Spinal cord organization US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Spinal cord organization. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Spinal cord organization US Medical PG Question 1: A 65-year-old woman comes to the physician for the evaluation of sharp, stabbing pain in the lower back for 3 weeks. The pain radiates to the back of her right leg and is worse at night. She reports decreased sensation around her buttocks and inner thighs. During the last several days, she has had trouble urinating. Three years ago, she was diagnosed with breast cancer and was treated with lumpectomy and radiation. Her only medication is anastrozole. Her temperature is 37°C (98.6°F), pulse is 80/min, respirations are 12/min, and blood pressure is 130/70 mm Hg. Neurologic examination shows 4/5 strength in the left lower extremity and 2/5 strength in her right lower extremity. Knee and ankle reflexes are 1+ on the right. The resting anal sphincter tone is normal but the squeeze tone is reduced. Which of the following is the most likely diagnosis?
- A. Anterior spinal cord syndrome
- B. Cauda equina syndrome (Correct Answer)
- C. Conus medullaris syndrome
- D. Central cord syndrome
- E. Brown-sequard syndrome
Spinal cord organization Explanation: ***Cauda equina syndrome***
- The patient's presentation with **severe low back pain**, **saddle anesthesia** (decreased sensation around buttocks and inner thighs), **bladder dysfunction** (trouble urinating), and **motor weakness** in the lower extremities is highly indicative of cauda equina syndrome. This can be caused by **spinal metastases** from her breast cancer.
- The **reduced squeeze tone** of the anal sphincter, despite normal resting tone, further supports the diagnosis, indicating dysfunction of the sacral nerve roots which are compressed in cauda equina syndrome.
*Anterior spinal cord syndrome*
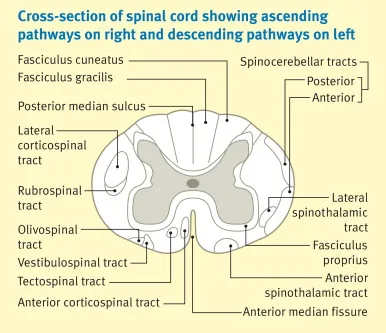
- This syndrome typically presents with **motor paralysis**, loss of **pain** and **temperature** sensation below the lesion, but preservation of **proprioception** and **vibration sense**.
- It does not typically cause **saddle anesthesia** or **bladder dysfunction** to the extent seen in this patient.
*Conus medullaris syndrome*
- Conus medullaris syndrome involves the lower part of the spinal cord (T12-L2) and typically presents with **symmetric motor weakness**, **early onset bladder and bowel dysfunction**, and often **perianal numbness**.
- While there is bladder dysfunction, the described **asymmetric weakness** and prominent **radicular pain** radiating down one leg are more characteristic of cauda equina syndrome, which affects nerve roots rather than the spinal cord itself.
*Central cord syndrome*
- This syndrome usually results from hyperextension injuries and leads to **greater motor impairment in the upper extremities** than in the lower extremities.
- It is often associated with a **'shawl-like' distribution** of sensory loss and does not typically present with the same severe lower extremity weakness, saddle anesthesia, or bladder dysfunction as seen in this patient.
*Brown-Sequard syndrome*
- This syndrome is characterized by **hemisection of the spinal cord**, resulting in **ipsilateral motor paralysis** and loss of **proprioception and vibration sensation** below the level of the lesion.
- It also causes **contralateral loss of pain and temperature sensation** starting a few segments below the lesion, which does not match the patient's symptoms of bilateral sensory and motor deficits with saddle anesthesia.
Spinal cord organization US Medical PG Question 2: A 20-year-old man is brought to the emergency department 20 minutes after he sustained a stab wound to his back during an altercation. He reports weakness and numbness of the lower extremities. He has no history of serious illness. On arrival, he is alert and cooperative. His pulse is 90/min, and blood pressure is 100/65 mm Hg. Examination shows a deep 4-cm laceration on his back next to the vertebral column at the level of the T10 vertebra. Neurologic examination shows right-sided motor weakness with diminished vibratory sense ipsilaterally, decreased sensation to light touch at the level of his laceration and below, and left-sided loss of hot, cold, and pin-prick sensation at the level of the umbilicus and below. Deep tendon reflexes of his right lower extremity are 4+ and symmetrical. Babinski sign is absent bilaterally. The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Brown-Sequard syndrome (Correct Answer)
- B. Anterior cord syndrome
- C. Posterior cord syndrome
- D. Cauda equina syndrome
- E. Central cord syndrome
Spinal cord organization Explanation: ***Brown-Sequard syndrome***
- This syndrome is characterized by **ipsilateral motor paresis** and **loss of proprioception/vibration sensation**, along with **contralateral loss of pain and temperature sensation**.
