Functional neuroanatomy of vision US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Functional neuroanatomy of vision. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Functional neuroanatomy of vision US Medical PG Question 1: You are seeing a patient in clinic who presents with complaints of weakness. Her physical exam is notable for right sided hyperreflexia, as well as the reflex finding shown in the image below. Where is the most likely location of this patient's lesion?
- A. Postcentral gyrus
- B. Neuromuscular junction
- C. Lateral geniculate nucleus
- D. Internal capsule (Correct Answer)
- E. Subthalamic nucleus
Functional neuroanatomy of vision Explanation: ***Internal capsule***
- The combination of **right-sided hyperreflexia** (an upper motor neuron sign) and a positive **Babinski sign** (as implied by a video demonstrating this reflex) points to an upper motor neuron lesion.
- The **internal capsule** contains descending motor pathways, and a lesion here would affect the contralateral side of the body, causing **weakness** and upper motor neuron signs.
*Postcentral gyrus*
- The **postcentral gyrus** is the primary somatosensory cortex and primarily deals with sensory processing, not motor output.
- A lesion here would typically cause **contralateral sensory deficits**, such as numbness or loss of proprioception, rather than motor weakness with hyperreflexia.
*Neuromuscular junction*
- Diseases of the **neuromuscular junction**, such as myasthenia gravis, cause **fatigable weakness** without hyperreflexia or other upper motor neuron signs.
- Reflexes are typically normal or decreased in these conditions.
*Lateral geniculate nucleus*
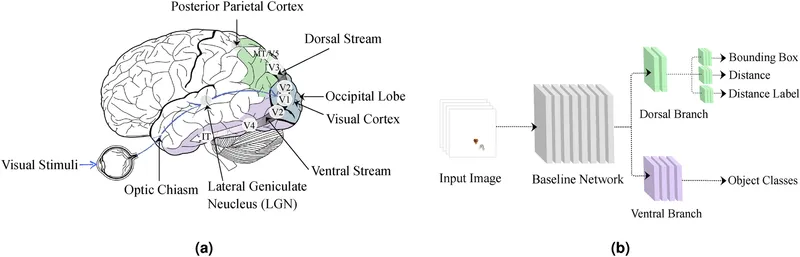
- The **lateral geniculate nucleus** is a thalamic relay center for visual information.
- Lesions here would result in **visual field deficits** (e.g., homonymous hemianopsia), not motor weakness or hyperreflexia.
*Subthalamic nucleus*
- The **subthalamic nucleus** is part of the basal ganglia and is involved in motor control, particularly in regulating movement initiation and stopping.
- Lesions here are classically associated with **hemiballismus**, which is characterized by wild, flinging movements, rather than weakness and hyperreflexia.
Functional neuroanatomy of vision US Medical PG Question 2: A 58-year-old woman presents with vision loss in her right eye. She noticed the visual changes the morning of presentation and has never experienced this visual disturbance before. Her medical history is significant for hypertension, hypercholesterolemia, and type II diabetes mellitus. She is currently on lisinopril, lovastatin, and metformin. She has smoked a pack of cigarettes daily for the last 25 years and also is a social drinker. On physical exam, her lids and lashes appear normal and there is no conjunctival injection. Both pupils are equal, round, and reactive to light; however, when the penlight is swung from the left eye to the right eye, there is bilateral pupillary dilation. The nerve that is most likely defective in this patient relays information to which of the following?
