Sensory pathways US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Sensory pathways. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Sensory pathways US Medical PG Question 1: A 58-year-old woman presents to the clinic with an abnormal sensation on the left side of her body that has been present for the past several months. At first, the area seemed numb and she recalls touching a hot stove and accidentally burning herself but not feeling the heat. Now she is suffering from a constant, uncomfortable burning pain on her left side for the past week. The pain gets worse when someone even lightly touches that side. She has recently immigrated and her past medical records are unavailable. Last month she had a stroke but she cannot recall any details from the event. She confirms a history of hypertension, type II diabetes mellitus, and bilateral knee pain. She also had cardiac surgery 20 years ago. She denies fever, mood changes, weight changes, and trauma to the head, neck, or limbs. Her blood pressure is 162/90 mm Hg, the heart rate is 82/min, and the respiratory rate is 15/min. Multiple old burn marks are visible on the left hand and forearm. Muscle strength is mildly reduced in the left upper and lower limbs. Hyperesthesia is noted in the left upper and lower limbs. Laboratory results are significant for:
Hemoglobin 13.9 g/dL
MCV 92 fL
White blood cells 7,500/mm3
Platelets 278,000/mm3
Creatinine 1.3 U/L
BUN 38 mg/dL
TSH 2.5 uU/L
Hemoglobin A1c 7.9%
Vitamin B12 526 ng/L
What is the most likely diagnosis?
- A. Conversion disorder
- B. Complex regional pain syndrome
- C. Dejerine-Roussy syndrome (Correct Answer)
- D. Medial medullary syndrome
- E. Subacute combined degeneration of spinal cord
Sensory pathways Explanation: ***Dejerine-Roussy syndrome***
- The patient's symptoms of **contralateral hemianesthesia**, followed by **dysesthesia**, **spontaneous burning pain**, and **allodynia/hyperalgesia**, developing after a stroke a month prior, are classic for **Dejerine-Roussy syndrome** (thalamic pain syndrome). The history of unnoticed burns and hyperesthesia supports this.
- This syndrome is caused by a lesion in the **thalamus**, typically due to a stroke, which disrupts sensory pathways and leads to an abnormal processing of sensory information.
*Conversion disorder*
- Conversion disorder involves neurological symptoms that are **incompatible with recognized neurological or medical conditions** and are often associated with psychological stress.
- The patient's symptoms are clearly attributable to a known neurological etiology (a recent stroke) and specific anatomical location (thalamus), ruling out conversion disorder.
*Complex regional pain syndrome*
- **Complex regional pain syndrome (CRPS)** is characterized by severe pain, swelling, and autonomic dysfunction, typically affecting a **single limb distal to an injury**, but not necessarily associated with a stroke to the brain.
- While the patient has burning pain and hyperesthesia, the **hemibody distribution** and clear link to a prior stroke make CRPS less likely than a central lesion.