- The patient's presentation of right-sided motor weakness and diminished vibratory sense ipsilaterally, coupled with left-sided loss of hot, cold, and pin-prick sensation, perfectly matches the classic signs of **Brown-Sequard syndrome** from a hemisection of the spinal cord (due to the stab wound).
*Anterior cord syndrome*
- This syndrome typically presents with **paraplegia or quadriplegia** and loss of pain and temperature sensation below the level of the lesion, with **preservation of proprioception and vibratory sensation**.
- The patient maintains **ipsilateral vibratory sensation** and has differential sensory loss, which is inconsistent with anterior cord syndrome where all distal sensation is broadly affected.
*Posterior cord syndrome*
- This syndrome is marked by a predominant loss of **proprioception and vibratory sensation** below the level of the lesion, with **preserved motor function** and pain/temperature sensation.
- The patient exhibits significant **motor weakness** and **contralateral loss of pain and temperature**, which are not typical features of posterior cord syndrome.
*Cauda equina syndrome*
- Cauda equina syndrome involves injury to the **nerve roots below the conus medullaris** and presents with **flaccid paralysis**, **saddle anesthesia**, and **bowel/bladder dysfunction**.
- The patient's presentation of spastic signs (4+ DTRs) and specific sensory deficits of a spinal cord lesion are inconsistent with the **lower motor neuron** signs of cauda equina syndrome.
*Central cord syndrome*
- This syndrome typically results in **greater motor impairment in the upper extremities than in the lower extremities**, along with a **variable sensory loss** below the level of the lesion, often involving a "cape-like" distribution of sensory loss.
- The patient's injury is at T10, and while there is motor weakness, the specific pattern of ipsilateral motor with contralateral pain/temperature loss is not characteristic of central cord syndrome, which usually affects the cervical region and has a different motor pattern.
Spinal cord organization US Medical PG Question 3: A 22-year-old man is rushed to the emergency department after a motor vehicle accident. The patient states that he feels weakness and numbness in both of his legs. He also reports pain in his lower back. His airway, breathing, and circulation is intact, and he is conversational. Neurologic exam is significant for bilateral lower extremity flaccid paralysis and impaired pain and temperature sensation up to T10-T11 with normal vibration sense. A computerized tomography scan of the spine is performed which shows a vertebral burst fracture of the vertebral body at the level of T11. Which of the following findings is most likely present in this patient?
- A. Intact vibration sense
- B. Bowel incontinence (Correct Answer)
- C. Flaccid paralysis at the level of the lesion
- D. Spasticity below the lesion
- E. Impaired proprioception sense
Spinal cord organization Explanation: ***Bowel incontinence***
- The presented symptoms of acute **bilateral lower extremity flaccid paralysis**, **impaired pain and temperature sensation**, and a T11 **vertebral burst fracture** are highly indicative of **anterior cord syndrome**.
- **Anterior cord syndrome** characteristically involves damage to the **anterior two-thirds of the spinal cord**, affecting the **corticospinal tracts** (motor control), **spinothalamic tracts** (pain and temperature sensation), and the **autonomic fibers** that control bladder and bowel function, leading to **bowel and bladder dysfunction**.
*Intact vibration sense*
- The sensation of **vibration** and **proprioception** is carried by the **dorsal columns** (posterior part of the spinal cord), which are typically **spared** in **anterior cord syndrome**.
- Therefore, **intact vibration sense** is an expected finding, but the question asks for the **most likely finding** that represents a significant complication of the syndrome.
*Flaccid paralysis at the level of the lesion*
- While **flaccid paralysis** is present in the lower extremities, it occurs **below the level of the lesion** due to damage to the descending motor tracts (corticospinal tracts).
- Flaccid paralysis *at* the level of the lesion would typically involve damage to the **lower motor neurons** at that specific segment, which is not the primary feature described for a burst fracture causing **anterior cord syndrome**.
