Motor pathways US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Motor pathways. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Motor pathways US Medical PG Question 1: An otherwise healthy 43-year-old woman comes to the physician because of several episodes of involuntary movements of her head over the past few months. They are sometimes associated with neck pain and last minutes to hours. Neurologic examination shows no abnormalities. During examination of the neck, the patient's head turns horizontally to the left. She states this movement is involuntary, and that she is unable to unturn her head. After 5 minutes, her head re-straightens. Which of the following best describes this patient's disorder?
- A. Dystonia (Correct Answer)
- B. Athetosis
- C. Akathisia
- D. Hemiballismus
- E. Chorea
Motor pathways Explanation: ***Dystonia***
- This patient presents with **sustained, involuntary muscle contractions** causing repetitive, twisting movements and abnormal postures [1], which are characteristic features of **dystonia**, specifically **cervical dystonia (torticollis)**.
- The description of the head turning involuntarily to the left and inability to unturn it, lasting minutes to hours, fits the pattern of intermittent or spasmodic dystonia.
*Athetosis*
- **Athetosis** involves slow, sinuous, **writhing involuntary movements**, particularly affecting distal limbs [1].
- These movements are often continuous and slow, unlike the more sudden, sustained contractions seen in the patient.
*Akathisia*
- **Akathisia** is characterized by an internal feeling of **restlessness** and a strong urge to move, often described as an inability to sit still.
- It results in fidgeting and pacing, rather than sustained, involuntary posturing of a specific body part.
*Hemiballismus*
- **Hemiballismus** involves **large-amplitude, involuntary, flinging movements** of one side of the body [1].
- This symptom typically arises from lesions in the **subthalamic nucleus** and is distinct from the sustained, twisting movements described [1].
*Chorea*
- **Chorea** presents as **brief, irregular, rapid, and unpredictable involuntary movements** that flow randomly from one body part to another [1].
- Unlike the sustained, fixed posturing seen in dystonia, choreiform movements are often described as "dance-like" and are not maintained.
Motor pathways US Medical PG Question 2: A 20-year-old man is brought to the emergency department 20 minutes after he sustained a stab wound to his back during an altercation. He reports weakness and numbness of the lower extremities. He has no history of serious illness. On arrival, he is alert and cooperative. His pulse is 90/min, and blood pressure is 100/65 mm Hg. Examination shows a deep 4-cm laceration on his back next to the vertebral column at the level of the T10 vertebra. Neurologic examination shows right-sided motor weakness with diminished vibratory sense ipsilaterally, decreased sensation to light touch at the level of his laceration and below, and left-sided loss of hot, cold, and pin-prick sensation at the level of the umbilicus and below. Deep tendon reflexes of his right lower extremity are 4+ and symmetrical. Babinski sign is absent bilaterally. The remainder of the examination shows no abnormalities. Which of the following is the most likely diagnosis?