*Medial medullary syndrome*
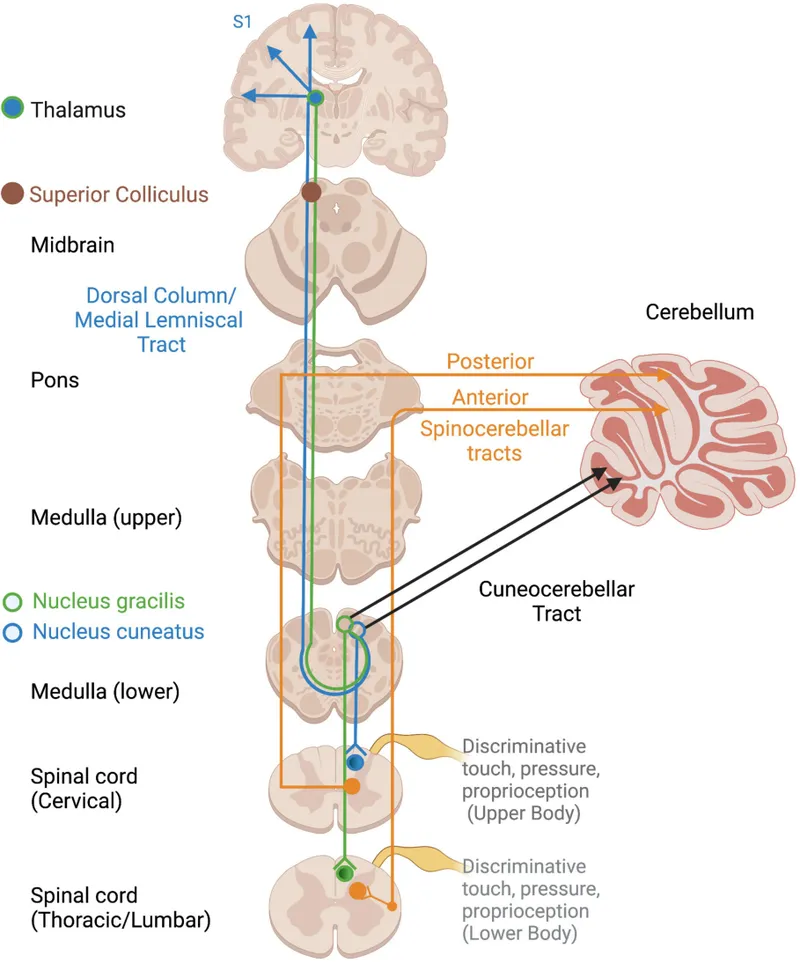
- **Medial medullary syndrome** results from damage to the medial medulla and typically presents with **ipsilateral tongue weakness**, **contralateral hemiparesis**, and **contralateral loss of vibratory and proprioceptive sensation**, but not the prominent burning pain and allodynia described.
- The patient's primary sensory complaints of burning pain and hyperesthesia across an entire hemibody are not characteristic of medial medullary syndrome.
*Subacute combined degeneration of spinal cord*
- **Subacute combined degeneration** is caused by **vitamin B12 deficiency** and affects the dorsal and lateral columns of the spinal cord, leading to **paresthesias**, weakness, gait ataxia, and impaired proprioception.
- The patient's **vitamin B12 level is normal**, and the symptoms are acute-onset and unilateral, clearly linked to a stroke, not a progressive, symmetrical myelopathy.
Sensory pathways US Medical PG Question 2: A 58-year-old man comes to the physician because of burning pain in his neck and arms for a year. He has also had paresthesias in his hands during this period. He has had increasing weakness in both hands during the past 3 months. He has type 2 diabetes mellitus, hypercholesterolemia, and hypertension. He was involved in a motor vehicle collision 3 years ago. Current medications include metformin, sitagliptin, enalapril, atorvastatin, and aspirin. He has had 7 sexual partners in his lifetime; he uses condoms inconsistently. He is oriented to time, place, and person. Vital signs are within normal limits. The pupils are equal and reactive to light. Examination of the upper extremities shows decreased muscle strength, absent reflexes, and decreased hand grip with fasciculations bilaterally. Sensation to temperature and pain is absent over the chest and bilateral upper arms. Vibration and joint position sensations are present in the upper limbs. Cranial nerve examination shows no focal findings. Examination of the lower extremities show no abnormalities. Which of the following is the most likely diagnosis?
