Meninges and blood-brain barrier US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Meninges and blood-brain barrier. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Meninges and blood-brain barrier US Medical PG Question 1: A 60-year-old woman is brought to the emergency department by ambulance after suffering a generalized tonic-clonic seizure. The seizure lasted 2 minutes, followed by a short period of unresponsiveness and loud breathing. Her blood pressure is 130/80 mm Hg, the heart rate is 76/min, and the respiratory rate is 15/min and regular. On physical examination, the patient is confused but follows commands and cannot recall recent events. The patient does not present with any other neurological deficits. T1/T2 MRI of the brain demonstrates a hypointense, contrast-enhancing mass within the right frontal lobe, surrounded by significant cerebral edema. Which of the following would you expect in the tissue surrounding the described lesion?
- A. Loss of endothelial tight junctions (Correct Answer)
- B. Replacement of interstitial fluid with cerebrospinal fluid (CSF)
- C. Increased intracellular concentrations of osmolytes
- D. Upregulation of aquaporin-4
- E. Increased interstitial fluid low in protein
Meninges and blood-brain barrier Explanation: ***Loss of endothelial tight junctions***
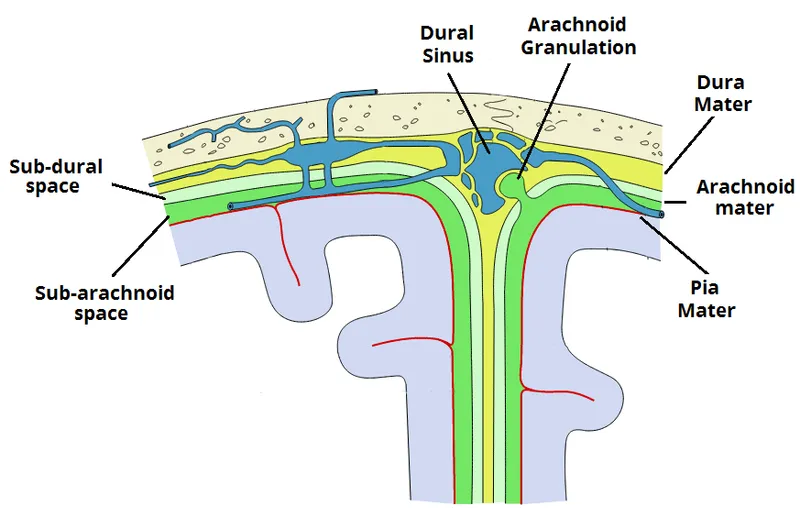
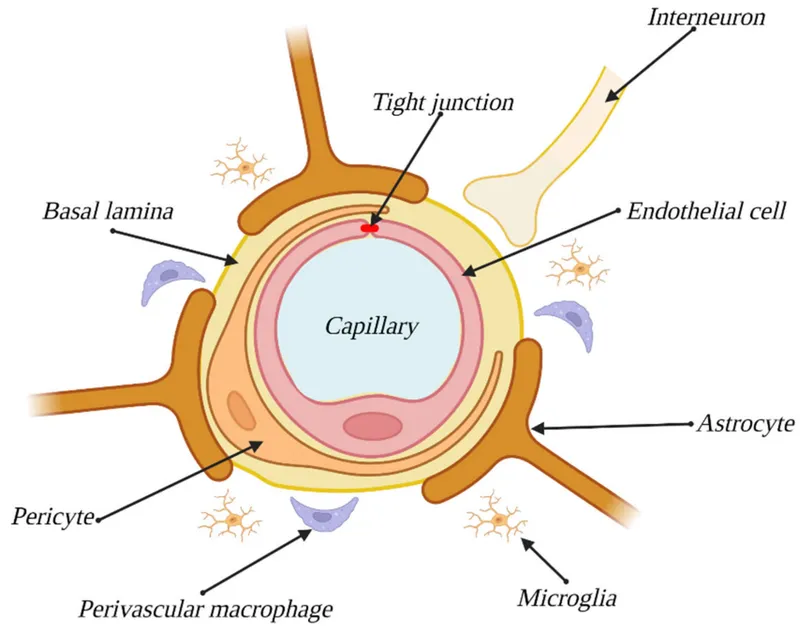
- The presence of a **contrast-enhancing mass** with surrounding edema suggests **vasogenic edema**, which is caused by the disruption of the **blood-brain barrier (BBB)**.