- A. Oculomotor nucleus
- B. Edinger-Westphal nucleus
- C. Medial geniculate nucleus
- D. Lateral geniculate nucleus (Correct Answer)
- E. Ventral posteromedial nucleus
Functional neuroanatomy of vision Explanation: ***Lateral geniculate nucleus***
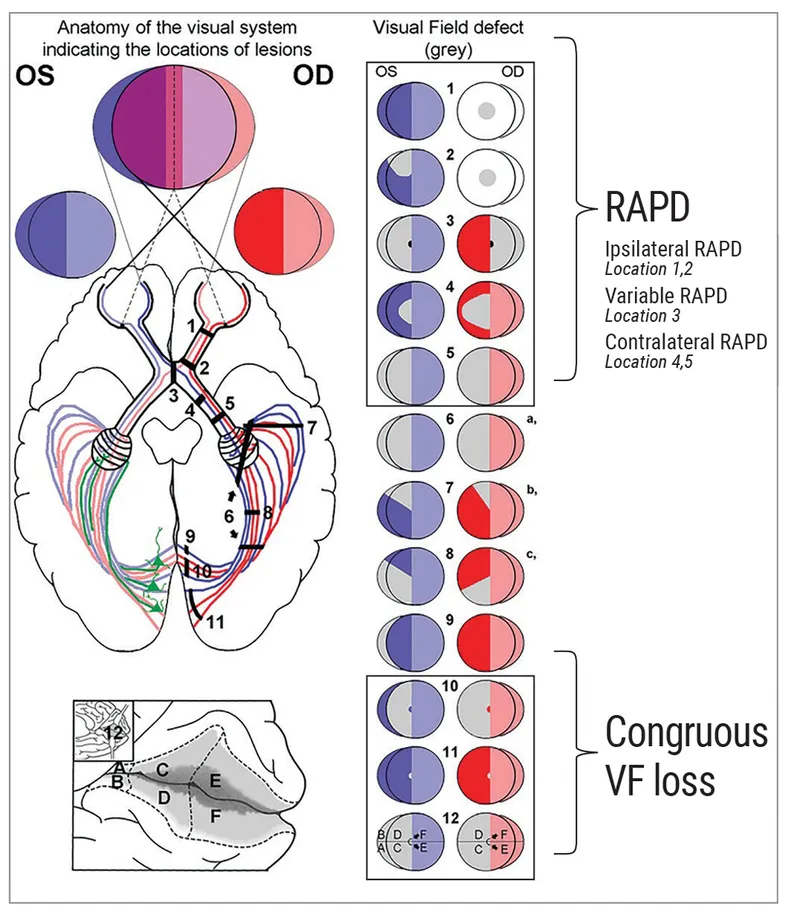
- The patient presents with unilateral vision loss (right eye) and a **relative afferent pupillary defect (RAPD)**, demonstrated by bilateral pupillary dilation when light swings from the unaffected left eye to the affected right eye.
- An RAPD localizes the lesion to the **afferent visual pathway anterior to the optic chiasm**, specifically the **retina or optic nerve (CN II)** of the affected eye.
- The **optic nerve** relays visual information TO the **lateral geniculate nucleus (LGN)** of the thalamus, making this the correct answer to the question "which structure does the defective nerve relay information to?"
- Note: A lesion directly AT the LGN (post-chiasmal) would cause vision loss but would NOT produce an RAPD, as the pupillary reflex integrates bilaterally at the pretectal nucleus before reaching the LGN.
*Oculomotor nucleus*
- The **oculomotor nucleus** contains motor neurons for CN III, controlling most extraocular muscles and providing parasympathetic innervation to the pupil via the Edinger-Westphal nucleus.
- A lesion here would cause **efferent deficits**: ipsilateral ptosis, eye positioned "down and out," and a dilated, fixed pupil - but NOT vision loss or RAPD.
- This is an efferent pathway issue, not an afferent visual pathway problem.
*Edinger-Westphal nucleus*
- The **Edinger-Westphal nucleus** provides preganglionic parasympathetic fibers via CN III to the ciliary ganglion, controlling pupillary constriction and accommodation.
- A lesion would cause a **dilated pupil with impaired direct and consensual light reflex** and impaired accommodation, but NOT vision loss or RAPD.
- This affects the efferent limb of the pupillary reflex, not the afferent visual pathway.
*Medial geniculate nucleus*
- The **medial geniculate nucleus (MGN)** is a thalamic relay nucleus in the **auditory pathway**, receiving input from the inferior colliculus.
- A lesion would cause hearing deficits, not visual symptoms or pupillary abnormalities.
*Ventral posteromedial nucleus*
- The **ventral posteromedial nucleus (VPM)** of the thalamus relays sensory information from the face (via trigeminal nerve) and taste sensation.
- A lesion would cause **facial sensory deficits** (numbness, altered sensation) or taste disturbances, not vision loss or RAPD.