- A. Brown-Sequard syndrome (Correct Answer)
- B. Anterior cord syndrome
- C. Posterior cord syndrome
- D. Cauda equina syndrome
- E. Central cord syndrome
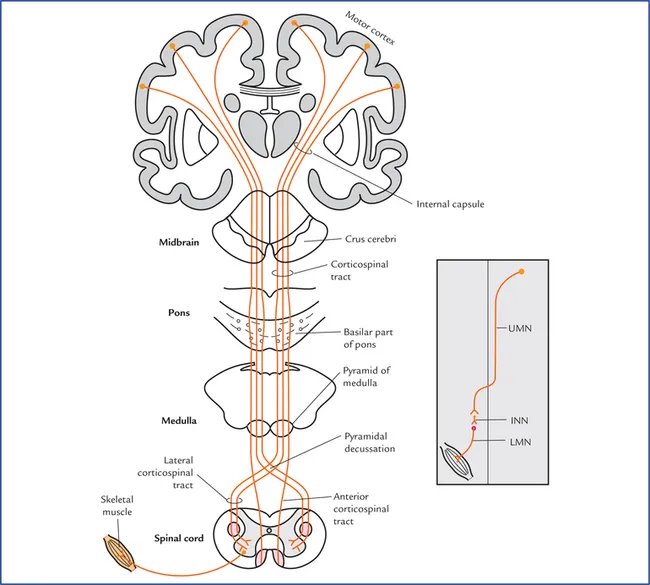
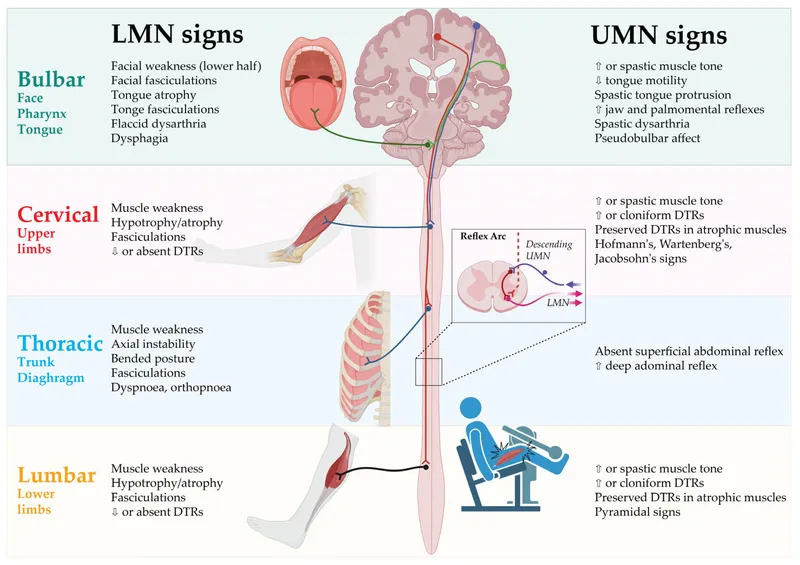
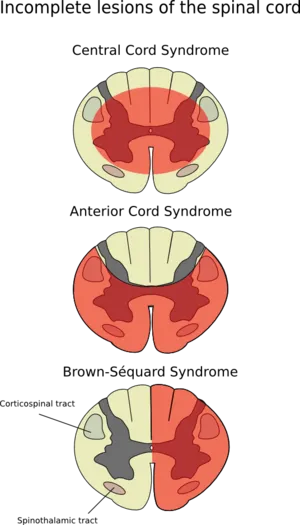
Motor pathways Explanation: ***Brown-Sequard syndrome***
- This syndrome is characterized by **ipsilateral motor paresis** and **loss of proprioception/vibration sensation**, along with **contralateral loss of pain and temperature sensation**.
- The patient's presentation of right-sided motor weakness and diminished vibratory sense ipsilaterally, coupled with left-sided loss of hot, cold, and pin-prick sensation, perfectly matches the classic signs of **Brown-Sequard syndrome** from a hemisection of the spinal cord (due to the stab wound).
*Anterior cord syndrome*
- This syndrome typically presents with **paraplegia or quadriplegia** and loss of pain and temperature sensation below the level of the lesion, with **preservation of proprioception and vibratory sensation**.
- The patient maintains **ipsilateral vibratory sensation** and has differential sensory loss, which is inconsistent with anterior cord syndrome where all distal sensation is broadly affected.
*Posterior cord syndrome*
- This syndrome is marked by a predominant loss of **proprioception and vibratory sensation** below the level of the lesion, with **preserved motor function** and pain/temperature sensation.
- The patient exhibits significant **motor weakness** and **contralateral loss of pain and temperature**, which are not typical features of posterior cord syndrome.
*Cauda equina syndrome*
- Cauda equina syndrome involves injury to the **nerve roots below the conus medullaris** and presents with **flaccid paralysis**, **saddle anesthesia**, and **bowel/bladder dysfunction**.
- The patient's presentation of spastic signs (4+ DTRs) and specific sensory deficits of a spinal cord lesion are inconsistent with the **lower motor neuron** signs of cauda equina syndrome.
*Central cord syndrome*
- This syndrome typically results in **greater motor impairment in the upper extremities than in the lower extremities**, along with a **variable sensory loss** below the level of the lesion, often involving a "cape-like" distribution of sensory loss.
- The patient's injury is at T10, and while there is motor weakness, the specific pattern of ipsilateral motor with contralateral pain/temperature loss is not characteristic of central cord syndrome, which usually affects the cervical region and has a different motor pattern.
