Thalamus and hypothalamus US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Thalamus and hypothalamus. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Thalamus and hypothalamus US Medical PG Question 1: A 58-year-old woman presents to the clinic with an abnormal sensation on the left side of her body that has been present for the past several months. At first, the area seemed numb and she recalls touching a hot stove and accidentally burning herself but not feeling the heat. Now she is suffering from a constant, uncomfortable burning pain on her left side for the past week. The pain gets worse when someone even lightly touches that side. She has recently immigrated and her past medical records are unavailable. Last month she had a stroke but she cannot recall any details from the event. She confirms a history of hypertension, type II diabetes mellitus, and bilateral knee pain. She also had cardiac surgery 20 years ago. She denies fever, mood changes, weight changes, and trauma to the head, neck, or limbs. Her blood pressure is 162/90 mm Hg, the heart rate is 82/min, and the respiratory rate is 15/min. Multiple old burn marks are visible on the left hand and forearm. Muscle strength is mildly reduced in the left upper and lower limbs. Hyperesthesia is noted in the left upper and lower limbs. Laboratory results are significant for:
Hemoglobin 13.9 g/dL
MCV 92 fL
White blood cells 7,500/mm3
Platelets 278,000/mm3
Creatinine 1.3 U/L
BUN 38 mg/dL
TSH 2.5 uU/L
Hemoglobin A1c 7.9%
Vitamin B12 526 ng/L
What is the most likely diagnosis?
- A. Conversion disorder
- B. Complex regional pain syndrome
- C. Dejerine-Roussy syndrome (Correct Answer)
- D. Medial medullary syndrome
- E. Subacute combined degeneration of spinal cord
Thalamus and hypothalamus Explanation: ***Dejerine-Roussy syndrome***
- The patient's symptoms of **contralateral hemianesthesia**, followed by **dysesthesia**, **spontaneous burning pain**, and **allodynia/hyperalgesia**, developing after a stroke a month prior, are classic for **Dejerine-Roussy syndrome** (thalamic pain syndrome). The history of unnoticed burns and hyperesthesia supports this.
- This syndrome is caused by a lesion in the **thalamus**, typically due to a stroke, which disrupts sensory pathways and leads to an abnormal processing of sensory information.
*Conversion disorder*
- Conversion disorder involves neurological symptoms that are **incompatible with recognized neurological or medical conditions** and are often associated with psychological stress.
- The patient's symptoms are clearly attributable to a known neurological etiology (a recent stroke) and specific anatomical location (thalamus), ruling out conversion disorder.
*Complex regional pain syndrome*
- **Complex regional pain syndrome (CRPS)** is characterized by severe pain, swelling, and autonomic dysfunction, typically affecting a **single limb distal to an injury**, but not necessarily associated with a stroke to the brain.
- While the patient has burning pain and hyperesthesia, the **hemibody distribution** and clear link to a prior stroke make CRPS less likely than a central lesion.
*Medial medullary syndrome*
- **Medial medullary syndrome** results from damage to the medial medulla and typically presents with **ipsilateral tongue weakness**, **contralateral hemiparesis**, and **contralateral loss of vibratory and proprioceptive sensation**, but not the prominent burning pain and allodynia described.
- The patient's primary sensory complaints of burning pain and hyperesthesia across an entire hemibody are not characteristic of medial medullary syndrome.
*Subacute combined degeneration of spinal cord*
- **Subacute combined degeneration** is caused by **vitamin B12 deficiency** and affects the dorsal and lateral columns of the spinal cord, leading to **paresthesias**, weakness, gait ataxia, and impaired proprioception.
- The patient's **vitamin B12 level is normal**, and the symptoms are acute-onset and unilateral, clearly linked to a stroke, not a progressive, symmetrical myelopathy.
Thalamus and hypothalamus US Medical PG Question 2: An 11-year-old boy presents with a 2-day history of uncontrollable shivering. During admission, the patient’s vital signs are within normal limits, except for a fluctuating body temperature registering as low as 35.0°C (95.0°F) and as high as 40.0°C (104.0°F), requiring alternating use of cooling and warming blankets. A complete blood count (CBC) is normal, and a chest radiograph is negative for consolidations and infiltrates. An MRI of the brain reveals a space-occupying lesion infiltrating the posterior hypothalamus and extending laterally. Which of the following additional findings are most likely, based on this patient’s physical examination?