- A. Brown-Séquard syndrome
- B. Tabes dorsalis
- C. Multiple sclerosis
- D. Syringomyelia (Correct Answer)
- E. Cervical disk prolapse
Sensory pathways Explanation: ***Syringomyelia***
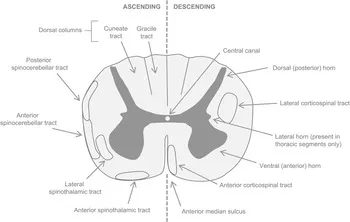
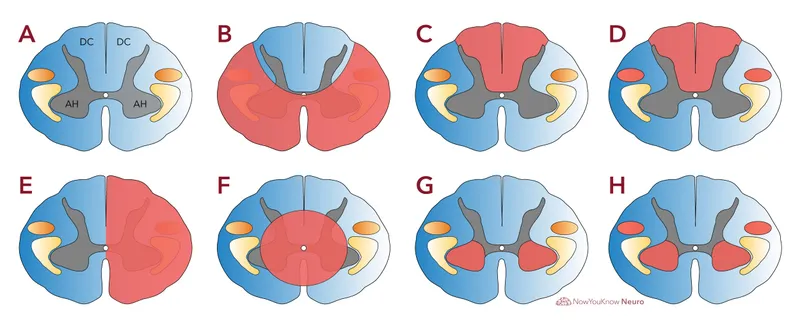
- This condition is characterized by a central canal cavitation (syrinx) in the spinal cord, leading to damage to the **spinothalamic tracts** (loss of pain and temperature sensation) and anterior horn cells (weakness, fasciculations, absent reflexes). The **'cape-like' distribution** of sensory loss over the chest and arms, along with hand weakness, is classic.
- The sensation loss to temperature and pain over the chest and bilateral upper arms with preserved vibration and joint position sensation in upper limbs is a **dissociated sensory loss**, a hallmark of syringomyelia, as the dorsal columns (responsible for vibration and proprioception) are typically spared.
*Brown-Séquard syndrome*
- This syndrome results from **hemitransaction of the spinal cord**, causing ipsilateral loss of motor function and proprioception/vibration sensation, and contralateral loss of pain and temperature sensation below the lesion.
- The patient's symptoms of **bilateral sensory loss** and **bilateral weakness** do not fit this unilateral lesion pattern.
*Tabes dorsalis*
- This is a late manifestation of **syphilis**, primarily affecting the posterior columns of the spinal cord (dorsal columns), leading to loss of **proprioception and vibration sensation**, along with ataxia and shooting pains.
- The patient presents with loss of pain and temperature sensation, not primarily proprioception and vibration, and has **motor weakness with fasciculations**, which are not typical for tabes dorsalis.
*Multiple sclerosis*
- MS is characterized by **demyelination in the central nervous system**, presenting with diverse neurological symptoms that often wax and wane, affecting multiple areas of the brain and spinal cord.
- While it can cause sensory and motor deficits, the **dissociated sensory loss** (pain/temperature vs. vibration/proprioception) in a "cape-like" distribution with prominent fasciculations points away from MS.
*Cervical disk prolapse*
- A cervical disk prolapse typically causes **radicular pain and neurological deficits** (motor weakness, sensory loss, reflex changes) in a dermatomal or myotomal distribution corresponding to the compressed nerve root.
- While it can cause arm pain and weakness, the **bilateral, "cape-like" dissociated sensory loss** over the chest and arms is not characteristic of a single or multiple cervical nerve root compressions.
Sensory pathways US Medical PG Question 3: A 17-year-old boy is brought to the emergency department after being stabbed with a knife during an altercation. Physical examination shows a 4-cm stab wound on the right lateral border of the T1 spinous process. An MRI of the spinal cord shows damage to the area of the right lateral corticospinal tract at the level of T1. Further evaluation will most likely show which of the following findings?
- A. Absence of right-sided motor function below T1 (Correct Answer)
- B. Absence of left-sided proprioception below T1
- C. Presence of left-sided Babinski sign
- D. Absence of left-sided fine touch sensation below T1
- E. Absence of right-sided temperature sensation below T1
Sensory pathways Explanation: ***Absence of right-sided motor function below T1***
- The **right lateral corticospinal tract** controls **voluntary motor function** on the **ipsilateral side** of the body.
- Damage to this tract at T1 would therefore lead to a loss of motor function on the right side below the level of the injury.
*Absence of left-sided proprioception below T1*
- **Proprioception** is carried by the **dorsal columns**, which ascend **ipsilaterally** before decussating in the brainstem.
- Damage to the right lateral corticospinal tract would not affect left-sided proprioception.
*Presence of left-sided Babinski sign*
- A **Babinski sign** (upgoing plantar reflex) indicates an **upper motor neuron lesion**.
