Functional neuroanatomy of hearing and balance US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Functional neuroanatomy of hearing and balance. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Functional neuroanatomy of hearing and balance US Medical PG Question 1: A 55-year-old woman presents to the physician with repeated episodes of dizziness for the last 3 months, which are triggered by rising from a supine position and by lying down. The episodes are sudden and usually last for less than 30 seconds. During the episode, she feels as if she is suddenly thrown into a rolling spin. She has no symptoms in the period between episodes. The patient denies having headaches, vomiting, deafness, ear discharge or ear pain. There is no history of a known medical disorder or prolonged consumption of a specific drug. The vital signs are within normal limits. On physical examination, when the physician asks the woman to turn her head 45° to the right, and then to rapidly move from the sitting to the supine position, self-limited rotatory nystagmus is observed following her return to the sitting position. The rest of the neurological examination is normal. Which of the following is the treatment of choice for the condition of this patient?
- A. Oral prednisolone for 2 weeks and follow-up
- B. Singular neurectomy
- C. Posterior canal occlusion
- D. Canalith repositioning (Correct Answer)
- E. Oral meclizine for 6 weeks and follow-up
Functional neuroanatomy of hearing and balance Explanation: ***Canalith repositioning***
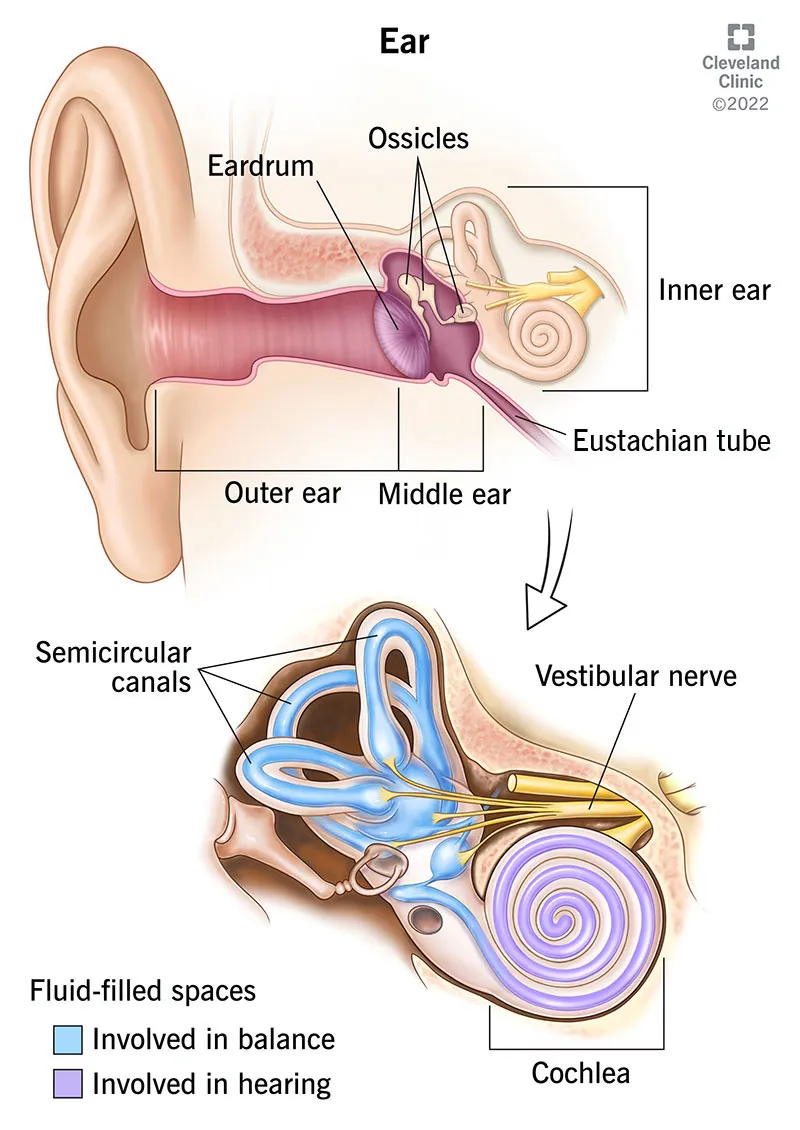
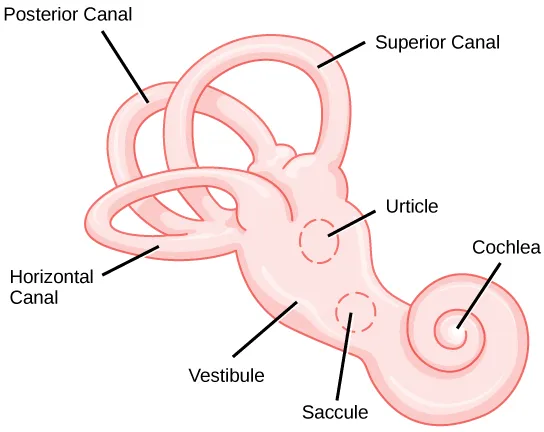
- The patient's symptoms (short-lasting, positional dizziness, rolling spin sensation, absence of other neurological symptoms, and positive **Dix-Hallpike maneuver** with **rotatory nystagmus**) are characteristic of **Benign Paroxysmal Positional Vertigo (BPPV)**.