- A. Polyuria
- B. Hyperphagia
- C. Galactorrhea
- D. Sleep disturbances
- E. Anorexia (Correct Answer)
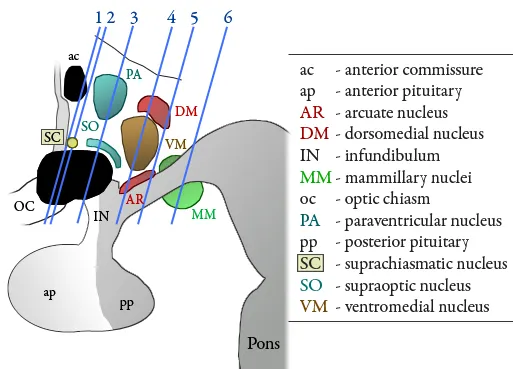
Thalamus and hypothalamus Explanation: **Anorexia**
- **Hypothalamic lesions**, particularly those affecting the **lateral hypothalamus**, often lead to **anorexia** and **weight loss** due to the role of this region in stimulating appetite.
- The patient's presentation with **uncontrollable shivering** and **deregulated body temperature** further points to hypothalamic dysfunction, which can also disrupt feeding centers.
*Polyuria*
- **Polyuria** is typically associated with damage to the **posterior pituitary gland** or its connections to the hypothalamus, leading to **diabetes insipidus** (lack of ADH).
- While a hypothalamic lesion can affect ADH production, the primary symptom constellation in this case more strongly suggests disruption of other hypothalamic functions.
*Hyperphagia*
- **Hyperphagia** (increased appetite) and **obesity** are most commonly linked to damage to the **ventromedial hypothalamus**, which is considered the satiety center.
- The presented lesion is described as infiltrating the posterior hypothalamus and extending laterally, making hyperphagia less likely than anorexia.
*Galactorrhea*
- **Galactorrhea** is often caused by **hyperprolactinemia**, which can result from lesions compressing the **pituitary stalk** or interfering with **dopamine's inhibitory effect** on prolactin release in the anterior pituitary.
- While a large hypothalamic lesion could theoretically impact pituitary function secondarily, galactorrhea is not a direct or most likely consequence of a posterior and lateral hypothalamic lesion.
*Sleep disturbances*
- While the **hypothalamus** plays a critical role in **sleep-wake cycles** (e.g., the **suprachiasmatic nucleus**), **uncontrollable shivering** and **poikilothermia** point more directly to acute disruption of temperature regulation rather than sleep disturbances as the most prominent likely additional finding.
- Many types of brain lesions can cause sleep disturbances, but the specific presentation here suggests a more particular set of hypothalamic dysfunctions.
Thalamus and hypothalamus US Medical PG Question 3: An 18-year-old man presents to his primary care physician with a complaint of excessive daytime sleepiness. He denies any substance abuse or major changes in his sleep schedule. He reports frequently dozing off during his regular daily activities. On further review of systems, he endorses falling asleep frequently with the uncomfortable sensation that there is someone in the room, even though he is alone. He also describes that from time to time, he has transient episodes of slurred speech when experiencing heartfelt laughter. Vital signs are stable, and his physical exam is unremarkable. This patient is likely deficient in a neurotransmitter produced in which part of the brain?
- A. Hippocampus
- B. Midbrain
- C. Pons nucleus
- D. Hypothalamus (Correct Answer)
- E. Thalamus
Thalamus and hypothalamus Explanation: ***Hypothalamus***
- The patient's symptoms of excessive daytime sleepiness, cataplexy (falling asleep with strong emotions like laughter), and hypnagogic hallucinations (sensing someone in the room upon falling asleep) are classic for **narcolepsy**.
- Narcolepsy type 1 is characterized by a significant loss of **orexin (hypocretin)** neurons, a neuropeptide primarily produced in the **lateral hypothalamus** (specifically the lateral and perifornical areas), which plays a crucial role in maintaining wakefulness.
*Hippocampus*
- The **hippocampus** is primarily involved in **memory formation** and spatial navigation.
- Deficiencies in neurotransmitters produced or acting in the hippocampus are typically associated with memory disorders, not narcolepsy.
*Midbrain*
- The **midbrain** contains nuclei involved in dopamine, serotonin, and norepinephrine pathways, which are critical for mood, reward, and sleep-wake regulation.
- While these neurotransmitters influence the sleep-wake cycle, the primary deficiency in narcolepsy type 1 is specifically orexin, which originates from the hypothalamus, not the midbrain.
*Pons nucleus*
- The **pons** is essential for regulating sleep stages, particularly **REM sleep**, and contains nuclei involved in breathing and motor control.