Motor pathways US Medical PG Question 3: A 74-year-old man is brought to the physician by his wife for progressively worsening confusion and forgetfulness. Vital signs are within normal limits. Physical examination shows a flat affect and impaired short-term memory. An MRI of the brain is shown. Further evaluation of this patient is most likely to show which of the following findings?
- A. Postural instability
- B. Pill-rolling tremor
- C. Choreiform movements
- D. Broad-based gait (Correct Answer)
- E. Papilledema
Motor pathways Explanation: ***Broad-based gait***
- The patient's symptoms of **confusion**, **forgetfulness (dementia)**, and the MRI finding of **hydrocephalus** (dilated ventricles without sulcal effacement) are classic for **Normal Pressure Hydrocephalus (NPH)**.
- A hallmark triad of NPH includes **dementia**, **gait disturbance** (often described as broad-based or magnetic), and **urinary incontinence**.
*Postural instability*
- While patients with NPH can have **postural instability**, a more specific and prominent gait disturbance is typically observed.
- **Postural instability** is also a feature of many other neurological conditions, making it less specific than a broad-based gait for NPH.
*Pill-rolling tremor*
- A **pill-rolling tremor** is a characteristic feature of **Parkinson's disease**, which presents with a different constellation of symptoms, including bradykinesia and rigidity, and is not directly associated with hydrocephalus.
- This type of tremor is a **resting tremor** and is not typically seen in NPH.
*Choreiform movements*
- **Choreiform movements** are involuntary, brief, abrupt, and irregular movements, characteristic of conditions like **Huntington's disease**.
- These movements are not a typical manifestation of NPH, which primarily involves gait, cognition, and continence.
*Papilledema*
- **Papilledema** is swelling of the optic disc due to **increased intracranial pressure**.
- While hydrocephalus can cause increased intracranial pressure, NPH is characterized by **normal intracranial pressure**, hence papilledema is not expected.
Motor pathways US Medical PG Question 4: A patient with a known spinal cord ependymoma presents to his neurologist for a check up. He complains that he has had difficulty walking, which he attributes to left leg weakness. On exam, he is noted to have 1/5 strength in his left lower extremity, as well as decreased vibration and position sensation in the left lower extremity and decreased pain and temperature sensation in the right lower extremity. Which of the following spinal cord lesions is most consistent with his presentation?
- A. Anterior cord syndrome
- B. Posterior cord syndrome
- C. Syringomyelia
- D. Right-sided Brown-Sequard (hemisection)
- E. Left-sided Brown-Sequard (hemisection) (Correct Answer)
Motor pathways Explanation: ***Left-sided Brown-Sequard (hemisection)***
- This syndrome is characterized by **ipsilateral loss of motor function (weakness)** and **proprioception/vibration sensation** below the lesion, along with **contralateral loss of pain and temperature sensation**.
- The patient's left leg weakness, decreased vibration/position sensation in the left lower extremity, and decreased pain/temperature sensation in the right lower extremity perfectly match a **left-sided hemisection of the spinal cord**.
*Anterior cord syndrome*
- This syndrome results in **bilateral motor paralysis** and bilateral loss of **pain and temperature sensation** below the level of the lesion.
- However, **proprioception** and **vibration sense** are typically preserved, which contrasts with the patient's presentation of ipsilateral loss of these senses.
*Posterior cord syndrome*
- This rare syndrome primarily affects the **dorsal columns**, leading to bilateral loss of **vibration and proprioception** below the lesion.
- **Motor function** and **pain/temperature sensation** are largely preserved, which is inconsistent with the patient's significant motor weakness and contralateral pain/temperature loss.
*Syringomelia*
- This condition involves a fluid-filled cavity (syrinx) within the spinal cord, often causing a **cape-like distribution of pain and temperature loss** (crossing the midline) due to damage to the **decussating spinothalamic fibers**.
- While it can cause weakness, the distinct **ipsilateral proprioceptive loss** and **contralateral pain/temperature loss** seen in this patient are not typical for syringomyelia.
*Right-sided Brown-Sequard (hemisection)*
- A right-sided Brown-Sequard syndrome would present with **right-sided weakness** and **loss of proprioception/vibration sensation**, along with **left-sided loss of pain and temperature sensation**.
- This is the **opposite of the patient's presentation** of left-sided weakness and ipsilateral proprioceptive loss.