Functional neuroanatomy of vision US Medical PG Question 3: A 62-year-old woman comes to the physician for decreased vision and worsening headaches since this morning. She has hypertension and hypercholesterolemia. Pulse is 119/min and irregular. Current medications include ramipril and atorvastatin. Ocular and funduscopic examination shows no abnormalities. The findings of visual field testing are shown. Which of the following is the most likely cause of this patient's symptoms?
- A. Occlusion of the posterior cerebral artery (Correct Answer)
- B. Occlusion of anterior cerebral artery
- C. Degeneration of the macula
- D. Occlusion of the anterior inferior cerebellar artery
- E. Impaired perfusion of the retina
Functional neuroanatomy of vision Explanation: ***Occlusion of the posterior cerebral artery***
- The patient presents with **acute visual field defect** and **headache** in the context of an **irregular pulse** (atrial fibrillation).
- **Atrial fibrillation** is a major risk factor for **cardioembolic stroke**, particularly affecting the posterior circulation.
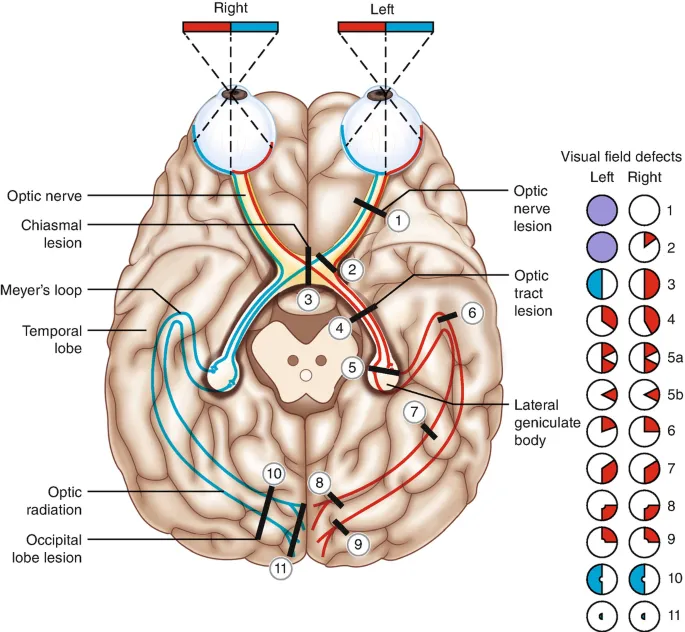
- The **posterior cerebral artery (PCA) supplies the occipital lobe**, which contains the primary visual cortex. PCA occlusion causes **contralateral homonymous hemianopia**, often with **macular sparing** due to collateral blood supply from the middle cerebral artery.
- The visual field defect pattern shown, combined with normal funduscopic examination (ruling out retinal pathology), is characteristic of **occipital cortex ischemia**.
- **Acute onset** with headache further supports an embolic stroke mechanism.
*Occlusion of anterior cerebral artery*
- Anterior cerebral artery (ACA) occlusion primarily affects the **frontal and medial parietal lobes**.
- Classic presentation includes **contralateral leg weakness** > arm weakness, sensory loss in the leg, and behavioral/personality changes.
- ACA strokes do **not cause visual field defects** or homonymous hemianopia.
*Degeneration of the macula*
- Macular degeneration causes **gradual central vision loss**, presenting with difficulty reading and central scotomas.
- This is a **chronic progressive condition**, not acute onset "since this morning."
- Would not cause **headache**, irregular pulse correlation, or the specific visual field pattern shown.
- Funduscopy would typically show **drusen** or retinal pigmentary changes.
*Occlusion of the anterior inferior cerebellar artery*
- AICA occlusion affects the **lateral pons and cerebellum**.
- Presents with **vertigo, nystagmus, ataxia, ipsilateral facial paralysis**, and hearing loss.
- Does **not affect the visual cortex** and would not cause homonymous visual field defects.
*Impaired perfusion of the retina*
- Central retinal artery occlusion causes **sudden monocular painless vision loss** (not bilateral field defects).
