexus** of the esophageal wall, leading to impaired esophageal motility and LES dysfunction.
*Submucosal (Meissner’s) plexus*
- The submucosal plexus is primarily involved in regulating **secretions and local blood flow** within the gastrointestinal tract.
- While important for GI function, damage to this plexus is not the primary cause of the severe motility disorders seen in achalasia.
*Muscularis mucosa*
- The muscularis mucosa is a thin layer of smooth muscle within the mucosa that causes **local movements of the mucosal folds**.
- It does not control the major peristaltic contractions of the esophagus or the relaxation of the lower esophageal sphincter.
*Lamina propria*
- The lamina propria is a layer of connective tissue within the mucosa, rich in **lymphoid tissue, blood vessels, and nerves**, providing structural support and immune function.
- It does not play a direct role in regulating esophageal peristalsis or LES function.
*Submucosa*
- The submucosa is a layer of connective tissue that contains the **submucosal plexus, blood vessels, and lymphatic vessels**.
- While it houses the submucosal plexus, the primary pathology in achalasia involves the myenteric plexus, which controls the muscularis propria responsible for peristalsis.
GI tract histology US Medical PG Question 6: A 52-year-old woman presents with mild epigastric pain and persistent heartburn for the past 2 months. An endoscopy is performed and reveals inflammation of the stomach mucosa without evidence of ulceration. A biopsy is performed and reveals intestinal metaplasia with destruction of a large number of parietal cells. She is diagnosed with chronic atrophic gastritis. Which of the following is characteristic of this patient’s diagnosis?
- A. Serum gastrin levels are decreased.
- B. Caused by a gram-negative rod that is urease positive
- C. It is the most common cause of folate deficiency in the US.
- D. Destruction of the mucosa of the stomach is mediated by T cells. (Correct Answer)
- E. MALT lymphoma is a common complication.
GI tract histology Explanation: ***Destruction of the mucosa of the stomach is mediated by T cells.***
- The type of chronic atrophic gastritis described, characterized by **parietal cell destruction** and **intestinal metaplasia**, is consistent with **autoimmune gastritis** (Type A gastritis).
- Autoimmune gastritis is mediated by **T cells** attacking gastric parietal cells, leading to their destruction and subsequent **achlorhydria** and loss of intrinsic factor.
*Serum gastrin levels are decreased.*
- Destruction of **parietal cells** leads to **achlorhydria** (lack of gastric acid), which removes the negative feedback on **G cells**.
- This results in **compensatory hypergastrinemia**, meaning serum gastrin levels are typically *elevated*, not decreased.
*Caused by a gram-negative rod that is urease positive*
- This describes **Helicobacter pylori infection**, which is the cause of **Type B gastritis** (environmental chronic atrophic gastritis) and typically affects the antrum.
- The patient's presentation with **destruction of parietal cells** and **intestinal metaplasia** is more consistent with **autoimmune (Type A) gastritis**, which is not caused by H. pylori.
*It is the most common cause of folate deficiency in the US.*
- **Folate deficiency** is more commonly associated with **poor dietary intake**, **alcoholism**, malabsorption disorders (e.g., celiac disease), and certain medications.
- While chronic atrophic gastritis can lead to **vitamin B12 deficiency** due to loss of intrinsic factor, it is not the most common cause of folate deficiency.
*MALT lymphoma is a common complication.*
- **MALT (mucosa-associated lymphoid tissue) lymphoma** is a known complication of chronic **H. pylori infection**, especially when it leads to gastritis and lymphoid follicle formation.
- While chronic inflammation is a risk factor for malignancy, MALT lymphoma is less commonly associated with **autoimmune gastritis** compared to H. pylori-induced gastritis.
GI tract histology US Medical PG Question 7: A 56-year-old man comes to the physician because of intermittent retrosternal chest pain. Physical examination shows no abnormalities. Endoscopy shows salmon pink mucosa extending 5 cm proximal to the gastroesophageal junction. Biopsy specimens from the distal esophagus show nonciliated columnar epithelium with numerous goblet cells. Which of the following is the most likely cause of this patient's condition?
- A. Hypermotile esophageal contractions
- B. Atopic inflammation of the esophagus
- C. Fungal infection of the lower esophagus
- D. Esophageal exposure to gastric acid (Correct Answer)
- E. Neoplastic proliferation of esophageal epithelium
GI tract histology Explanation: ***Esophageal exposure to gastric acid***
- The presence of **salmon pink mucosa** extending 5 cm proximally from the gastroesophageal junction, along with **nonciliated columnar epithelium** and **goblet cells** in biopsy specimens, is characteristic of **Barrett's esophagus**.
- Barrett's esophagus is a metaplastic change in the esophageal lining, typically caused by chronic **gastroesophageal reflux disease (GERD)**, where recurrent exposure to **gastric acid** leads to the replacement of normal stratified squamous epithelium with intestinal-type columnar epithelium.
*Hypermotile esophageal contractions*
- **Hypermotile esophageal contractions**, such as in spastic disorders, can cause chest pain but do not typically lead to the **mucosal changes** of Barrett's esophagus.
- While they can contribute to reflux, they are not the direct cause of the intestinal metaplasia seen in this patient.
*Atopic inflammation of the esophagus*
- **Atopic inflammation of the esophagus** refers to **eosinophilic esophagitis**, characterized by dysphagia and food impaction, and histologically by significant eosinophil infiltration.
- This condition does not typically present with the **salmon pink mucosa** or **goblet cells** that are indicative of Barrett's esophagus.
*Fungal infection of the lower esophagus*
- **Fungal infections**, such as **Candida esophagitis**, usually present with **odynophagia** and endoscopy showing **white plaques**, not salmon pink mucosa or columnar metaplasia.