- Since the corticospinal tract decussates in the **medulla** (before reaching the spinal cord), a lesion in the **right lateral corticospinal tract at T1** affects motor function on the **right side** of the body.
- Therefore, if a Babinski sign were present, it would be on the **right side**, not the left.
*Absence of left-sided fine touch sensation below T1*
- **Fine touch** sensation is transmitted by the **dorsal columns**, which ascend **ipsilaterally** and decussate in the brainstem.
- Damage to the right lateral corticospinal tract would not affect fine touch sensation on the left side.
*Absence of right-sided temperature sensation below T1*
- **Temperature sensation** is carried by the **spinothalamic tracts**, which decussate at the level of entry into the spinal cord.
- Therefore, a lesion of the right lateral corticospinal tract would not affect temperature sensation on the right side; ipsilateral temperature loss would be due to damage to the right spinothalamic tract, which is located more anterolaterally in the spinal cord.
Sensory pathways US Medical PG Question 4: A 72-year-old woman is brought in to the emergency department after her husband noticed that she appeared to be choking on her dinner. He performed a Heimlich maneuver but was concerned that she may have aspirated something. The patient reports a lack of pain and temperature on the right half of her face, as well as the same lack of sensation on the left side of her body. She also states that she has been feeling "unsteady" on her feet. On physical exam you note a slight ptosis on the right side. She is sent for an emergent head CT. Where is the most likely location of the neurological lesion?
- A. Pons
- B. Internal capsule
- C. Cervical spinal cord
- D. Medulla (Correct Answer)
- E. Midbrain
Sensory pathways Explanation: ***Medulla***
- This presentation describes **Wallenberg syndrome** (lateral medullary syndrome), characterized by **ipsilateral facial sensory loss**, **contralateral body sensory loss**, and **ataxia** due to involvement of the spinothalamic tracts, trigeminal nucleus, and cerebellar pathways.
- **Dysphagia** (choking) and **Horner's syndrome** (ptosis, miosis, anhidrosis) are also classic signs, specifically the ptosis seen here, pointing to an infarct in the **lateral medulla**.
*Pons*
- Lesions in the pons typically present with varying degrees of **cranial nerve deficits** (e.g., trigeminal, abducens, facial) and **motor or sensory deficits** affecting both sides of the body due to the decussation of tracts.
- The specific combination of **crossed sensory loss** and other symptoms seen here is not characteristic of isolated pontine lesions.
*Internal capsule*
- A lesion in the internal capsule would primarily cause **contralateral motor weakness (hemiparesis)** and **sensory loss** affecting both the face and body on the same side, without the ipsilateral facial involvement.
- It would not explain the **ataxia** or specific cranial nerve signs like ptosis.
*Cervical spinal cord*
- Spinal cord lesions result in **sensory and motor deficits below the level of the lesion**, affecting both sides of the body symmetrically, or ipsilaterally depending on the tract involved.
- They do not cause **facial sensory disturbances**, **dysphagia**, or **ataxia** in the manner described.
*Midbrain*
- Midbrain lesions typically involve the **oculomotor nerve** (CN III), causing eye movement abnormalities, and can result in **contralateral hemiparesis**.
- They do not produce the **crossed sensory deficits** (ipsilateral face, contralateral body) or **ataxia** characteristic of this case.
Sensory pathways US Medical PG Question 5: A 37-year-old man presents to his primary care provider complaining of bilateral arm numbness. He was involved in a motor vehicle accident 3 months ago. His past medical history is notable for obesity and psoriatic arthritis. He takes adalimumab. His temperature is 99.3°F (37.4°C), blood pressure is 130/85 mmHg, pulse is 90/min, and respirations are 18/min. On exam, superficial skin ulcerations are found on his fingers bilaterally. His strength is 5/5 bilaterally in shoulder abduction, arm flexion, arm extension, wrist extension, finger abduction, and thumb flexion. He demonstrates loss of light touch and pinprick response in the distal tips of his 2nd and 5th fingertips and over the first dorsal web space. Vibratory sense is intact in the bilateral upper and lower extremities. Which of the following nervous system structures is most likely affected in this patient?