- Funduscopy would reveal **"cherry-red spot"** at the macula and retinal whitening.
- The question states funduscopic examination shows **no abnormalities**, excluding this diagnosis.
- Would not explain the bilateral homonymous field defect pattern.
Functional neuroanatomy of vision US Medical PG Question 4: A 34-year-old woman comes to the physician because she has not had her period for 4 months. Menses had previously occurred at regular 28-day intervals with moderate flow. A home pregnancy test was negative. She also reports recurrent headaches and has noticed that when she goes to the movies she cannot see the outer edges of the screen without turning her head to each side. This patient's symptoms are most likely caused by abnormal growth of which of the following?
- A. Adenohypophysis (Correct Answer)
- B. Astrocytes
- C. Schwann cells
- D. Pineal gland
- E. Arachnoid cap cells
Functional neuroanatomy of vision Explanation: ***Adenohypophysis***
- The patient's symptoms of **amenorrhea**, recurrent headaches, and **bitemporal hemianopsia** (cannot see the outer edges of the screen) strongly suggest a **pituitary adenoma**.
- Pituitary adenomas typically arise from the **adenohypophysis** and can cause hormonal imbalances (leading to amenorrhea) and compress the **optic chiasm** (leading to visual field defects).
*Astrocytes*
- **Astrocytes** are glial cells that support neurons and form the **blood-brain barrier**; their abnormal growth typically leads to **gliomas**, which present with different symptoms like seizures, focal neurological deficits, or increased intracranial pressure, rather than specific endocrine dysfunction and bitemporal hemianopsia.
- While gliomas can cause headaches and visual field defects, the combination with **amenorrhea** points away from this diagnosis.
*Schwann cells*
- **Schwann cells** produce myelin in the peripheral nervous system; abnormal growth usually results in **schwannomas**, which present with symptoms related to cranial nerve or spinal nerve compression (e.g., hearing loss in acoustic neuroma), not typically bitemporal hemianopsia or amenorrhea.
- Schwannomas are derived from the myelin sheaths of peripheral nerves and would not explain the endocrine disturbances seen here.
*Pineal gland*
- Lesions of the **pineal gland** often cause **Parinaud syndrome** (failure of upward gaze, pupillary abnormalities) due to compression of the superior colliculi, and can also lead to **hydrocephalus** or precocious puberty.
- While headaches can occur, **bitemporal hemianopsia** and **amenorrhea** are not characteristic presentations of pineal gland tumors.
*Arachnoid cap cells*
- Abnormal growth of **arachnoid cap cells** leads to **meningiomas**, which are typically slow-growing tumors arising from the meninges.
- Meningiomas can cause headaches and focal neurological deficits depending on their location, but they do **not typically cause bitemporal hemianopsia** or **endocrine dysfunction** like amenorrhea, as they are usually external to the brain tissue.
Functional neuroanatomy of vision US Medical PG Question 5: A 22-year-old man is brought to the physician by his mother because of concerns about his recent behavior. Three months ago, the patient first reported hearing loud voices coming from the ceiling of his room. During this time, he has also become increasingly worried that visitors to the house were placing secret surveillance cameras. Mental status examination shows tangential speech with paranoid thoughts. Treatment for this patient's condition predominantly targets which of the following dopaminergic pathways?
- A. Mesocortical pathway
- B. Thalamocortical pathway
- C. Nigrostriatal pathway
- D. Corticostriatal pathway
- E. Mesolimbic pathway (Correct Answer)
Functional neuroanatomy of vision Explanation: ***Mesolimbic pathway***
- The patient's symptoms of **auditory hallucinations** and **paranoid delusions** are **positive symptoms** of psychosis consistent with **schizophrenia**.
- **Hyperactivity** of the **mesolimbic dopaminergic pathway** is strongly associated with the positive symptoms of schizophrenia, making it the primary target for antipsychotic treatment.
*Mesocortical pathway*
- The **mesocortical pathway** is primarily involved in **cognition, motivation, and executive functions**, originating from the ventral tegmental area and projecting to the prefrontal cortex.
- **Hypoactivity** in this pathway is thought to contribute to the **negative and cognitive symptoms** of schizophrenia, not the positive symptoms described.