- This disruption primarily involves the **loss of tight junctions** between endothelial cells, allowing plasma proteins and fluid to leak into the interstitial space.
*Replacement of interstitial fluid with cerebrospinal fluid (CSF)*
- **CSF** is produced by the choroid plexus and flows through the ventricular system and subarachnoid space; it does not replace interstitial fluid within the brain parenchyma.
- While disruptions can occur, the primary mechanism of edema in this context is leakage from blood vessels, not direct replacement by CSF.
*Increased intracellular concentrations of osmolytes*
- This describes the mechanism of **cytotoxic edema**, where intracellular swelling occurs due to **cellular dysfunction** (e.g., ischemia) and the accumulation of osmolytes within cells.
- However, the patient's MRI findings of a **contrast-enhancing mass** and significant surrounding edema are more consistent with **vasogenic edema**, which is extracellular.
*Upregulation of aquaporin-4*
- **Aquaporin-4** channels are involved in water transport and are primarily associated with the development of **cytotoxic edema** or hydrocephalic edema by facilitating water movement across cell membranes.
- In **vasogenic edema**, the primary issue is the **breakdown of the BBB** and leakage of fluid and proteins, rather than altered aquaporin expression as the initial cause.
*Increased interstitial fluid low in protein*
- While there is **increased interstitial fluid**, the fluid in **vasogenic edema** is typically **rich in protein** (plasma proteins) because the **blood-brain barrier** is compromised.
- Fluid that is **low in protein** is characteristic of **hydrocephalic edema**, where CSF transudates into the periventricular white matter due to increased ventricular pressure.
Meninges and blood-brain barrier US Medical PG Question 2: A 48-year-old man presents to the ER with a sudden-onset, severe headache. He is vomiting and appears confused. His wife, who accompanied him, says that he has not had any trauma, and that the patient has no relevant family history. He undergoes a non-contrast head CT that shows blood between the arachnoid and pia mater. What is the most likely complication from this condition?
- A. Hemorrhagic shock
- B. Arterial Vasospasm (Correct Answer)
- C. Renal failure
- D. Bacterial Meningitis
- E. Blindness
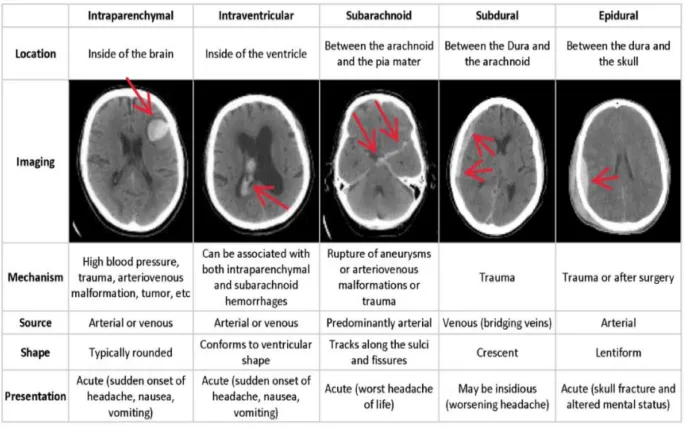
Meninges and blood-brain barrier Explanation: **Arterial Vasospasm**
- **Arterial vasospasm** is a major delayed complication of **subarachnoid hemorrhage (SAH)**, typically occurring 3-14 days after the initial bleed.