*Spasticity below the lesion*
- **Spasticity** typically develops much **later** in spinal cord injuries, after the initial phase of **spinal shock** resolves (usually weeks to months).
- In the acute phase following a significant spinal cord injury, **flaccid paralysis** is the more common finding below the lesion, reflecting spinal shock.
*Impaired proprioception sense*
- Similar to vibration sense, **proprioception** is primarily mediated by the **dorsal columns**, which are generally **spared** in **anterior cord syndrome**.
- Therefore, **proprioception** would likely be **intact**, not impaired, in this specific type of spinal cord injury.
Spinal cord organization US Medical PG Question 4: A 47-year-old man comes to the emergency department because of urinary and fecal incontinence for 6 hours. Earlier in the day, he suffered a fall at a construction site and sustained injuries to his back and thighs but did not seek medical attention. He took ibuprofen for lower back pain. His temperature is 36.9°C (98.4°F), pulse is 80/min, and blood pressure is 132/84 mm Hg. Examination shows tenderness over the lumbar spine, bilateral lower extremity weakness, absent ankle jerk reflexes, and preserved patellar reflexes. There is decreased rectal tone. An ultrasound of the bladder shows a full bladder. Which of the following is the most likely diagnosis?
- A. Cerebellar stroke
- B. Spinal epidural abscess
- C. Anterior spinal cord syndrome
- D. Conus medullaris syndrome (Correct Answer)
- E. Brown-Sequard syndrome
Spinal cord organization Explanation: ***Conus medullaris syndrome***
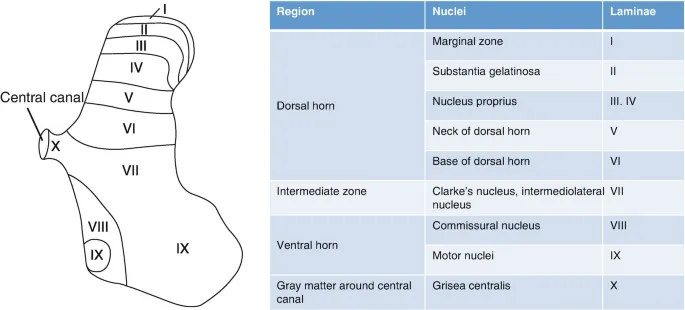
- The combination of **bilateral lower extremity weakness**, **urinary and fecal incontinence**, **decreased rectal tone**, and a **full bladder** is characteristic of conus medullaris syndrome. This syndrome results from damage to the **conus medullaris** (the terminal part of the spinal cord), which typically involves the **S3-S5 nerve roots**.
- **Absent ankle jerk reflexes** (S1-S2) with **preserved patellar reflexes** (L2-L4) further pinpoints the lesion to the lower lumbar/sacral spinal cord segments, consistent with conus medullaris involvement. The recent **fall with back injury** is a predisposing factor.
*Cerebellar stroke*
- **Cerebellar stroke** would primarily manifest with symptoms of **ataxia**, **dysarthria**, **nystagmus**, and **vertigo**, without direct involvement of bladder/bowel function or specific lower extremity reflex abnormalities as described.
- While a stroke can cause weakness, it would typically be **unilateral** or involve specific cortical patterns, and not generally present with this constellation of lower spinal cord signs.
*Spinal epidural abscess*
- A **spinal epidural abscess** would typically present with **fever**, **severe localized back pain**, and progressive **neurological deficits**, often following an infection or recent spinal procedure.
- While it can cause neurological deficits similar to the conus medullaris syndrome, the absence of **fever** and the acute onset following trauma makes an abscess less likely in this scenario.
*Anterior spinal cord syndrome*
- **Anterior spinal cord syndrome** primarily affects the **anterior two-thirds of the spinal cord**, leading to **motor paralysis** below the lesion and **loss of pain and temperature sensation**, while **proprioception** and **vibration sense are preserved**.
- Although it can cause motor weakness and bladder dysfunction, the isolated loss of ankle jerk reflexes with preserved patellar reflexes and the specific pattern of incontinence are more indicative of conus medullaris involvement.
*Brown-Sequard syndrome*
- **Brown-Séquard syndrome** is characterized by **ipsilateral motor paralysis** and loss of **proprioception/vibration sensation**, along with **contralateral loss of pain and temperature sensation** below the level of the lesion, due to hemisection of the spinal cord.