Motor pathways US Medical PG Question 5: A 55-year-old man is brought to the emergency department by his wife after falling down. About 90 minutes ago, they were standing in their kitchen making lunch and chatting when he suddenly complained that he could not see as well, felt weak, and was getting dizzy. He began to lean to 1 side, and he eventually fell to the ground. He did not hit his head. In the emergency department, he is swaying while seated, generally leaning to the right. The general physical exam is unremarkable. The neurologic exam is notable for horizontal nystagmus, 3/5 strength in the right arm, ataxia of the right arm, and absent pinprick sensation in the left arm and left leg. The computed tomography (CT) scan of the head is unremarkable. Which of the following is the most likely single location of this patient's central nervous system lesion?
- A. Primary motor cortex
- B. Thalamus
- C. Lateral medulla (Correct Answer)
- D. Primary somatosensory cortex
- E. Anterior spinal cord
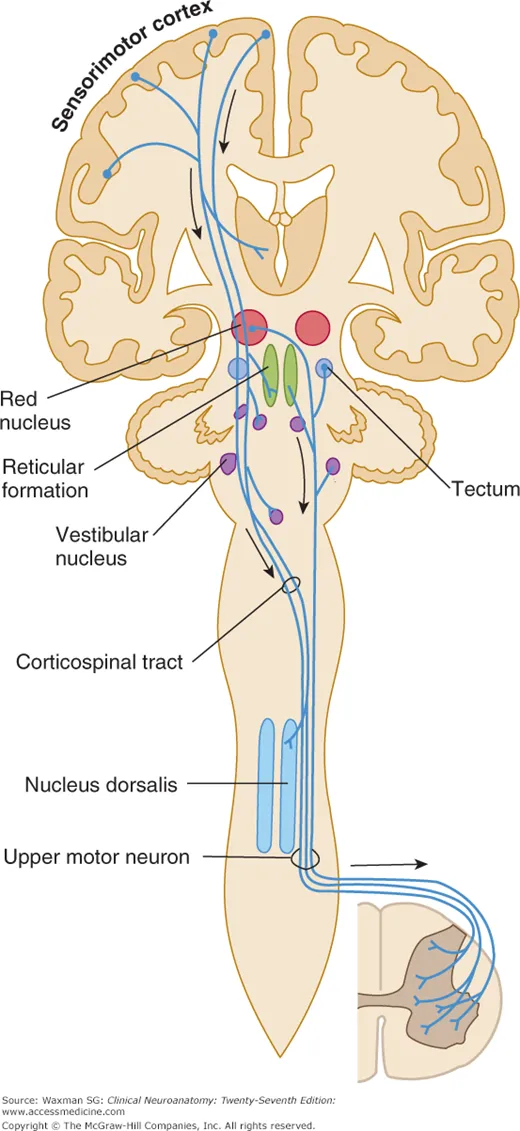
Motor pathways Explanation: ***Lateral medulla***
- The combination of **ipsilateral ataxia** and **weakness** (right arm) along with **contralateral pain and temperature sensory loss** (left arm and leg) is classic for a **lateral medullary syndrome (Wallenberg syndrome)**.
- **Horizontal nystagmus**, vertigo, and leaning to one side are also consistent with involvement of vestibular nuclei and cerebellar pathways in the lateral medulla.
*Primary motor cortex*
- A lesion here would cause **contralateral weakness or paralysis** but would not explain the ipsilateral ataxia, nystagmus, or contralateral pain and temperature loss.
- Sensory deficits would be minimal or absent, and would primarily affect discriminative touch.
*Thalamus*
- A thalamic lesion could cause **contralateral sensory loss** (affecting all modalities) and potentially some motor deficits or ataxia, but it typically does not cause **ipsilateral ataxia** or **nystagmus** in the pattern described.
- The specific combination of ipsilateral motor and contralateral sensory deficits points away from a pure thalamic lesion.
*Primary somatosensory cortex*
- A lesion in this area would primarily result in **contralateral deficits in discriminative touch, proprioception, and stereognosis**, not pain and temperature sensation.
- It would not explain the motor deficits, ataxia, or nystagmus seen in the patient.