- While it contributes to sleep architecture, the core pathology of narcolepsy type 1, the loss of orexin-producing neurons, is located higher in the brain, in the hypothalamus.
*Thalamus*
- The **thalamus** acts as a crucial relay station for sensory and motor signals to the cerebral cortex and is involved in regulating consciousness and alertness.
- While it is involved in arousal regulation, it is not the primary site of orexin production, nor is a neurotransmitter deficiency directly from the thalamus the primary cause of narcolepsy.
Thalamus and hypothalamus US Medical PG Question 4: A 20-year-old woman reports to student health complaining of 5 days of viral symptoms including sneezing and a runny nose. She started coughing 2 days ago and is seeking cough medication. She additionally mentions that she developed a fever 2 days ago, but this has resolved. On exam, her temperature is 99.0°F (37.2°C), blood pressure is 118/76 mmHg, pulse is 86/min, and respirations are 12/min. Changes in the activity of warm-sensitive neurons in which part of her hypothalamus likely contributed to the development and resolution of her fever?
- A. Anterior hypothalamus (Correct Answer)
- B. Paraventricular nucleus
- C. Suprachiasmatic nucleus
- D. Lateral area
- E. Posterior hypothalamus
Thalamus and hypothalamus Explanation: ***Anterior hypothalamus***
- The **anterior hypothalamus** contains warm-sensitive neurons that detect increases in body temperature and activate mechanisms for heat dissipation, such as sweating and vasodilation.
- In fever, **prostaglandins** increase the set point in the anterior hypothalamus, causing the body to retain heat and increase heat production until the new set point is reached; resolution of fever involves resetting this set point back to normal.
*Paraventricular nucleus*
- The **paraventricular nucleus** is primarily involved in neuroendocrine functions, stress response, and the regulation of appetite and autonomic nervous system.
- It plays a significant role in releasing hormones like **corticotropin-releasing hormone (CRH)** and **oxytocin**, not direct temperature regulation.
*Suprachiasmatic nucleus*
- The **suprachiasmatic nucleus (SCN)** is the body's main biological clock, regulating **circadian rhythms** including the sleep-wake cycle and daily fluctuations in body temperature.
- While it influences the normal diurnal variation in body temperature, it is not directly responsible for the acute regulation of fever.
*Lateral area*
- The **lateral hypothalamus** primarily functions as the "hunger center," stimulating foraging and feeding behavior.
- Damage to this area can lead to **anorexia** and reduced food intake, not impairments in fever response.
*Posterior hypothalamus*
- The **posterior hypothalamus** is primarily involved in heat conservation and production mechanisms, such as shivering and vasoconstriction, in response to cold.
- It contains cold-sensitive neurons and functions to raise body temperature if it falls below the set point, but it is not where the set point itself is regulated in response to pyrogens.
Thalamus and hypothalamus US Medical PG Question 5: An 85-year-old woman otherwise healthy presents with left-sided weakness. Her symptoms started 4 hours ago while she was on the phone with her niece. The patient recalls dropping the phone and not being able to pick it up with her left hand. No significant past medical history. No current medications. Physical examination reveals decreased sensation on the left side, worse in the left face and left upper extremity. There is significant weakness of the left upper extremity and weakness and drooping of the lower half of the left face. Ophthalmic examination reveals conjugate eye deviation to the right. A noncontrast CT of the head is unremarkable. The patient is started on aspirin. A repeat contrast CT of the head a few days later reveals an ischemic stroke involving the lateral convexity of right cerebral hemisphere. Which of the following additional findings would most likely be seen in this patient?