- The presence of blood products in the subarachnoid space can irritate cerebral arteries, leading to their narrowing and subsequent **delayed cerebral ischemia** or infarction.
*Hemorrhagic shock*
- **Subarachnoid hemorrhage (SAH)** typically involves bleeding within the confines of the skull, which is usually not extensive enough to cause systemic **hypovolemia** or **hemorrhagic shock**.
- **Hemorrhagic shock** would require significant external blood loss or internal bleeding into a large body cavity, which is not characteristic of an isolated SAH.
*Renal failure*
- **Renal failure** is not a direct or common complication of **subarachnoid hemorrhage (SAH)**.
- While systemic complications can sometimes arise in critically ill patients, there is no direct pathophysiological link between SAH and primary kidney injury.
*Bacterial Meningitis*
- The presence of blood in the **subarachnoid space** can cause a **chemical meningitis** due to irritation, mimicking some symptoms of bacterial meningitis.
- However, it does not typically predispose to **bacterial infection** unless there's an iatrogenic cause (e.g., lumbar puncture contamination).
*Blindness*
- While damage to the **optic nerves** or visual pathways can occur with severe neurological events or increased intracranial pressure, **blindness** is not a common or direct complication specifically arising from the bleed itself or its immediate sequelae in SAH.
- Visual disturbances are possible due to elevated **intracranial pressure** or specific anatomical lesion, but not primary blindness.
Meninges and blood-brain barrier US Medical PG Question 3: A 65-year-old male prisoner goes on a hunger strike to protest the conditions of his detainment. After 5 days without food, he suffers a seizure for which he is taken into a medical facility. On physical examination, he looks pale and diaphoretic. His blood glucose level is 50 mg/dL. In order to keep a constant supply of energy to his brain, which of the following molecules is his liver releasing into the bloodstream?
- A. Glycogen
- B. Glucose-6-phosphate
- C. ß-hydroxybutyric acid (Correct Answer)
- D. Fatty acids
- E. Glucose-1-phosphate
Meninges and blood-brain barrier Explanation: ***ß-hydroxybutyric acid***
- After 5 days of a hunger strike, **glycogen stores** are depleted, forcing the body to rely on **fatty acid oxidation** and **ketone body production** in the liver as an alternative fuel source for the brain.
- **ß-hydroxybutyrate** is one of the primary ketone bodies released by the liver into the bloodstream to provide energy, especially for the brain, during prolonged fasting.
*Glycogen*
- **Glycogenolysis** (breakdown of glycogen) is a short-term response to low blood glucose and supplies glucose for only about 24-36 hours of fasting. After 5 days, **hepatic glycogen stores** would be largely depleted.
- The liver releases **free glucose** into the bloodstream, not intact glycogen, from glycogen breakdown.
*Glucose-6-phosphate*
- **Glucose-6-phosphate** is an intermediate in glycolysis and gluconeogenesis, but it is not directly released into the bloodstream by the liver.
- It must be converted to **free glucose** by glucose-6-phosphatase before it can exit the hepatocyte and enter circulation.
*Fatty acids*
- The liver takes up **fatty acids** from adipose tissue breakdown during prolonged fasting to convert them into **ketone bodies**.
- While fatty acids are a major energy source for other tissues, the **brain cannot directly utilize fatty acids** for energy due to the inability of long-chain fatty acids to cross the blood-brain barrier.
*Glucose-1-phosphate*
- **Glucose-1-phosphate** is an intermediate formed during the breakdown of glycogen (glycogenolysis).
- Like glucose-6-phosphate, it is not directly released into the bloodstream but is further metabolized within the hepatocyte, eventually leading to the release of **free glucose**.
Meninges and blood-brain barrier US Medical PG Question 4: Which change in CSF production most directly affects intracranial pressure?