*Anterior spinal cord*
- Damage to the anterior spinal cord (e.g., **anterior spinal artery syndrome**) would cause **bilateral motor weakness (paraplegia/quadriplegia)** and **bilateral loss of pain and temperature sensation** below the level of the lesion.
- It would not account for the nystagmus, vertigo, or the specific combination of ipsilateral and contralateral deficits observed in this patient, which are characteristic of brainstem involvement.
Motor pathways US Medical PG Question 6: A 47-year-old man comes to the emergency department because of urinary and fecal incontinence for 6 hours. Earlier in the day, he suffered a fall at a construction site and sustained injuries to his back and thighs but did not seek medical attention. He took ibuprofen for lower back pain. His temperature is 36.9°C (98.4°F), pulse is 80/min, and blood pressure is 132/84 mm Hg. Examination shows tenderness over the lumbar spine, bilateral lower extremity weakness, absent ankle jerk reflexes, and preserved patellar reflexes. There is decreased rectal tone. An ultrasound of the bladder shows a full bladder. Which of the following is the most likely diagnosis?
- A. Cerebellar stroke
- B. Spinal epidural abscess
- C. Anterior spinal cord syndrome
- D. Conus medullaris syndrome (Correct Answer)
- E. Brown-Sequard syndrome
Motor pathways Explanation: ***Conus medullaris syndrome***
- The combination of **bilateral lower extremity weakness**, **urinary and fecal incontinence**, **decreased rectal tone**, and a **full bladder** is characteristic of conus medullaris syndrome. This syndrome results from damage to the **conus medullaris** (the terminal part of the spinal cord), which typically involves the **S3-S5 nerve roots**.
- **Absent ankle jerk reflexes** (S1-S2) with **preserved patellar reflexes** (L2-L4) further pinpoints the lesion to the lower lumbar/sacral spinal cord segments, consistent with conus medullaris involvement. The recent **fall with back injury** is a predisposing factor.
*Cerebellar stroke*
- **Cerebellar stroke** would primarily manifest with symptoms of **ataxia**, **dysarthria**, **nystagmus**, and **vertigo**, without direct involvement of bladder/bowel function or specific lower extremity reflex abnormalities as described.
- While a stroke can cause weakness, it would typically be **unilateral** or involve specific cortical patterns, and not generally present with this constellation of lower spinal cord signs.
*Spinal epidural abscess*
- A **spinal epidural abscess** would typically present with **fever**, **severe localized back pain**, and progressive **neurological deficits**, often following an infection or recent spinal procedure.
- While it can cause neurological deficits similar to the conus medullaris syndrome, the absence of **fever** and the acute onset following trauma makes an abscess less likely in this scenario.
*Anterior spinal cord syndrome*
- **Anterior spinal cord syndrome** primarily affects the **anterior two-thirds of the spinal cord**, leading to **motor paralysis** below the lesion and **loss of pain and temperature sensation**, while **proprioception** and **vibration sense are preserved**.
- Although it can cause motor weakness and bladder dysfunction, the isolated loss of ankle jerk reflexes with preserved patellar reflexes and the specific pattern of incontinence are more indicative of conus medullaris involvement.
*Brown-Sequard syndrome*
- **Brown-Séquard syndrome** is characterized by **ipsilateral motor paralysis** and loss of **proprioception/vibration sensation**, along with **contralateral loss of pain and temperature sensation** below the level of the lesion, due to hemisection of the spinal cord.
- This patient presents with **bilateral weakness** and specific bladder/bowel dysfunction, which is inconsistent with the typical lateralized deficits seen in Brown-Séquard syndrome.
Motor pathways US Medical PG Question 7: A 5-year-old boy who recently emigrated from Nigeria is brought to the emergency department because of a 2-day history of lower leg weakness, swallowing difficulty, and drooling of saliva. He has not yet received any childhood vaccinations. Two days after admission, the patient develops shortness of breath. Pulse oximetry shows an oxygen saturation of 64%. Despite resuscitative efforts, the patient dies of respiratory failure. At autopsy, examination of the spinal cord shows destruction of the anterior horn cells. Neurological examination of this patient would have most likely shown which of the following findings?
- A. Sensory loss
- B. Positive Babinski sign
- C. Hyporeflexia (Correct Answer)
- D. Myoclonus
- E. Pronator drift
Motor pathways Explanation: ***Hyporeflexia***
- The destruction of **anterior horn cells** in the spinal cord is characteristic of **poliomyelitis**, a disease that primarily affects **lower motor neurons**.