- A. Homonymous hemianopsia (Correct Answer)
- B. Horner's syndrome
- C. Amaurosis fugax
- D. Profound lower limb weakness
- E. Prosopagnosia
Thalamus and hypothalamus Explanation: ***Homonymous hemianopsia***
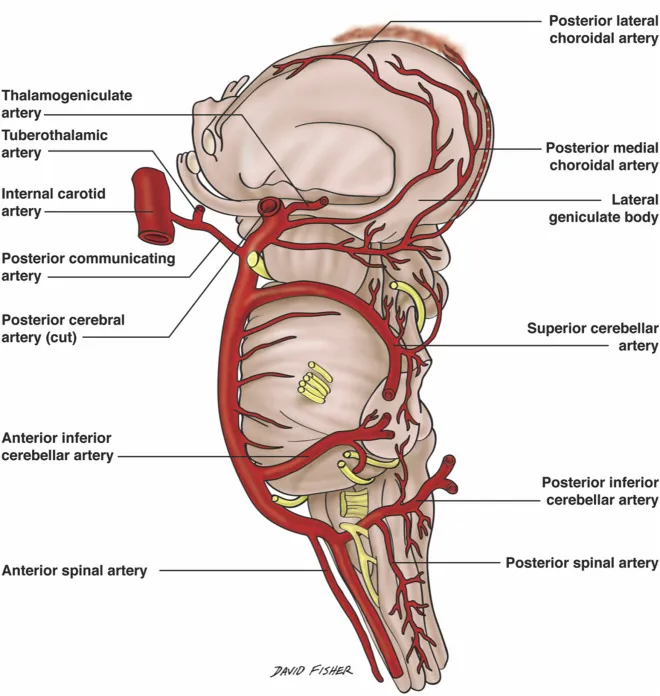
- The patient has an ischemic stroke affecting the **right cerebral hemisphere**, specifically the **lateral convexity**. This suggests involvement of the **middle cerebral artery (MCA)** territory.
- The **optic radiations** carrying visual information from the contralateral visual field pass through the parietal and temporal lobes to the occipital cortex. Damage to these radiations in the right hemisphere would result in a **left homonymous hemianopsia**.
*Horner's syndrome*
- Characterized by **ptosis**, **miosis**, and **anhidrosis** on one side of the face.
- It results from damage to the **sympathetic pathway**, typically in the brainstem, spinal cord above T1, or sympathetic chain, which is not the primary location of this stroke.
*Amaurosis fugax*
- This is a **transient monocular vision loss** ("curtain coming down") due to temporary interruption of blood flow to the retina, usually from an **ipsilateral carotid artery embolus**.
- It is typically a symptom of impending stroke or TIA, not a direct neurological deficit resulting from a cerebral hemisphere stroke.
*Profound lower limb weakness*
- The described stroke involves the **lateral convexity of the right cerebral hemisphere**, fed by the **middle cerebral artery (MCA)**.
- The MCA primarily supplies the upper limb and facial motor/sensory cortices, leading to more pronounced **upper limb and facial weakness** rather than profound lower limb weakness, which is more characteristic of an **anterior cerebral artery (ACA)** stroke.
*Prosopagnosia*
- This is the inability to recognize familiar faces, often due to damage to the **fusiform gyrus** in the temporal and occipital lobes, usually on the **right side**.
- While it can occur with right hemisphere strokes, it is a specific higher-order cognitive deficit and not the *most likely* additional finding in this presentation focused on motor and sensory deficits and conjugate eye deviation.
Thalamus and hypothalamus US Medical PG Question 6: A 80-year-old man is brought to the emergency department with complaints that he "can't control his left leg". His symptoms started a few hours ago. He was outside taking a walk with his wife when suddenly his leg shot out and kicked her. His past medical history is notable for diabetes, hypertension, and a myocardial infarction 5 years ago. He smokes 1-2 cigarettes/day. He does not use alcohol or illicit drugs. On exam, the patient has intermittent wide, flinging movements that affect his proximal left arm and left leg. Which of the following parts of his brain is most likely damaged?
- A. Ventral posterior thalamic nucleus
- B. Left internal capsule
- C. Right subthalamic nucleus (Correct Answer)
- D. Left subthalamic nucleus
- E. Right internal capsule
Thalamus and hypothalamus Explanation: ***Right subthalamic nucleus***
- The patient's symptoms of sudden, uncontrolled, wide-flinging movements, affecting the contralateral (left) side of the body, are characteristic of **hemiballism**.
- **Hemiballism** is almost exclusively caused by a lesion in the **contralateral subthalamic nucleus (STN)**, or its afferent/efferent connections, most commonly due to a **lacunar infarct**.
*Ventral posterior thalamic nucleus*
- Damage to the **ventral posterior thalamic nucleus** primarily causes **sensory deficits**, such as loss of touch, pain, and temperature sensation, on the contralateral side of the body.
- While it can be involved in motor control, it does not typically cause the characteristic flinging movements seen in hemiballism.
*Left internal capsule*
- A lesion in the **left internal capsule** would result in contralateral (right-sided) motor and sensory deficits, including **hemiparesis** or **hemiplegia**, but not the ballistic, uncontrollable movements described.
- The internal capsule carries major motor and sensory pathways to and from the cerebral cortex.
*Left subthalamic nucleus*
- Damage to the **left subthalamic nucleus** would cause hemiballism on the **contralateral (right) side** of the body.