- A. Decreased arachnoid granulation function
- B. Increased choroid plexus blood flow
- C. Decreased carbonic anhydrase activity (Correct Answer)
- D. Increased osmotic gradient
Meninges and blood-brain barrier Explanation: ***Decreased carbonic anhydrase activity***
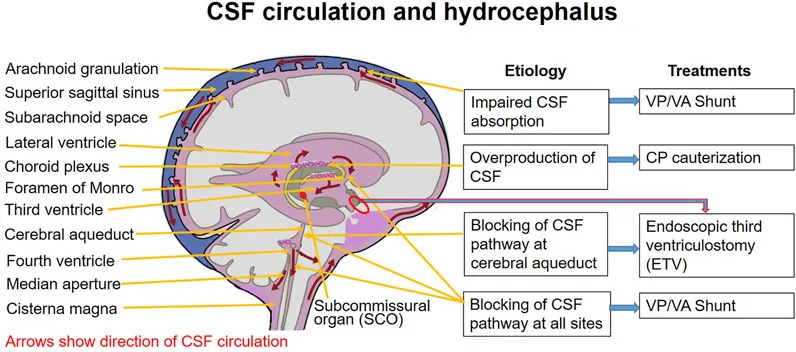
- The **choroid plexus** produces CSF primarily through an active secretion process involving carbonic anhydrase.
- Decreased activity of this enzyme directly reduces the formation of **bicarbonate ions** and **protons (H+)**, which are crucial for the active transport of Na+ and Cl- into the CSF, thereby lowering CSF production and subsequently **intracranial pressure**.
*Decreased arachnoid granulation function*
- This change would lead to a **decreased reabsorption** of CSF, which would *increase* intracranial pressure, not directly affect production to lower it.
- Arachnoid granulations are responsible for the **resorption of CSF** into the venous system.
*Increased choroid plexus blood flow*
- While increased blood flow could potentially increase the delivery of substrates for CSF production, it is **not the most direct or primary determinant** of CSF production rate.
- CSF production is predominantly an **active secretory process**, not a passive filtration process dependent solely on blood flow.
*Increased osmotic gradient*
- An increased osmotic gradient, if referring to a higher osmolality in the CSF compared to plasma, would tend to **draw water into the CSF**, potentially *increasing* CSF volume and intracranial pressure.
- If referring to a gradient drawing water *out* of the CSF, it would *decrease* intracranial pressure but is not a primary mechanism of CSF production regulation.
Meninges and blood-brain barrier US Medical PG Question 5: A 56-year-old woman presents with sudden-onset severe headache, nausea, vomiting, and neck pain for the past 90 minutes. She describes her headache as a ‘thunderclap’, followed quickly by severe neck pain and stiffness, nausea and vomiting. She denies any loss of consciousness, seizure, or similar symptoms in the past. Her past medical history is significant for an episode 6 months ago where she suddenly had trouble putting weight on her right leg, which resolved within hours. The patient denies any history of smoking, alcohol or recreational drug use. On physical examination, the patient has significant nuchal rigidity. Her muscle strength in the lower extremities is 4/5 on the right and 5/5 on the left. The remainder of the physical examination is unremarkable. A noncontrast CT scan of the head is normal. Which of the following is the next best step in the management of this patient?
- A. Diffusion-weighted magnetic resonance imaging of the brain
- B. IV tPA
- C. Placement of a ventriculoperitoneal (VP) shunt
- D. T1/T2 MRI of the head
- E. Lumbar puncture (Correct Answer)
Meninges and blood-brain barrier Explanation: ***Lumbar puncture***
- A **thunderclap headache**, nuchal rigidity, nausea, and vomiting despite a normal noncontrast CT scan, is highly suspicious for **subarachnoid hemorrhage (SAH)**. A lumbar puncture is the next diagnostic step to look for **xanthochromia** or **red blood cells** in the cerebrospinal fluid.
- The previous episode of transient leg weakness could indicate a prior **warning leak** from an **aneurysm**, increasing the suspicion for SAH.