- This patient presents with **bilateral weakness** and specific bladder/bowel dysfunction, which is inconsistent with the typical lateralized deficits seen in Brown-Séquard syndrome.
Spinal cord organization US Medical PG Question 5: A 22-year-old man is brought to the emergency department after he was impaled by a metal rod during a work accident. The rod went into his back around the level of T9 but was removed before arrival. He has no past medical history and does not take any medications. On physical examination, he has significant muscle weakness in his entire left lower body. He also exhibits impaired vibration and proprioception in his left leg as well as loss of pain and temperature sensation in his right leg. Which of the following sections of the spinal cord was most likely damaged in this patient?
- A. Posterior cord
- B. Anterior cord
- C. Left hemicord (Correct Answer)
- D. Central cord
- E. Right hemicord
Spinal cord organization Explanation: ***Left hemicord***
- The combination of **ipsilateral motor weakness** and **loss of vibration/proprioception** (damage to the **corticospinal tract** and **dorsal column**) along with **contralateral loss of pain/temperature** (damage to the **spinothalamic tract**) is the classic presentation of **Brown-Séquard syndrome**, which results from a lesion affecting one side (hemicord) of the spinal cord.
- The injury at **T9** is consistent with lower body symptoms, as tracts for the legs would be affected at this level.
*Posterior cord*
- Damage to the **posterior cord** primarily affects the **dorsal columns**, leading to **ipsilateral loss of vibration and proprioception**.
- It would not explain the **ipsilateral motor weakness** or the **contralateral loss of pain and temperature sensation**.
*Anterior cord*
- **Anterior cord syndrome** typically presents with **bilateral loss of motor function** (due to damage to the corticospinal tracts) and **bilateral loss of pain and temperature sensation** (due to damage to the spinothalamic tracts).
- **Vibration and proprioception** are usually preserved because the dorsal columns are spared.
*Central cord*
- **Central cord syndrome** most commonly results from hyperextension injuries, particularly in the cervical spine, affecting the central gray matter.
- It typically causes greater **weakness in the upper extremities** than the lower extremities and a variable sensory loss, often in a **"cape-like" distribution**.
*Right hemicord*
- A **right hemicord** lesion would cause **right-sided motor weakness** and **loss of vibration/proprioception**, along with **left-sided loss of pain/temperature sensation**.
- The patient's symptoms are on the **left side for motor/proprioception** and the **right side for pain/temperature**, indicating a left hemicord lesion.
Spinal cord organization US Medical PG Question 6: An MRI of a patient with low back pain reveals compression of the L5 nerve root. Which of the following muscles would most likely show weakness during physical examination?
- A. Tibialis posterior
- B. Tibialis anterior (Correct Answer)
- C. Gastrocnemius
- D. Quadriceps femoris
Spinal cord organization Explanation: ***Tibialis anterior***
- The **L5 nerve root** primarily innervates muscles responsible for **dorsiflexion** of the foot, with the **tibialis anterior** being the primary dorsiflexor.
- Weakness of the tibialis anterior would manifest as difficulty lifting the front of the foot, potentially leading to a **foot drop** gait.
*Tibialis posterior*
- The **tibialis posterior** is primarily innervated by the **tibial nerve** (S1-S2) and is responsible for **plantarflexion** and **inversion** of the foot.
- Weakness in this muscle would not be the most likely presentation of L5 nerve root compression.
*Gastrocnemius*
- The **gastrocnemius** muscle is primarily innervated by the **tibial nerve** (S1-S2) and is a powerful **plantarflexor** of the foot.
- Weakness in this muscle would indicate an S1 or S2 nerve root issue, not typically L5.
*Quadriceps femoris*
- The **quadriceps femoris** is innervated by the **femoral nerve**, predominantly originating from the **L2, L3, and L4 nerve roots**.
- Weakness would manifest as difficulty extending the knee, which is not characteristic of L5 compression.
Spinal cord organization US Medical PG Question 7: Where does the only cranial nerve without a thalamic relay nucleus enter the skull?