- The patient's symptoms are on the left side, indicating a lesion in the right subthalamic nucleus.
*Right internal capsule*
- A lesion in the **right internal capsule** would primarily cause contralateral (left-sided) motor and sensory deficits, such as **hemiparesis** or **hemiplegia**.
- While it affects the contralateral side as described in the patient, it would typically present as weakness rather than uncontrolled flinging movements.
Thalamus and hypothalamus US Medical PG Question 7: A 61-year-old man is brought to the emergency department because of increasing weakness of his right arm and leg that began when he woke up that morning. He did not notice any weakness when he went to bed the night before. He has hypertension and hypercholesterolemia. Current medications include hydrochlorothiazide and atorvastatin. He is alert and oriented to person, time, place. His temperature is 36.7°C (98°F), pulse is 91/min, and blood pressure is 132/84 mm Hg. Examination shows drooping of the right side of the face. Muscle strength is decreased in the right upper and lower extremities. Deep tendon reflexes are 4+ on the right side. Sensation is intact. His speech is normal in rate and rhythm. The remainder of the examination shows no abnormalities. An infarction of which of the following sites is the most likely cause of this patient's symptoms?
- A. Base of the left pons
- B. Left cerebellar vermis
- C. Left posterolateral thalamus
- D. Posterior limb of the left internal capsule (Correct Answer)
- E. Left lateral medulla
Thalamus and hypothalamus Explanation: ***Posterior limb of the left internal capsule***
- The patient presents with sudden onset of **right-sided weakness**, including the face, arm, and leg (hemiparesis), consistent with a **pure motor stroke**.
- The **posterior limb of the internal capsule** contains UMN fibers of the **corticospinal and corticobulbar tracts**, which project to the contralateral side of the body, thus lesions here cause contralateral pure motor deficits.
*Base of the left pons*
- A lesion here would typically cause **contralateral hemiparesis or hemiplegia** (right side in this case).
- However, pontine lesions also often include **cranial nerve palsies** (e.g., abducens or facial nerve) or **ataxia**, which are not described.
*Left cerebellar vermis*
- Damage to the cerebellar vermis primarily results in **truncal ataxia** and disorders of gait and balance.
- It would not cause contralateral hemiparesis or facial droop, as seen in this patient.
*Left posterolateral thalamus*
- An infarct in this area would primarily cause **contralateral sensory deficits**, such as hemianesthesia or dysesthesia.
- While motor deficits can occur, they are typically less prominent than sensory issues and would not be the isolated pure motor syndrome described.
*Left lateral medulla*
- A lesion in the lateral medulla (e.g., Wallenberg syndrome) typically presents with **contralateral pain and temperature loss**, ipsilateral Horner's syndrome, ataxia, and dysphagia.
- It would not manifest as an isolated pure motor hemiparesis.
Thalamus and hypothalamus US Medical PG Question 8: Where does the only cranial nerve without a thalamic relay nucleus enter the skull?
- A. Superior orbital fissure
- B. Internal auditory meatus
- C. Foramen rotundum
- D. Jugular foramen
- E. Cribriform plate (Correct Answer)
Thalamus and hypothalamus Explanation: ***Cribriform plate***
- The **olfactory nerve (CN I)** is the only cranial nerve that does not have a thalamic relay nucleus before reaching the cerebral cortex.
- It passes through the **cribriform plate** of the ethmoid bone to reach the olfactory bulbs.
*Superior orbital fissure*
- This opening transmits the **oculomotor (CN III), trochlear (CN IV), ophthalmic division of trigeminal (CN V1)**, and **abducens (CN VI)** nerves.
- These nerves all have sensory or motor components that relay through the thalamus, directly or indirectly.
*Internal auditory meatus*
- This canal transmits the **facial (CN VII)** and **vestibulocochlear (CN VIII)** nerves.
- The vestibulocochlear nerve's auditory pathway involves a thalamic relay in the **medial geniculate nucleus**.
*Foramen rotundum*
- The **maxillary division of the trigeminal nerve (CN V2)** passes through the foramen rotundum.
- Sensory information carried by CN V2 relays through the **thalamus**.
*Jugular foramen*
- This opening transmits the **glossopharyngeal (CN IX), vagus (CN X)**, and **accessory (CN XI)** nerves.
- Sensory components of these nerves, particularly taste and visceral sensation, involve thalamic nuclei.