*Diffusion-weighted magnetic resonance imaging of the brain*
- This imaging is primarily used to detect **acute ischemic stroke**, which presents differently.
- While helpful for ischemic events, it is **not the primary diagnostic test** for suspected SAH after a normal CT.
*IV tPA*
- **Intravenous tissue plasminogen activator (IV tPA)** is a thrombolytic used in acute ischemic stroke, characterized by focal neurological deficits.
- It is **contraindicated** in SAH due to the significant risk of exacerbating intracranial bleeding.
*Placement of a ventriculoperitoneal (VP) shunt*
- A **VP shunt** is a surgical procedure to drain excess cerebrospinal fluid, typically used to treat **hydrocephalus**.
- This is a treatment for a complication (hydrocephalus) that may arise from SAH, but it is **not the initial diagnostic or management step** for an acute SAH.
*T1/T2 MRI of the head*
- While MRI can detect SAH, especially if performed with specific sequences (FLAIR), a **lumbar puncture is more sensitive for detecting SAH** when a CT scan is negative and clinical suspicion remains high.
- MRI is generally less accessible and more time-consuming than lumbar puncture in an emergency setting for suspected SAH.
Meninges and blood-brain barrier US Medical PG Question 6: A 24-year-old man is brought to the emergency department after he is found sluggish, drowsy, feverish, and complaining about a headache. His past medical history is unremarkable. His vital signs include: blood pressure 120/60 mm Hg, heart rate 70/min, respiratory rate 17/min, and body temperature 39.0°C (102.2°F). On physical examination, the patient is dysphasic and incapable of following commands. Gait ataxia is present. No meningeal signs or photophobia are present. A noncontrast CT of the head is unremarkable. A T2 MRI is performed and is shown in the image. A lumbar puncture (LP) is subsequently performed. Which of the following CSF findings would you most likely expect to find in this patient?
- A. Opening pressure: 28 cm H2O, color: cloudy, protein: 68 mg/dL, cell count: 150 cells/µL, mostly PMNs, ratio CSF:blood glucose: 0.3
- B. Opening pressure: 38 cm H2O, color: cloudy, protein: 75 mg/dL, cell count: 80 cells/µL, mostly lymphocytes, ratio CSF:blood glucose: 0.25
- C. Opening pressure: 15 cm H2O, color: clear, protein: 50 mg/dL, cell count: 40 cells/µL, mostly lymphocytes, ratio CSF:blood glucose: 0.65 (Correct Answer)
- D. Opening pressure: 18 cm H2O, color: clear, protein: 40 mg/dL, cell count: 2 cells/µL, mostly polymorphonuclear (PMNs), ratio CSF:blood glucose: 0.7
- E. Opening pressure: 40 cm H2O, color: cloudy, protein: 80 mg/dL, cell count: 135 cells/µL, mostly lymphocytes with some PMNs, ratio CSF:blood glucose: 0.2
Meninges and blood-brain barrier Explanation: ***Opening pressure: 15 cm H2O, color: clear, protein: 50 mg/dL, cell count: 40 cells/µL, mostly lymphocytes, ratio CSF:blood glucose: 0.65***
- The MRI shows **hyperintensity in the right temporal lobe**, consistent with **herpes simplex encephalitis (HSE)**, which often presents with viral encephalitis CSF findings: mildly elevated protein, normal glucose, and lymphocytosis.
- The clinical presentation of fever, headache, altered mental status (sluggish, drowsy, dysphasic), and focal neurological deficits (gait ataxia) without meningeal signs also points towards viral encephalitis.
*Opening pressure: 28 cm H2O, color: cloudy, protein: 68 mg/dL, cell count: 150 cells/µL, mostly PMNs, ratio CSF:blood glucose: 0.3*
- This CSF profile (elevated opening pressure, cloudy appearance, high protein, low glucose, and **predominance of PMNs**) is characteristic of **bacterial meningitis**.