- A. Cuneate fasciculus
- B. Ventral horns
- C. Anterior corticospinal tract
- D. Spinocerebellar tract
- E. Ventral white commissure (Correct Answer)
Sensory pathways Explanation: ***Ventral white commissure***
- The patient presents with **bilateral loss of pain (pinprick) and light touch sensation** in the upper extremity fingertips, while **vibratory sense is intact** and **motor strength is fully preserved (5/5)**. This dissociated sensory loss pattern is pathognomonic for a lesion affecting the **ventral white commissure**.
- The ventral white commissure contains **decussating fibers of the spinothalamic tract**, which carry pain and temperature sensation from the contralateral body. A lesion here (classically seen in **syringomyelia** affecting the cervical spinal cord) causes **bilateral loss of pain and temperature sensation** in a characteristic distribution while **sparing the dorsal columns** (vibratory sense and proprioception remain intact) and motor pathways.
- The **superficial skin ulcerations** on his fingers are explained by chronic loss of protective pain sensation, leading to unnoticed repetitive trauma. The motor vehicle accident 3 months ago may have precipitated or worsened an underlying syrinx.
- This is the classic **"cape-like" or suspended sensory loss** pattern, though it can present with focal dermatomal involvement as in this case.
*Cuneate fasciculus*
- The cuneate fasciculus is part of the **dorsal column-medial lemniscal pathway** that carries **vibratory sense, proprioception, and fine discriminative touch** from the upper extremities.
- A lesion here would cause **loss of vibratory sense** and proprioception, which are explicitly **intact** in this patient, making this option incorrect.
*Ventral horns*
- The ventral horns contain **lower motor neuron cell bodies** that innervate skeletal muscles.
- Damage would cause **motor deficits** including weakness (reduced strength), muscle atrophy, and fasciculations, none of which are present in this patient who has normal 5/5 strength throughout.
*Anterior corticospinal tract*
- This tract mediates **voluntary motor control**, primarily of axial and proximal muscles.
- Lesions would result in **motor weakness or spasticity**, not the isolated sensory deficits seen in this patient.
*Spinocerebellar tract*
- The spinocerebellar tracts carry **unconscious proprioceptive information** to the cerebellum for motor coordination.
- Damage would manifest as **ataxia, dysmetria, and incoordination**, which are not described in this patient's presentation.
Sensory pathways US Medical PG Question 6: A 28-year-old man presents with visual disturbances. He says that he is having double vision since he woke up this morning. His past medical history is insignificant except for occasional mild headaches. The patient is afebrile and his vitals are within normal limits. On physical examination of his eyes, there is paralysis of left lateral gaze. Also, at rest, there is esotropia of the left eye. A noncontrast CT scan of the head reveals a tumor impinging on one of his cranial nerves. Which of the following nerves is most likely affected?
- A. Trigeminal nerve
- B. Optic nerve
- C. Oculomotor nerve
- D. Trochlear nerve
- E. Abducens nerve (Correct Answer)
Sensory pathways Explanation: ***Abducens nerve***
- **Paralysis of left lateral gaze** and **esotropia** (inward turning of the eye) at rest are classic signs of a **left abducens nerve (CN VI) palsy**. This nerve exclusively innervates the **lateral rectus muscle**, which is responsible for abducting (moving outward) the eye.
- Impingement from a **tumor** is a common cause of cranial nerve palsies, and the presentation perfectly matches the function of the abducens nerve.
*Trigeminal nerve*
- The **trigeminal nerve (CN V)** is responsible for **facial sensation** and **mastication** (chewing).
- Dysfunction would present as facial numbness, pain, or weakness in chewing, not visual disturbances or eye movement issues.
*Optic nerve*
- The **optic nerve (CN II)** transmits **visual information** from the retina to the brain.