Thalamus and hypothalamus US Medical PG Question 9: Arrange in sequence the structures involved in the direct pathway (1=Striatum, 2=GPi, 3=Thalamus, 4=Cortex output, 5=Cortex input):-
- A. 1,3,4,2,5
- B. 5,1,2,3,4 (Correct Answer)
- C. 1,2,3,4,5
- D. 5,4,2,3,1
- E. 5,1,3,2,4
Thalamus and hypothalamus Explanation: ***5,1,2,3,4***
- The direct pathway of the basal ganglia begins with the **cortex** (5) sending excitatory signals to the **striatum** (1).
- The striatum then inhibits the **internal globus pallidus (GPi)** (2), which disinhibits the **thalamus** (3), leading to excitation of the **cortex** (4).
- This is the correct sequence: **Cortex input → Striatum → GPi → Thalamus → Cortex output**.
*1,3,4,2,5*
- This sequence is incorrect as it starts with the striatum instead of cortical input.
- The direct pathway does not begin with striatal activity; the cortex must first activate the striatum.
*1,2,3,4,5*
- This order is incorrect because it implies the pathway starts at the striatum rather than the cortex.
- The cortex should be the starting point (5) and the ending point (4) of the motor loop.
*5,4,2,3,1*
- This sequence is incorrect as it places cortex output (4) before the striatum receives input.
- This reverses the functional flow and does not follow the **disinhibitory mechanism** of the direct pathway.
*5,1,3,2,4*
- This sequence incorrectly places the thalamus (3) before the GPi (2).
- In the direct pathway, the striatum must first inhibit the GPi before the thalamus can be disinhibited.
Thalamus and hypothalamus US Medical PG Question 10: A man appearing to be in his mid-50s is brought in by ambulance after he was seen walking on railroad tracks. On further questioning, the patient does not recall being on railroad tracks and is only able to provide his name. Later on, he states that he is a railroad worker, but this is known to be false. On exam, his temperature is 99.9°F (37.7°C), blood pressure is 128/86 mmHg, pulse is 82/min, and respirations are 14/min. He appears disheveled, and his clothes smell of alcohol. The patient is alert, is only oriented to person, and is found to have abnormal eye movements and imbalanced gait when attempting to walk. Which of the following structures in the brain likely has the greatest reduction in the number of neurons?
- A. Mammillary bodies (Correct Answer)
- B. Cerebellar vermis
- C. Parietal-temporal cortex
- D. Frontal eye fields
- E. Basal ganglia
Thalamus and hypothalamus Explanation: ***Mammillary bodies***
- This patient presents with symptoms highly suggestive of **Wernicke-Korsakoff syndrome**, which includes **ophthalmoplegia** (abnormal eye movements), **ataxia** (imbalanced gait), and **confabulation** (making up stories, like being a railroad worker) with **anterograde amnesia** (not recalling being on railroad tracks).
- Wernicke-Korsakoff syndrome is primarily caused by **thiamine (vitamin B1) deficiency**, commonly seen in **chronic alcoholics**, and results in neuronal loss and necrosis, especially in the **mammillary bodies** and dorsomedial nucleus of the thalamus.
*Cerebellar vermis*
- While **alcoholism** can lead to cerebellar damage, particularly the **vermis**, causing **ataxia**, it does not fully explain the **memory deficits, confabulation, and ophthalmoplegia** seen in Wernicke-Korsakoff syndrome.
- Damage to the cerebellar vermis would primarily result in truncal ataxia and gait instability without the prominent amnesia and confabulation.
*Parietal-temporal cortex*
- Damage to the **parietal-temporal cortex** is associated with various cognitive deficits, including **aphasias** and **agnosias**, depending on the specific areas affected.
- While it can be affected by chronic alcoholism, it is not the primary site of damage in **Wernicke-Korsakoff syndrome** and does not typically present with the classic triad.
*Frontal eye fields*
- The **frontal eye fields** are involved in controlling **voluntary eye movements** and saccades. Damage here can cause specific patterns of gaze palsies.
- However, the abnormal eye movements seen in Wernicke-Korsakoff syndrome (e.g., nystagmus, ophthalmoplegia) are typically due to damage in brainstem nuclei and **mammillary bodies**, not primarily the frontal eye fields.
*Basal ganglia*
- The **basal ganglia** are primarily involved in motor control, learning, and executive functions. Damage to these structures can lead to **movement disorders** like Parkinsonism or Huntington's disease.
- While chronic alcoholism can have diffuse effects on the brain, the basal ganglia are not the primary site of pathology in **Wernicke-Korsakoff syndrome**, and damage here would not explain the memory and confabulation symptoms.
More Thalamus and hypothalamus US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.