- **Canalith repositioning maneuvers** (e.g., Epley maneuver) are the treatment of choice as they aim to move dislodged otoconia out of the semicircular canals.
*Oral prednisolone for 2 weeks and follow-up*
- **Prednisolone** is a corticosteroid used for inflammatory conditions, but it is **not indicated for BPPV**, which is a mechanical problem.
- While corticosteroids might be used in other vestibular disorders like Meniere's disease or vestibular neuritis, they would not address the underlying cause of BPPV.
*Singular neurectomy*
- **Singular neurectomy** is a surgical procedure that involves cutting the singular nerve (posterior ampullary nerve).
- This is a highly invasive treatment reserved for **intractable BPPV** that has failed multiple conservative treatments, and it carries risks such as hearing loss.
*Posterior canal occlusion*
- **Posterior canal occlusion** is a surgical procedure that involves plugging the posterior semicircular canal.
- This is a surgical option for **severe, refractory BPPV** that has not responded to canalith repositioning maneuvers, and it is more invasive than repositioning.
*Oral meclizine for 6 weeks and follow-up*
- **Meclizine** is an antihistamine used to relieve symptoms of nausea, vomiting, and dizziness associated with vertigo.
- While it can help alleviate symptoms, it does **not treat the underlying cause of BPPV** and is typically used for symptomatic relief, not as a definitive treatment.
Functional neuroanatomy of hearing and balance US Medical PG Question 2: A 69-year-old man comes to the physician with a 2-year history of progressive hearing loss. His hearing is worse in crowded rooms, and he has noticed that he has more difficulty understanding women than men. He has no history of serious illness and does not take any medications. A Rinne test shows air conduction is greater than bone conduction bilaterally. This condition is most likely associated with damage closest to which of the following structures?
- A. Tympanic membrane
- B. Round window
- C. Base of the stapes
- D. External acoustic meatus
- E. Basal turn of the cochlea (Correct Answer)
Functional neuroanatomy of hearing and balance Explanation: ***Basal turn of the cochlea***
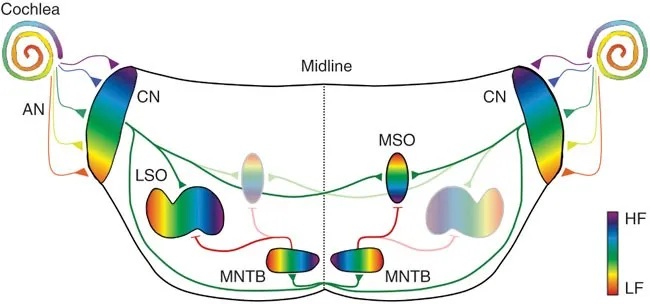
- The patient's presentation of progressive hearing loss, difficulty hearing in crowded rooms (**presbycusis**), and trouble understanding women's voices (higher frequencies) is characteristic of **sensorineural hearing loss**.
- The **basal turn of the cochlea** is responsible for detecting high-frequency sounds, making it the most likely site of damage in presbycusis.
*Tympanic membrane*
- Damage to the **tympanic membrane** would typically result in a **conductive hearing loss**, characterized by bone conduction being greater than air conduction (abnormal Rinne test).