- While the patient has fever and altered mental status, the MRI strongly suggests encephalitis rather than meningitis, and the clinical picture does not fully align with bacterial meningitis (e.g., absence of meningeal signs).
*Opening pressure: 38 cm H2O, color: cloudy, protein: 75 mg/dL, cell count: 80 cells/µL, mostly lymphocytes, ratio CSF:blood glucose: 0.25*
- This CSF profile (very high opening pressure, cloudy, high protein, and very **low glucose**) is most consistent with **fungal or tuberculous meningitis**.
- Although there is lymphocytosis, the markedly low glucose suggests a different etiology than typical viral encephalitis like HSE, and the opening pressure is excessively high for standard viral encephalitis.
*Opening pressure: 18 cm H2O, color: clear, protein: 40 mg/dL, cell count: 2 cells/µL, mostly polymorphonuclear (PMNs), ratio CSF:blood glucose: 0.7*
- This CSF profile represents essentially **normal findings** (normal opening pressure, clear, normal protein, very low cell count, normal glucose ratio).
- Given the patient's significant symptoms (fever, dysphasia, gait ataxia) and the clear abnormalities on MRI, normal CSF findings are highly unlikely in this case, as it would suggest a non-inflammatory process.
*Opening pressure: 40 cm H2O, color: cloudy, protein: 80 mg/dL, cell count: 135 cells/µL, mostly lymphocytes with some PMNs, ratio CSF:blood glucose: 0.2*
- This profile (extremely high opening pressure, cloudy, high protein, high cell count with **mixed pleocytosis but predominantly lymphocytes**, and very **low glucose**) points towards a severe inflammatory process such as **tuberculous meningitis** or certain severe fungal infections.
- While viral encephalitis can have an elevated lymphocyte count and protein, the very high opening pressure and markedly low glucose are not typical for HSE.
Meninges and blood-brain barrier US Medical PG Question 7: A 68-year-old man is brought to the emergency department by his wife because of a 2-week history of progressive disorientation and a 1-day history of left-sided weakness and difficulty speaking. The wife reports that the patient had a minor fall 4 months ago, during which he may have hit his head. He has hypertension and hyperlipidemia. He drinks 3–4 bottles of beer daily. He is only oriented to person. Neurological examination shows moderate spastic weakness, decreased sensation, and increased deep tendon reflexes in the left upper and lower extremities. A CT scan of the head is shown. Which of the following is the most likely cause of this patient's condition?
- A. Tearing of bridging veins (Correct Answer)
- B. Embolus to middle cerebral artery
- C. Injury to middle meningeal artery
- D. Bleeding from intraventricular vascular malformation
- E. Damage to lenticulostriate arteries
Meninges and blood-brain barrier Explanation: ***Tearing of bridging veins***
- The patient's presentation with progressive disorientation, left-sided weakness, and difficulty speaking, occurring months after a minor head trauma, is highly suggestive of a **chronic subdural hematoma**. This typically results from the tearing of **bridging veins** traversing the subdural space.
- Risk factors like **advanced age** (brain atrophy stretches bridging veins), **alcoholism** (which leads to brain atrophy and increased fall risk), and his symptoms progressing over weeks further support this diagnosis.
*Embolus to middle cerebral artery*
- An **embolic stroke** typically presents with a **sudden onset** of neurological deficits, not a progressive deterioration over weeks as seen in this patient.
- While an MCA stroke could cause left-sided weakness and aphasia, the **history of head trauma** and delayed, progressive symptoms are not characteristic.
*Injury to middle meningeal artery*
- Injury to the middle meningeal artery usually leads to an **epidural hematoma**, which presents acutely with a **lucid interval** followed by rapid neurological decline.
- The CT scan of an epidural hematoma shows a **biconvex (lenticular) shape**, whereas a subdural hematoma has a crescent shape.