- Lesions typically cause **vision loss** (e.g., blindness, scotoma, visual field defects), not double vision or eye movement paralysis.
*Oculomotor nerve*
- The **oculomotor nerve (CN III)** controls most **extraocular muscles** (medial, superior, inferior rectus, inferior oblique) and the **levator palpebrae superioris** (eyelid elevation), as well as pupillary constriction.
- A palsy would typically present with a **"down and out" eye**, **ptosis** (drooping eyelid), and **mydriasis** (dilated pupil), which are not described.
*Trochlear nerve*
- The **trochlear nerve (CN IV)** innervates the **superior oblique muscle**, which depresses and intorts the eye.
- A palsy typically causes **vertical double vision**, especially when looking down and inward, and a compensatory head tilt away from the affected side. This does not match the described lateral gaze paralysis.
Sensory pathways US Medical PG Question 7: A 63-year-old man presents to the clinic concerned about numbness and weakness in his bilateral shoulders and arms for the past 8 weeks. The symptoms started when he fell from scaffolding at work and landed on his back. Initial workup was benign and he returned to normal duty. However, his symptoms have progressively worsened since the fall. He denies fever, back pain, preceding vomiting, and diarrhea. He has a history of type 2 diabetes mellitus, hypertension, hypercholesterolemia, ischemic heart disease, and a 48-pack-year cigarette smoking history. He takes atorvastatin, hydrochlorothiazide, lisinopril, labetalol, and metformin. His blood pressure is 132/82 mm Hg, the pulse is 72/min, and the respiratory rate is 15/min. All cranial nerves are intact. Muscle strength is reduced in the upper limbs (4/5 bilaterally) but normal in the lower limbs. Perception of sharp stimuli and temperature is reduced on his shoulders and upper arms. The vibratory sense is preserved. Sensory examination is normal in the lower limbs. What is the most likely diagnosis?
- A. Anterior cord syndrome
- B. Central cord syndrome (Correct Answer)
- C. Guillain-Barre syndrome
- D. Vitamin B12 deficiency
- E. Pontine infarction
Sensory pathways Explanation: ***Central cord syndrome***
- This syndrome typically results from a **hyperextension injury** in patients with pre-existing cervical spinal stenosis, leading to damage to the central gray matter and surrounding tracts.
- It classically presents with greater **motor weakness in the upper extremities** than in the lower extremities, and a **"cape-like" distribution of sensory loss** (impaired pain and temperature sensation) over the shoulders and arms due to spinothalamic tract involvement, as seen in this patient.
*Anterior cord syndrome*
- This syndrome is characterized by **paraplegia/quadriplegia**, dissociated sensory loss (loss of **pain and temperature sensation**), and bowel/bladder dysfunction below the level of the lesion.
- It spares **proprioception and vibratory sensation** since the posterior columns remain intact, which is not fully consistent with the patient's presentation of primarily sensory symptoms in the upper limbs with normal strength.
*Guillain-Barre syndrome*
- This is an **acute demyelinating polyneuropathy** that typically presents with **progressive, ascending weakness** and often **areflexia**, usually following an infection.
- The patient's symptoms are primarily sensory, descending, and lack significant weakness or preceding infection, making this diagnosis less likely.
*Vitamin B12 deficiency*
- This deficiency can cause **subacute combined degeneration** of the spinal cord, affecting the **posterior columns** (vibratory and proprioception loss) and **corticospinal tracts** (weakness, spasticity).
- The patient primarily has loss of pain and temperature sensation with preserved vibratory sense and normal strength, which is inconsistent with B12 deficiency.
*Pontine infarction*
- A pontine infarction would present with a constellation of cranial nerve deficits, motor weakness (hemiparesis or quadriplegia), and cerebellar signs due to its location in the brainstem.
- The patient has intact cranial nerves, normal muscle strength, and specific sensory deficits limited to the shoulders and arms, which does not align with a brainstem stroke.