*Thalamocortical pathway*
- The **thalamocortical pathway** connects the **thalamus to the cerebral cortex** and is crucial for sensory processing, arousal, and consciousness.
- While involved in neural circuits, it is not considered a primary dopaminergic pathway targeted for the treatment of positive psychotic symptoms.
*Nigrostriatal pathway*
- The **nigrostriatal pathway** projects from the **substantia nigra to the striatum** and is primarily involved in **motor control**.
- Blocking dopamine receptors in this pathway by antipsychotic medications can cause **extrapyramidal symptoms (EPS)**, but it is not the main pathway responsible for positive psychotic symptoms or their treatment.
*Corticostriatal pathway*
- The **corticostriatal pathway** is **predominantly a glutamatergic pathway** connecting the **cerebral cortex to the striatum**, playing a role in motor control and habit formation.
- This is not a primary dopaminergic pathway and is not directly implicated in the positive symptoms of schizophrenia or their pharmacological treatment.
Functional neuroanatomy of vision US Medical PG Question 6: An 82-year-old right-handed woman is brought in by ambulance after being found down in her home. On presentation, she is found to be awake but does not follow directions or respond to questions. She is able to speak and produces a fluent string of nonsensical words and sounds. She does not appear to be bothered by her deficits. Subsequent neurologic exam finds that the patient is unable to comprehend any instructions and is also unable to repeat phrases. CT scan reveals an acute stroke to her left hemisphere. Damage to which of the following structures would be most likely to result in this pattern of deficits?
- A. Precentral gyrus
- B. Superior temporal gyrus (Correct Answer)
- C. Arcuate fasciculus
- D. Inferior frontal gyrus
- E. Watershed zone
Functional neuroanatomy of vision Explanation: ***Superior temporal gyrus***
- This patient presents with **fluent aphasia** (speaking nonsensical words), severely impaired **comprehension**, and impaired **repetition**. This triad is characteristic of **Wernicke's aphasia**.
- **Wernicke's area**, responsible for language comprehension, is located in the **posterior part of the superior temporal gyrus** in the dominant hemisphere (typically left).
*Precentral gyrus*
- The **precentral gyrus** contains the **primary motor cortex** and its damage would primarily cause contralateral motor deficits (e.g., **hemiparesis** or **hemiplegia**).
- This area is not directly involved in language comprehension or production of fluent but nonsensical speech.
*Arcuate fasciculus*
- Damage to the **arcuate fasciculus**, a white matter tract connecting Broca's and Wernicke's areas, results in **conduction aphasia**.
- In **conduction aphasia**, comprehension and fluency are relatively preserved, but **repetition is severely impaired**. This patient also has impaired comprehension.
*Inferior frontal gyrus*
- The **inferior frontal gyrus** houses **Broca's area**, which is responsible for **language production and motor aspects of speech**.
- Damage to this area typically causes **Broca's aphasia**, characterized by **non-fluent speech**, preserved comprehension, and impaired repetition. This patient has fluent speech.
*Watershed zone*
- **Watershed infarcts** occur at the borders between major arterial territories due to hypoperfusion, often leading to **transcortical aphasias**.
- While transcortical sensory aphasia involves impaired comprehension and fluent speech, **repetition is preserved**, which is not the case here.
Functional neuroanatomy of vision US Medical PG Question 7: A 78-year-old right-handed man with hypertension and hyperlipidemia is brought to the emergency department for sudden onset of nausea and vertigo one hour ago. Physical examination shows 5/5 strength in all extremities. Sensation to light touch and pinprick is decreased in the right arm and leg. A CT scan of the brain shows an acute infarction in the distribution of the left posterior cerebral artery. Further evaluation of this patient is most likely to show which of the following findings?
- A. Right-sided homonymous hemianopia (Correct Answer)
- B. Prosopagnosia
- C. Left-sided gaze deviation
- D. Left-sided hemineglect
- E. Right-sided superior quadrantanopia
Functional neuroanatomy of vision Explanation: ***Right-sided homonymous hemianopia***
- A **left PCA infarct** typically affects the **occipital lobe**, specifically the visual cortex or optic radiations, leading to a contralateral visual field deficit.