- A. Superior orbital fissure
- B. Internal auditory meatus
- C. Foramen rotundum
- D. Jugular foramen
- E. Cribriform plate (Correct Answer)
Spinal cord organization Explanation: ***Cribriform plate***
- The **olfactory nerve (CN I)** is the only cranial nerve that does not have a thalamic relay nucleus before reaching the cerebral cortex.
- It passes through the **cribriform plate** of the ethmoid bone to reach the olfactory bulbs.
*Superior orbital fissure*
- This opening transmits the **oculomotor (CN III), trochlear (CN IV), ophthalmic division of trigeminal (CN V1)**, and **abducens (CN VI)** nerves.
- These nerves all have sensory or motor components that relay through the thalamus, directly or indirectly.
*Internal auditory meatus*
- This canal transmits the **facial (CN VII)** and **vestibulocochlear (CN VIII)** nerves.
- The vestibulocochlear nerve's auditory pathway involves a thalamic relay in the **medial geniculate nucleus**.
*Foramen rotundum*
- The **maxillary division of the trigeminal nerve (CN V2)** passes through the foramen rotundum.
- Sensory information carried by CN V2 relays through the **thalamus**.
*Jugular foramen*
- This opening transmits the **glossopharyngeal (CN IX), vagus (CN X)**, and **accessory (CN XI)** nerves.
- Sensory components of these nerves, particularly taste and visceral sensation, involve thalamic nuclei.
Spinal cord organization US Medical PG Question 8: A 55-year-old construction worker falls off a 2-story scaffolding and injures his back. His coworkers bring him to the urgent care clinic within 30 minutes of the fall. He complains of left lower-limb weakness and loss of sensation in the right lower limb. He does not have any past medical history. His vital signs are stable. A neurologic examination reveals a total loss of motor function when testing left knee extension, along with the left-sided loss of light touch sensation from the mid-thigh and below. There is a right-sided loss of pin-prick sensation of the lateral leg and entire foot. At this time of acute injury, what other finding is most likely to be found in this patient?
- A. Left-sided extensor plantar response
- B. Intact voluntary anal contraction
- C. Left-sided spastic paralysis below the lesion
- D. Left-sided numbness at the level of the lesion
- E. Left-sided loss of proprioception and vibration sensation (Correct Answer)
Spinal cord organization Explanation: ***Left-sided loss of proprioception and vibration sensation***
- The presented symptoms (left lower-limb weakness/motor loss, left-sided loss of light touch, and right-sided loss of pin-prick sensation) are classic for **Brown-Séquard syndrome**, resulting from a **hemicord lesion on the LEFT side**.
- **Proprioception** and **vibration sensation** are carried by the **dorsal columns**, which ascend **ipsilaterally** (same side) in the spinal cord and decussate in the **medulla** (lower brainstem).
- Therefore, a lesion on the **left side** of the spinal cord would result in **ipsilateral (left-sided) loss** of proprioception and vibration sensation below the level of the lesion.
- The right-sided loss of pain/temperature occurs because the spinothalamic tract decussates at the spinal level of entry, making pain/temperature deficits contralateral to the lesion.
*Left-sided extensor plantar response*
- An **extensor plantar response (Babinski sign)**, indicating an upper motor neuron lesion, is typically present in the **chronic phase** of spinal cord injury.
- In the **acute phase (spinal shock)**, **flaccid paralysis** and **absent reflexes** are more common, not hyperreflexia or Babinski signs.
*Intact voluntary anal contraction*
- **Voluntary anal contraction** indicates preserved sacral spinal cord function, which is assessed to determine if an injury is **complete or incomplete**.
- Given the severe motor and sensory deficits described, this would suggest an incomplete lesion, but the classic Brown-Séquard presentation makes this less likely as the primary finding.
*Left-sided spastic paralysis below the lesion*
- **Spastic paralysis** is a sign of an upper motor neuron lesion that emerges **weeks to months** after the initial injury, typically after spinal shock resolves.
- In the **acute phase (spinal shock)**, the patient would experience **flaccid paralysis** and hyporeflexia below the level of the lesion.
*Left-sided numbness at the level of the lesion*
- Sensory loss **at the level of the lesion** can occur due to damage to the dorsal horn at that specific spinal segment.
- However, the question describes **left-sided loss of light touch from the mid-thigh down**, which represents loss **below** the lesion level.