*Bleeding from intraventricular vascular malformation*
- Intraventricular bleeding from a vascular malformation typically causes **acute hydrocephalus**, severe headache, and rapid neurological deterioration with signs of increased intracranial pressure.
- This scenario does not fit the several-week progressive course or the delayed presentation after trauma.
*Damage to lenticulostriate arteries*
- Damage to the lenticulostriate arteries (often due to hypertension) is a common cause of **lacunar strokes**, which can lead to pure motor or pure sensory deficits.
- While the patient has hypertension, the clinical presentation of progressive symptoms over weeks following head trauma is not typical for a lacunar stroke.
Meninges and blood-brain barrier US Medical PG Question 8: Where does the only cranial nerve without a thalamic relay nucleus enter the skull?
- A. Superior orbital fissure
- B. Internal auditory meatus
- C. Foramen rotundum
- D. Jugular foramen
- E. Cribriform plate (Correct Answer)
Meninges and blood-brain barrier Explanation: ***Cribriform plate***
- The **olfactory nerve (CN I)** is the only cranial nerve that does not have a thalamic relay nucleus before reaching the cerebral cortex.
- It passes through the **cribriform plate** of the ethmoid bone to reach the olfactory bulbs.
*Superior orbital fissure*
- This opening transmits the **oculomotor (CN III), trochlear (CN IV), ophthalmic division of trigeminal (CN V1)**, and **abducens (CN VI)** nerves.
- These nerves all have sensory or motor components that relay through the thalamus, directly or indirectly.
*Internal auditory meatus*
- This canal transmits the **facial (CN VII)** and **vestibulocochlear (CN VIII)** nerves.
- The vestibulocochlear nerve's auditory pathway involves a thalamic relay in the **medial geniculate nucleus**.
*Foramen rotundum*
- The **maxillary division of the trigeminal nerve (CN V2)** passes through the foramen rotundum.
- Sensory information carried by CN V2 relays through the **thalamus**.
*Jugular foramen*
- This opening transmits the **glossopharyngeal (CN IX), vagus (CN X)**, and **accessory (CN XI)** nerves.
- Sensory components of these nerves, particularly taste and visceral sensation, involve thalamic nuclei.
Meninges and blood-brain barrier US Medical PG Question 9: A 53-year-old man is brought to the emergency department for confusion. He was in his usual state of health until about 3 hours ago when he tried to use his sandwich to turn off the TV. He also complained to his wife that he had a severe headache. Past medical history is notable for hypertension, which has been difficult to control on multiple medications. His temperature is 36.7°C (98°F), the pulse is 70/min, and the blood pressure is 206/132 mm Hg. On physical exam he is alert and oriented only to himself, repeating over and over that his head hurts. The physical exam is otherwise unremarkable and his neurologic exam is nonfocal. The noncontrast CT scan of the patient's head is shown and reveals an acute intraparenchymal hemorrhage in the basal ganglia. Which of the following diagnostic tests would be most helpful in determining the underlying cause of this patient's hemorrhage?
- A. Lumbar puncture
- B. Electroencephalogram (EEG)
- C. MRI of the brain
- D. CT angiography of the neck
- E. CT angiography of the brain (Correct Answer)
Meninges and blood-brain barrier Explanation: ***CT angiography of the brain***
- Following identification of an **intracerebral hemorrhage** on noncontrast CT, **CT angiography (CTA) of the brain** is the most appropriate next diagnostic test to identify underlying vascular abnormalities such as **arteriovenous malformations (AVMs)**, **aneurysms**, **dural arteriovenous fistulas**, or **moyamoya disease**.
- While this patient has severe hypertension (a common cause of basal ganglia hemorrhage), CTA should still be performed to rule out secondary causes, particularly in patients under 70 years old or those with atypical features.
- CTA can be performed rapidly in the acute setting and has high sensitivity for detecting vascular lesions that may require specific treatment.