- The **right visual field** from both eyes projects to the left occipital lobe, so infarction here causes a **right homonymous hemianopia**.
*Prosopagnosia*
- **Prosopagnosia**, the inability to recognize faces, is associated with infarction of the **fusiform gyrus**, often a bilateral PCA territory infarction or an infarct affecting the right occipital or temporal lobe.
- This patient has a **left PCA infarct**, so isolated prosopagnosia is less likely.
*Left-sided gaze deviation*
- **Gaze deviation** usually occurs in lesions of the **frontal eye fields** (Brodmann area 8), which are supplied by the middle cerebral artery, causing the eyes to deviate towards the side of the lesion in acute stages.
- A **PCA infarct** typically spares the frontal eye fields and the brainstem gaze centers.
*Left-sided hemineglect*
- **Hemineglect** is most commonly associated with lesions of the **right parietal lobe** or right frontal lobe, primarily in the territory of the right middle cerebral artery.
- With a **left PCA infarct**, left-sided hemineglect is an unexpected finding.
*Right-sided superior quadrantanopia*
- A **superior quadrantanopia** is caused by damage to the **inferior optic radiations** (Meyer's loop), which typically carry information from the superior visual field.
- A complete **homonymous hemianopia** involving the entire right visual field is more characteristic of an occipital lobe lesion due to a PCA infarct, rather than an isolated quadrantanopia.
Functional neuroanatomy of vision US Medical PG Question 8: A 54-year-old man with hypertension and congenital blindness comes to the physician because he is unable to recognize objects by touch with his right hand. The symptoms started about 2 hours ago. When given a house key, he can feel the object in his right hand but is not able to identify what it is. This patient's condition is most likely caused by a lesion in which of the following locations?
- A. Ipsilateral cingulate gyrus
- B. Contralateral superior parietal lobule (Correct Answer)
- C. Ipsilateral inferior frontal gyrus
- D. Ipsilateral superior temporal gyrus
- E. Contralateral precentral gyrus
Functional neuroanatomy of vision Explanation: ***Contralateral superior parietal lobule***
- The patient exhibits **astereognosis**, which is the inability to recognize objects by touch despite intact sensation, suggesting a lesion in the **parietal association cortex**.
- Since the deficit is in the **right hand**, the lesion must be on the **contralateral side**, which is the left superior parietal lobule.
*Ipsilateral cingulate gyrus*
- The **cingulate gyrus** is primarily involved in emotion, learning, and memory, and a lesion here would not typically cause isolated astereognosis.
- Furthermore, astereognosis with the right hand implies a contralateral lesion, not an ipsilateral one.
*Ipsilateral inferior frontal gyrus*
- The **inferior frontal gyrus** (Broca's area) is crucial for speech production; damage here usually results in **expressive aphasia**.
- A lesion in this area would not explain the patient's specific difficulty with tactile object recognition in the right hand.
*Ipsilateral superior temporal gyrus*
- The **superior temporal gyrus** (Wernicke's area) is concerned with language comprehension; damage typically causes **receptive aphasia**.
- This location is not associated with astereognosis, nor would an ipsilateral lesion explain a right-hand deficit.
*Contralateral precentral gyrus*
- The **precentral gyrus** is the primary motor cortex; a lesion here would cause **motor deficits** such as weakness or paralysis of the contralateral side, not an inability to recognize objects by touch while sensation is intact.
- The patient can feel the object, indicating intact sensation and motor function, merely difficulty identifying it.
Functional neuroanatomy of vision US Medical PG Question 9: A 25-year-old previously healthy woman presents to her PCP reporting cessation of menses for the past 6 months. Previously, her period occurred regularly, every 30 days. She also complains of decreased peripheral vision, most noticeably when she is driving her car. She denies any recent sexual activity and a pregnancy test is negative. Upon further work-up, what physical exam finding is most likely to be identified?
- A. Breast mass
- B. Enlarged thyroid
- C. Bitemporal hemianopsia (Correct Answer)
- D. Renal failure
- E. Pregnancy
Functional neuroanatomy of vision Explanation: ***Bitemporal hemianopsia***
- The patient's symptoms of **amenorrhea** and **decreased peripheral vision** are highly suggestive of a **pituitary adenoma**, specifically one that causes mass effect on the optic chiasm.