- **Brown-Séquard syndrome** can cause a narrow band of bilateral sensory loss at the lesion level, but the most clinically significant and testable finding in the acute phase is the **ipsilateral loss of proprioception and vibration** below the lesion.
Spinal cord organization US Medical PG Question 9: Fibers from the marked structure terminate at which of the following?
- A. Red nucleus (Correct Answer)
- B. Subthalamus
- C. Inferior olivary nucleus
- D. Fastigial nucleus
Spinal cord organization Explanation: ***Red nucleus***
- The arrow points to the **superior cerebellar peduncle**, which contains efferent fibers from the **dentate nucleus** of the cerebellum.
- A major projection of the superior cerebellar peduncle is to the **contralateral red nucleus**, forming part of the **dentato-rubro-thalamic pathway**.
*Subthalamus*
- The subthalamus is part of the **diencephalon** and is involved in motor control as part of the **basal ganglia circuit**.
- It does not receive direct efferent projections from the cerebellum via the superior cerebellar peduncle.
*Inferior olivary nucleus*
- The inferior olivary nucleus is a major source of **climbing fibers** to the cerebellum, providing **afferent input** for motor learning and coordination.
- It does not receive direct efferent output from the cerebellum's deep nuclei via the superior cerebellar peduncle.
*Fastigial nucleus*
- The fastigial nucleus is one of the **deep cerebellar nuclei**, located medially.
- Its primary efferent projections are via the **inferior cerebellar peduncle** to the vestibular nuclei and reticular formation, not typically receiving fibers from the superior cerebellar peduncle.
Spinal cord organization US Medical PG Question 10: A 38-year-old man comes to the physician for a follow-up examination. He has quadriparesis as a result of a burst fracture of the cervical spine that occurred after a fall from his roof 1 month ago. He has urinary and bowel incontinence. He appears malnourished. His temperature is 37.1°C (98.8°F), pulse is 88/min, and blood pressure is 104/60 mm Hg. Examination shows spasticity in all extremities. Muscle strength is decreased in proximal and distal muscle groups bilaterally. Deep tendon reflexes are 4+ bilaterally. Plantar reflex shows extensor response bilaterally. Sensation to pinprick and temperature is absent below the neck. Sensation to vibration, position, and light touch is normal bilaterally. Rectal tone is decreased. There is a 1-cm area of erythema over the sacrum. Which of the following is the most likely cause of this patient's symptoms?
- A. Hemi-transection of the spinal cord
- B. Cavitation within the spinal cord
- C. Injury to gray matter of the spinal cord
- D. Occlusion of the posterior spinal artery
- E. Damage to the anterior spinal artery (Correct Answer)
Spinal cord organization Explanation: ***Damage to the anterior spinal artery***
- This typically results in **anterior cord syndrome**, characterized by bilateral loss of pain and temperature sensation, motor function (quadriparesis), and autonomic dysfunction (bowel/bladder incontinence below the level of injury).
- The **preservation of posterior column functions** (vibration, proprioception, light touch) is a hallmark of anterior spinal artery ischemia, as the posterior columns are supplied by the posterior spinal arteries.
*Hemi-transection of the spinal cord*
- This describes **Brown-Séquard syndrome**, which involves ipsilateral loss of motor function, vibration, and proprioception, and contralateral loss of pain and temperature sensation.
- The patient's symptoms are inconsistent with Brown-Séquard syndrome due to the **bilateral presentation of motor and sensory deficits**.
*Cavitation within the spinal cord*
- This condition, known as **syringomyelia**, typically presents with a **cape-like distribution of pain and temperature loss** (due to central cord involvement affecting the decussating spinothalamic fibers).
- It would usually spare motor function initially and would not explain the sudden, severe quadriparesis and complete sensory loss described.
*Injury to gray matter of the spinal cord*
- Isolated gray matter injury, often seen in conditions like **central cord syndrome**, primarily affects the pain and temperature pathways and may cause upper extremity weakness.
- It would not explain the **complete loss of motor function and pain/temperature sensation below the neck** while preserving posterior column function.
*Occlusion of the posterior spinal artery*
- Occlusion of the posterior spinal artery would primarily affect the **dorsal columns**, leading to loss of vibration, proprioception, and light touch.
- This patient, however, has **preserved sensation to vibration, position, and light touch**, making posterior spinal artery occlusion unlikely.
More Spinal cord organization US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.