Sensory pathways US Medical PG Question 8: A 23-year-old man presents to the emergency room following a stab wound to the back. He was in a bar when he got into an argument with another man who proceeded to stab him slightly right of the midline of his back. He is otherwise healthy and does not take any medications. He has one previous admission to the hospital for a stab wound to the leg from another bar fight 2 years ago. His temperature is 99°F (37.2°C), blood pressure is 115/80 mmHg, pulse is 100/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal exams are unremarkable; however, he has an abnormal neurologic exam. If this wound entered his spinal cord but did not cross the midline, which of the following would most likely be seen in this patient?
- A. Contralateral spasticity below the level of the lesion
- B. Ipsilateral flaccid paralysis at the level of the lesion (Correct Answer)
- C. Ipsilateral loss of pain and temperature sensation below the lesion
- D. Contralateral loss of tactile, vibration, and proprioception below the lesion
- E. Contralateral loss of sensation at the level of the lesion
Sensory pathways Explanation: ***Ipsilateral flaccid paralysis at the level of the lesion***
- A stab wound indicates an acute lesion, which often results in **spinal shock** at the level of the injury, leading to **flaccid paralysis** due to damage to the lower motor neurons or their axons.
- If the transection affects nerve roots or the ventral horn at the level of the lesion, it would specifically cause **ipsilateral flaccid paralysis** due to interruption of the efferent motor pathways before decussation.
*Contralateral spasticity below the level of the lesion*
- **Spasticity** (upper motor neuron signs) would occur **ipsilaterally** below the level of the lesion due to damage to the **corticospinal tracts** before their decussation in the medulla.
- This symptom takes time to develop following an acute injury, as the initial phase is often characterized by **spinal shock** and flaccid paralysis.
*Ipsilateral loss of pain and temperature sensation below the lesion*
- The **spinothalamic tracts**, responsible for pain and temperature sensation, **decussate (cross over)** almost immediately upon entering the spinal cord.
- Therefore, a lesion on one side of the spinal cord would cause **contralateral loss of pain and temperature** sensation below the level of the lesion.
*Contralateral loss of tactile, vibration, and proprioception below the lesion*
- The **dorsal columns**, which carry tactile, vibration, and proprioception information, **decussate in the medulla** oblongata, not in the spinal cord.
- Thus, a lesion on one side of the spinal cord would result in **ipsilateral loss of these sensations** below the level of the lesion.
*Contralateral loss of sensation at the level of the lesion*
- Sensation loss at the level of the lesion would involve the disruption of nerve roots or segmental grey matter, which primarily causes **ipsilateral sensory deficits** corresponding to the affected dermatome, not contralateral.
- Contralateral loss occurs for specific tracts (like spinothalamic) **below** the lesion, not typically at the level itself for all sensations.
Sensory pathways US Medical PG Question 9: A 39-year-old woman is brought to the emergency department following a stab wound to the neck. Per the patient, she was walking her dog when she got robbed and was subsequently stabbed with a knife. Vitals are stable. Strength examination reveals 2/5 right-sided elbow flexion and extension, wrist extension, and finger motions. Babinski sign is upward-going on the right. There is decreased sensation to light touch and vibration on the patient's right side up to her shoulder. She also reports decreased sensation to pinprick and temperature on her left side, including her lower extremities, posterior forearm, and middle finger. The patient's right pupil is 2 mm smaller than the left with drooping of the right upper eyelid. Which of the following is the most likely cause of the patient’s presentation?
- A. Hemisection injury (Correct Answer)
- B. Syringomyelia
- C. Anterior cord syndrome
- D. Posterior cord syndrome
- E. Central cord syndrome
Sensory pathways Explanation: ***Hemisection injury***
- The combination of **ipsilateral motor weakness** and **dorsal column deficits** (vibration, light touch) along with **contralateral loss of pain and temperature sensation** (spinothalamic tract) is the hallmark of a Brown-Séquard syndrome, which results from a hemisection injury to the spinal cord.
- The presence of **ipsilateral Horner's syndrome** (miosis and ptosis) indicates sympathetic nerve damage, further localizing the injury to the cervical spinal cord and supporting a hemisection.