- Lower motor neuron lesions lead to symptoms like **flaccid paralysis**, **weakness**, and **hyporeflexia** (diminished or absent reflexes).
*Sensory loss*
- Poliomyelitis specifically targets **motor neurons** and typically spares **sensory pathways**, meaning sensory function remains intact.
- Therefore, **sensory loss** is not a characteristic finding in poliomyelitis.
*Positive Babinski sign*
- A positive Babinski sign (**upgoing plantar reflex**) is indicative of an **upper motor neuron lesion** affecting the **corticospinal tract**.
- Since poliomyelitis involves lower motor neurons, a positive Babinski sign would not be expected.
*Myoclonus*
- **Myoclonus** refers to brief, involuntary twitching of a muscle or a group of muscles, often associated with disorders affecting the **cerebellum**, **brainstem**, or **cortex**.
- It is not a typical neurological finding in **poliomyelitis**, which primarily causes muscle weakness and paralysis.
*Pronator drift*
- **Pronator drift** is a sign of **upper motor neuron weakness** affecting the **contralateral corticospinal tract**, particularly in the arm.
- As **poliomyelitis** is a **lower motor neuron disease**, pronator drift would not be expected as a primary finding.
Motor pathways US Medical PG Question 8: A man appearing to be in his mid-50s is brought in by ambulance after he was seen walking on railroad tracks. On further questioning, the patient does not recall being on railroad tracks and is only able to provide his name. Later on, he states that he is a railroad worker, but this is known to be false. On exam, his temperature is 99.9°F (37.7°C), blood pressure is 128/86 mmHg, pulse is 82/min, and respirations are 14/min. He appears disheveled, and his clothes smell of alcohol. The patient is alert, is only oriented to person, and is found to have abnormal eye movements and imbalanced gait when attempting to walk. Which of the following structures in the brain likely has the greatest reduction in the number of neurons?
- A. Mammillary bodies (Correct Answer)
- B. Cerebellar vermis
- C. Parietal-temporal cortex
- D. Frontal eye fields
- E. Basal ganglia
Motor pathways Explanation: ***Mammillary bodies***
- This patient presents with symptoms highly suggestive of **Wernicke-Korsakoff syndrome**, which includes **ophthalmoplegia** (abnormal eye movements), **ataxia** (imbalanced gait), and **confabulation** (making up stories, like being a railroad worker) with **anterograde amnesia** (not recalling being on railroad tracks).
- Wernicke-Korsakoff syndrome is primarily caused by **thiamine (vitamin B1) deficiency**, commonly seen in **chronic alcoholics**, and results in neuronal loss and necrosis, especially in the **mammillary bodies** and dorsomedial nucleus of the thalamus.
*Cerebellar vermis*
- While **alcoholism** can lead to cerebellar damage, particularly the **vermis**, causing **ataxia**, it does not fully explain the **memory deficits, confabulation, and ophthalmoplegia** seen in Wernicke-Korsakoff syndrome.
- Damage to the cerebellar vermis would primarily result in truncal ataxia and gait instability without the prominent amnesia and confabulation.
*Parietal-temporal cortex*
- Damage to the **parietal-temporal cortex** is associated with various cognitive deficits, including **aphasias** and **agnosias**, depending on the specific areas affected.
- While it can be affected by chronic alcoholism, it is not the primary site of damage in **Wernicke-Korsakoff syndrome** and does not typically present with the classic triad.
*Frontal eye fields*
- The **frontal eye fields** are involved in controlling **voluntary eye movements** and saccades. Damage here can cause specific patterns of gaze palsies.
- However, the abnormal eye movements seen in Wernicke-Korsakoff syndrome (e.g., nystagmus, ophthalmoplegia) are typically due to damage in brainstem nuclei and **mammillary bodies**, not primarily the frontal eye fields.
*Basal ganglia*
- The **basal ganglia** are primarily involved in motor control, learning, and executive functions. Damage to these structures can lead to **movement disorders** like Parkinsonism or Huntington's disease.