*MRI of the brain*
- MRI with specialized sequences (GRE, SWI, FLAIR) can provide detailed information about **chronic microhemorrhages**, **cerebral amyloid angiopathy**, **underlying tumors**, or **cavernomas**.
- However, MRI is typically performed **after CTA** in the workup of intracerebral hemorrhage, not as the immediate next step.
- MRI is less readily available in the acute setting and takes longer to perform than CTA.
*CT angiography of the neck*
- This test visualizes the **carotid and vertebral arteries** in the neck to detect **stenosis**, **dissection**, or **atherosclerotic disease**.
- It is not directly useful for identifying the cause of an **intraparenchymal hemorrhage** within the brain substance itself.
*Lumbar puncture*
- Lumbar puncture analyzes **cerebrospinal fluid (CSF)** and is primarily used for suspected **subarachnoid hemorrhage** (when CT is negative), **meningitis**, or **encephalitis**.
- It is **contraindicated** in patients with significant intraparenchymal hemorrhage due to risk of herniation from increased intracranial pressure.
*Electroencephalogram (EEG)*
- EEG measures **electrical activity in the brain** and is used to diagnose **seizure disorders** or evaluate altered mental status from metabolic or epileptic causes.
- While confusion can result from seizures, the primary pathology is the **intracerebral hemorrhage** identified on CT, which EEG cannot diagnose or characterize.
Meninges and blood-brain barrier US Medical PG Question 10: A 56-year-old man presents to the family medicine office since he has been having difficulty keeping his blood pressure under control for the past month. He has a significant medical history of hypertension, coronary artery disease, and diabetes mellitus. He has a prescription for losartan, atenolol, and metformin. The blood pressure is 178/100 mm Hg, the heart rate is 92/min, and the respiratory rate is 16/min. The physical examination is positive for a grade II holosystolic murmur at the left sternal border. He also has diminished sensation in his toes. Which of the following statements is the most effective means of communication between the doctor and the patient?
- A. “What is causing your blood pressure to be elevated?” (Correct Answer)
- B. “Have you been taking your medications as prescribed?”
- C. “Would you like us to consider trying a different medication for your blood pressure?”
- D. “You are taking your medications as prescribed, aren’t you?”
- E. “Why are you not taking your medication?”
Meninges and blood-brain barrier Explanation: ***“What is causing your blood pressure to be elevated?”***
- This is an **open-ended question** that encourages the patient to share their perspective, concerns, and potential reasons for the elevated blood pressure, fostering a **patient-centered approach**.
- It allows the physician to understand the patient's individual circumstances, medication adherence, lifestyle factors, or other contributing issues without being judgmental or leading.
*“Have you been taking your medications as prescribed?”*
- This is a **closed-ended question** that primarily elicits a "yes" or "no" answer, providing limited insight into the patient's actual adherence and the underlying reasons for non-adherence.
- While important, phrasing it this way might make the patient feel interrogated or judged, potentially hindering honest communication.
*“Would you like us to consider trying a different medication for your blood pressure?”*
- This question prematurely jumps to a solution without fully understanding the cause of the elevated blood pressure and the patient's perspective.
- It bypasses the crucial step of investigating potential reasons for poor blood pressure control, which could include non-adherence, lifestyle factors, or secondary hypertension, rather than necessarily a medication efficacy issue.
*“You are taking your medications as prescribed, aren’t you?”*
- This is a **leading question** that implies an expectation and can make the patient feel pressured to answer affirmatively, even if they are not consistently taking their medication.
- Such phrasing can create a defensive environment and discourage the patient from openly discussing adherence challenges.
*“Why are you not taking your medication?”*
- This is a **direct and accusatory question** that implies blame and can immediately put the patient on the defensive, making them less likely to be honest or forthcoming about their medication habits.
- It fails to create a supportive or collaborative atmosphere, which is essential for effective patient-physician communication.
More Meninges and blood-brain barrier US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.