- Biopsy would reveal fungal elements, not goblet cells or columnar epithelium.
*Neoplastic proliferation of esophageal epithelium*
- **Neoplastic proliferation** would involve dysplastic changes or carcinoma, which would show severe architectural distortion and cytologic atypia, distinct from the **metaplastic changes** (nonciliated columnar epithelium with goblet cells) observed here.
- While Barrett's esophagus is a **precursor to adenocarcinoma**, the biopsy description indicates metaplasia, not active neoplasia.
GI tract histology US Medical PG Question 8: A 45-year-old woman comes to the physician because of progressive difficulty swallowing solids and liquids over the past 4 months. She has lost 4 kg (9 lb) during this period. There is no history of serious illness. She emigrated to the US from Panama 7 years ago. She does not smoke cigarettes or drink alcohol. Cardiopulmonary examination shows a systolic murmur and an S3 gallop. A barium radiograph of the chest is shown. Histopathologic examination of the esophageal wall is most likely to show which of the following?
- A. Presence of intranuclear basophilic inclusions
- B. Atrophy of esophageal smooth muscle cells
- C. Infiltration of eosinophils in the epithelium
- D. Presence of metaplastic columnar epithelium
- E. Absence of myenteric plexus neurons (Correct Answer)
GI tract histology Explanation: ***Absence of myenteric plexus neurons***
- This finding is pathognomonic for **Chagas disease** (American trypanosomiasis), caused by *Trypanosoma cruzi*, endemic to Central and South America including Panama.
- The parasite destroys the **myenteric (Auerbach's) plexus neurons** in the esophageal wall, disrupting normal peristalsis and leading to **megaesophagus**.
- This results in **progressive dysphagia for both solids and liquids** and weight loss, as seen in this patient.
- The **cardiac findings** (systolic murmur and S3 gallop) indicate associated **chagasic cardiomyopathy**, another manifestation of chronic Chagas disease.
*Presence of intranuclear basophilic inclusions*
- Suggestive of **cytomegalovirus (CMV) esophagitis**, typically seen in immunocompromised patients (HIV/AIDS, transplant recipients).
- This patient has no immunocompromised state, and CMV does not cause the cardiac manifestations or chronic megaesophagus seen here.
*Atrophy of esophageal smooth muscle cells*
- Not characteristic of Chagas disease or achalasia; these conditions typically show **smooth muscle hypertrophy** due to chronic obstruction.
- Muscle atrophy would not explain the dysphagia, megaesophagus, or cardiac findings.
*Infiltration of eosinophils in the epithelium*
- Indicates **eosinophilic esophagitis**, an allergic condition usually presenting with food impaction and dysphagia mainly for solids.
- Would not explain the cardiac manifestations or the epidemiological connection to Panama.
*Presence of metaplastic columnar epithelium*
- Represents **Barrett's esophagus**, a complication of chronic gastroesophageal reflux disease (GERD).
- The patient's presentation with dysphagia for both solids and liquids, cardiac disease, and megaesophagus on barium study points to a **motility disorder** (Chagas disease), not reflux disease.
GI tract histology US Medical PG Question 9: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
GI tract histology Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
GI tract histology US Medical PG Question 10: A 72-year-old male with a past medical history significant for aortic stenosis and hypertension presents to the emergency department complaining of weakness for the past 3 weeks. He states that, apart from feeling weaker, he also has noted lightheadedness, pallor, and blood-streaked stools. The patient's vital signs are stable, and he is in no acute distress. Laboratory workup reveals that the patient is anemic. Fecal occult blood test is positive for bleeding. EGD was performed and did not reveal upper GI bleeding. Suspecting a lower GI bleed, a colonoscopy is performed after prepping the patient, and it is unremarkable. What would be an appropriate next step for localizing a lower GI bleed in this patient?
- A. Technetium-99 labelled erythrocyte scintigraphy (Correct Answer)
- B. Flexible sigmoidoscopy
- C. Nasogastric tube lavage
- D. Ultrasound of the abdomen
- E. CT of the abdomen
GI tract histology Explanation: ***Technetium-99 labelled erythrocyte scintigraphy***
- This test can detect **slow-rate lower GI bleeds** (as low as 0.2-0.5 mL/min) that may be missed by endoscopy or colonoscopy, especially when the bleeding is intermittent or subtle.
- Given the **negative EGD** and **unremarkable colonoscopy** despite evidence of an ongoing lower GI bleed, this nuclear medicine study is appropriate for localization.
- Particularly useful in this patient with **aortic stenosis**, where angiodysplasia (vascular malformations, often in the small bowel) is a common cause of obscure GI bleeding (Heyde's syndrome).
*Flexible sigmoidoscopy*
- This procedure only visualizes the **rectum and a portion of the sigmoid colon**, which is insufficient given the negative full colonoscopy.
- It would not provide any new information for localizing a bleed that has already been ruled out from the accessible colon.
*Nasogastric tube lavage*
- This procedure is used to assess for **upper GI bleeding** by checking for blood in the gastric contents.
- The EGD already ruled out an upper GI bleed, making this step unnecessary and unhelpful for a suspected lower GI source.
*Ultrasound of the abdomen*
- Abdominal ultrasound is primarily used to evaluate **solid organs** (e.g., liver, gallbladder, kidneys) and potential fluid collections.
- It is generally **not effective** for localizing or diagnosing the source of active GI bleeding.
*CT of the abdomen*
- A standard CT abdomen without specialized imaging protocol has **limited sensitivity** for detecting the source of GI bleeding.
- While **CT angiography** (a different test with IV contrast timed to arterial phase) can detect active bleeding at rates >0.3-0.5 mL/min, a routine "CT of the abdomen" as listed in this option would not be adequate for localizing occult GI bleeding.
More GI tract histology US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.