- While chronic alcoholism can have diffuse effects on the brain, the basal ganglia are not the primary site of pathology in **Wernicke-Korsakoff syndrome**, and damage here would not explain the memory and confabulation symptoms.
Motor pathways US Medical PG Question 9: A 23-year-old man presents to the emergency room following a stab wound to the back. He was in a bar when he got into an argument with another man who proceeded to stab him slightly right of the midline of his back. He is otherwise healthy and does not take any medications. He has one previous admission to the hospital for a stab wound to the leg from another bar fight 2 years ago. His temperature is 99°F (37.2°C), blood pressure is 115/80 mmHg, pulse is 100/min, and pulse oximetry is 99% on room air. Cardiopulmonary and abdominal exams are unremarkable; however, he has an abnormal neurologic exam. If this wound entered his spinal cord but did not cross the midline, which of the following would most likely be seen in this patient?
- A. Contralateral spasticity below the level of the lesion
- B. Ipsilateral flaccid paralysis at the level of the lesion (Correct Answer)
- C. Ipsilateral loss of pain and temperature sensation below the lesion
- D. Contralateral loss of tactile, vibration, and proprioception below the lesion
- E. Contralateral loss of sensation at the level of the lesion
Motor pathways Explanation: ***Ipsilateral flaccid paralysis at the level of the lesion***
- A stab wound indicates an acute lesion, which often results in **spinal shock** at the level of the injury, leading to **flaccid paralysis** due to damage to the lower motor neurons or their axons.
- If the transection affects nerve roots or the ventral horn at the level of the lesion, it would specifically cause **ipsilateral flaccid paralysis** due to interruption of the efferent motor pathways before decussation.
*Contralateral spasticity below the level of the lesion*
- **Spasticity** (upper motor neuron signs) would occur **ipsilaterally** below the level of the lesion due to damage to the **corticospinal tracts** before their decussation in the medulla.
- This symptom takes time to develop following an acute injury, as the initial phase is often characterized by **spinal shock** and flaccid paralysis.
*Ipsilateral loss of pain and temperature sensation below the lesion*
- The **spinothalamic tracts**, responsible for pain and temperature sensation, **decussate (cross over)** almost immediately upon entering the spinal cord.
- Therefore, a lesion on one side of the spinal cord would cause **contralateral loss of pain and temperature** sensation below the level of the lesion.
*Contralateral loss of tactile, vibration, and proprioception below the lesion*
- The **dorsal columns**, which carry tactile, vibration, and proprioception information, **decussate in the medulla** oblongata, not in the spinal cord.
- Thus, a lesion on one side of the spinal cord would result in **ipsilateral loss of these sensations** below the level of the lesion.
*Contralateral loss of sensation at the level of the lesion*
- Sensation loss at the level of the lesion would involve the disruption of nerve roots or segmental grey matter, which primarily causes **ipsilateral sensory deficits** corresponding to the affected dermatome, not contralateral.
- Contralateral loss occurs for specific tracts (like spinothalamic) **below** the lesion, not typically at the level itself for all sensations.
Motor pathways US Medical PG Question 10: At what age does maximum brain growth occur?
- A. 6 months (Correct Answer)
- B. 1 year
- C. 2 years
- D. 3 years
- E. 5 years
Motor pathways Explanation: ***6 months***
- **Brain growth** is most rapid during the early postnatal period, with the brain reaching almost **50% of its adult size by 6 months of age**.
- This period involves rapid **synaptogenesis** and myelination, crucial for early cognitive and motor development.
*1 year*
- While significant **brain growth** continues, the peak rate of increase in brain volume has typically passed by 1 year.
- At this age, the brain has reached approximately **75% of its adult size**.
*2 years*
- By 2 years, the brain is about **80% of its adult size**, indicating ongoing but slower growth compared to the first year.
- This period is more characterized by refinement of neural circuits rather than rapid volumetric expansion.
*3 years*
- At 3 years, the brain has attained around **90% of its adult size**, though important developmental changes continue.
- The rate of **neural development** at this stage largely focuses on strengthening existing connections and pruning less used ones.
*5 years*
- By 5 years, the brain has reached approximately **90-95% of its adult size**, with growth significantly slower than in earlier years.
- Development at this age focuses primarily on **synaptic pruning** and refinement of neural networks rather than volumetric growth.
More Motor pathways US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.