- A pituitary adenoma can compress the **optic chiasm**, leading to the classic visual field defect known as **bitemporal hemianopsia**, where the temporal (peripheral) vision in both eyes is lost.
*Breast mass*
- While breast masses are common, they are generally **not associated** with amenorrhea or peripheral vision loss.
- A breast mass would typically present with a palpable lump or imaging abnormality of the breast.
*Enlarged thyroid*
- An enlarged thyroid (goiter) can be associated with thyroid dysfunction, which can cause menstrual irregularities, but it typically **does not cause peripheral vision loss**.
- Visual field defects point towards a problem with the **optic pathways**, not thyroid pathology.
*Renal failure*
- **Chronic renal failure** can cause menstrual irregularities due to hormonal imbalances, but it is **not directly linked** to visual field defects like bitemporal hemianopsia.
- Renal failure would present with symptoms like edema, fatigue, and changes in urination.
*Pregnancy*
- Although amenorrhea is a hallmark of pregnancy, the patient has explicitly **denied recent sexual activity** and a **negative pregnancy test** rules this out.
- Pregnancy does not cause **bitemporal hemianopsia** as a primary symptom.
Functional neuroanatomy of vision US Medical PG Question 10: A 32-year-old previously healthy female presents to her primary care physician with double vision. She first noted the double vision yesterday and saw no improvement this morning. She does not think it is worsening. She has not had any changes in her normal routine though she recalls one episode of right arm weakness 2 months ago. She did not seek treatment and the weakness subsided after several days. She does not have a history of head trauma. She denies headache, fever, chills, nausea, vomiting, paresthesias, extremity pain, or weakness. On exam she has right adduction palsy on leftward gaze. She has no focal weakness. Which of the following additional physical exam findings is associated with the lesion responsible for her ocular findings?
- A. Afferent pupillary defect in the left eye
- B. Horizontal nystagmus in the left eye on leftward gaze (Correct Answer)
- C. Ptosis on the right
- D. Left abduction palsy on leftward gaze
- E. Proptosis of the right eye
Functional neuroanatomy of vision Explanation: **Horizontal nystagmus in the left eye on leftward gaze**
- The patient presents with **double vision** and **right adduction palsy on leftward gaze**, indicative of an **internuclear ophthalmoplegia (INO)**, highly suggestive of **multiple sclerosis (MS)** in a young adult with a history of transient neurological symptoms (right arm weakness).
- In INO, the eye attempting to adduct (in this case, the right eye on leftward gaze) has impaired movement, while the contralateral abducting eye (left eye on leftward gaze) often exhibits **horizontal nystagmus**.
*Afferent pupillary defect in the left eye*
- An **afferent pupillary defect (APD)**, also known as a **Marcus Gunn pupil**, indicates a lesion to the **afferent visual pathway** (retina, optic nerve, or optic chiasm).
- While MS can cause optic neuritis leading to APD, it is not a direct consequence or associated finding of an INO itself.
*Ptosis on the right*
- **Ptosis** (drooping eyelid) is typically caused by dysfunction of the **oculomotor nerve (cranial nerve III)** or the **sympathetic pathway (Horner's syndrome)**.
- While MS can affect cranial nerves, ptosis is not a characteristic finding specifically associated with INO.
*Left abduction palsy on leftward gaze*
- A **left abduction palsy on leftward gaze** would mean the left eye is unable to fully abduct, indicating a problem with the **left abducens nerve (cranial nerve VI)** or its nucleus.
- In INO, it is the **adduction** of the ipsilateral eye that is impaired, and the contralateral eye typically **abducts normally** but with nystagmus.
*Proptosis of the right eye*
- **Proptosis** (exophthalmos) is the bulging of the eye from the orbit, usually caused by retro-orbital mass lesions (e.g., **thyroid eye disease**, orbital tumors) or inflammation.
- This finding is unrelated to the neurological lesion causing an INO.
More Functional neuroanatomy of vision US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.