*Syringomyelia*
- This condition is characterized by a **cavity (syrinx)** within the spinal cord, typically leading to a **cape-like distribution of pain and temperature loss** due to damage to the decussating spinothalamic fibers.
- It usually spares the dorsal columns and motor tracts in early stages, which contradicts the described ipsilateral motor and dorsal column deficits.
*Anterior cord syndrome*
- Results from damage to the **anterior spinal artery**, leading to **bilateral loss of motor function** (corticospinal tracts) and **pain/temperature sensation** (spinothalamic tracts) below the level of injury.
- **Proprioception and vibration sensation** (dorsal columns) are typically preserved in this syndrome, which is inconsistent with the patient's presentation.
*Posterior cord syndrome*
- Involves damage primarily to the **dorsal columns**, resulting in **loss of proprioception, vibration, and light touch** below the level of injury.
- **Motor function, pain, and temperature sensation** are generally preserved, which is not consistent with the motor deficits and contralateral pain/temperature loss described.
*Central cord syndrome*
- Most commonly seen after **hyperextension injuries**, leading to greater **motor weakness in the upper extremities** than the lower extremities.
- It typically causes varying degrees of **sensory loss** and can preserve sacral sensation, but the specific pattern of ipsilateral motor/dorsal column deficits and contralateral spinothalamic loss is not characteristic of central cord syndrome.
Sensory pathways US Medical PG Question 10: A 27-year-old woman comes to the clinic for blisters on both hands. The patient has a past medical history of asthma, eczema, and a car accident 2 years ago where she sustained a concussion. She also reports frequent transient episodes of blurred vision that clear with artificial tears. When asked about her blisters, the patient claims she was baking yesterday and forgot to take the pan out with oven gloves. Physical examination demonstrates weeping blisters bilaterally concentrated along the palmar surfaces of both hands and decreased pinprick sensation along the arms bilaterally. What is the most likely explanation of this patient’s symptoms?
- A. Brain contusion
- B. Syringomyelia at the lumbar region
- C. Syringomyelia at the cervico-thoracic region (Correct Answer)
- D. Multiple sclerosis
- E. Sjogren syndrome
Sensory pathways Explanation: ***Syringomyelia at the cervico-thoracic region***
- The presence of **painless burns/blisters** (due to **loss of pain and temperature sensation**) on the hands, coupled with **decreased pinprick sensation bilaterally along the arms**, strongly suggests involvement of the **cervical and thoracic spinal cord**, characteristic of syringomyelia.
- The history of a **concussion** from a car accident 2 years ago could be a predisposing factor leading to or exacerbating a Chiari malformation, which is often associated with syringomyelia.
*Brain contusion*
- A **brain contusion** would typically cause focal neurological deficits based on the affected brain region, but it would not explain the **bilateral loss of pain and temperature sensation** in the arms or palmar blistering.
- While a concussion history is provided, contusions do not usually present with the specific type of sensory deficit seen here.
*Syringomyelia at the lumbar region*
- **Syringomyelia at the lumbar region** would primarily cause symptoms in the **lower extremities**, such as leg weakness, pain, and sensory loss in the legs and feet.
- It would not explain the **bilateral decreased pinprick sensation along the arms** or the blisters on the hands.
*Multiple sclerosis*
- **Multiple sclerosis** often presents with fluctuating neurological symptoms, including **blurred vision**, but the characteristic **dissociated sensory loss** (loss of pain and temperature with preserved touch) and **painless burns** are not typical primary presentations.
- Sensory deficits in MS are usually more varied and can include numbness, tingling, or electric shock sensations rather than purely dissociated loss.
*Sjogren syndrome*
- **Sjögren's syndrome** is an autoimmune disorder primarily affecting exocrine glands, leading to **dry eyes** (which could cause blurred vision that improves with artificial tears) and dry mouth.
- It does not explain the **painless burns** or the bilateral **loss of pain and temperature sensation** in the upper extremities.
More Sensory pathways US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.