- The patient's Rinne test shows air conduction greater than bone conduction, indicating a sensorineural or normal hearing pattern.
*Round window*
- The **round window** plays a role in relieving pressure in the cochlea, allowing fluid movement and sound transmission.
- While damage here can affect hearing, it's not the primary site of progressive, age-related high-frequency sensorineural loss.
*Base of the stapes*
- Issues at the **base of the stapes**, particularly **otosclerosis**, cause **conductive hearing loss** due to the ossification of the oval window, hindering sound transmission.
- This would present with an abnormal Rinne test (BC > AC), which is not observed in this patient.
*External acoustic meatus*
- Obstruction or damage to the **external acoustic meatus** (e.g., earwax impaction, otitis externa) would cause a **conductive hearing loss**.
- The Rinne test would show bone conduction greater than air conduction, which is inconsistent with the patient's findings.
Functional neuroanatomy of hearing and balance US Medical PG Question 3: A 75-year-old woman with hypertension presents to your office for a routine health exam. Her medications include hydrochlorothiazide and a multivitamin. She has been feeling well; however, she mentions that her family has been complaining about the volume of the television. She also reports difficulty hearing when others have called her name. On physical examination, her temperature is 99°F (37.2°C), blood pressure is 120/85 mmHg, pulse is 70/min, respirations are 17/min, and pulse oximetry is 99% on room air. The tympanic membrane is gray with no drainage or granulation tissue. Audiometry is consistent with high frequency sensorineural hearing loss. Which of the following is the most likely physiology behind this patient’s presentation?
- A. Bacterial infection of the middle ear
- B. Destruction of cochlear hair cells (Correct Answer)
- C. Increased endolymph production
- D. Abnormal skin growth in the middle ear
- E. Fixation of the stapes to the cochlea
Functional neuroanatomy of hearing and balance Explanation: ***Destruction of cochlear hair cells***
- The patient's age and history of **high-frequency sensorineural hearing loss** on audiometry are characteristic of **presbycusis**, which is primarily caused by **age-related degeneration of cochlear hair cells**.
- **Sensory hair cells** in the **basal turn of the cochlea**, which are responsible for detecting high-frequency sounds, are particularly vulnerable to age-related damage and are often the first to be affected.
*Bacterial infection of the middle ear*
- A bacterial infection of the middle ear, or **otitis media**, would typically present with **ear pain**, **fever**, and signs of inflammation on **tympanic membrane examination**, none of which are noted here.
- Furthermore, otitis media primarily causes a **conductive hearing loss**, whereas the patient has **sensorineural hearing loss**.
*Increased endolymph production*
- **Increased endolymph production** or **Meniere's disease** is characterized by episodic **vertigo**, **tinnitus**, and ** fluctuating sensorineural hearing loss**, often affecting low frequencies initially.
- The patient's chronic, progressive high-frequency hearing loss without vertigo does not align with Meniere's disease.
*Abnormal skin growth in the middle ear*
- An **abnormal skin growth** in the middle ear, or **cholesteatoma**, typically presents with **conductive hearing loss**, **otorrhea (ear discharge)**, and possibly **tinnitus** or **vertigo**.
- The patient has **sensorineural hearing loss**, and there is no mention of discharge or other symptoms indicative of a cholesteatoma.
*Fixation of the stapes to the cochlea*
- **Otosclerosis**, which involves the **fixation of the stapes** to the oval window (not the cochlea), leads to **conductive hearing loss** due to impaired sound transmission to the inner ear.
- The patient's audiometry specifically indicates **sensorineural hearing loss**, ruling out otosclerosis as the primary cause.
Functional neuroanatomy of hearing and balance US Medical PG Question 4: A 45-year-old male presents to his primary care physician for complaints of dizziness. The patient reports he experiences room-spinning dizziness lasting several hours at a time, approximately 2-3 times a month, starting 3 months ago. Upon questioning, the patient also reports right sided diminished hearing, tinnitus, and a sensation of ear fullness. His temperature is 99 deg F (37.2 deg C), pulse 70/min, respirations 12, blood pressure 130 mmHg/85 mmHg, SpO2 99%. You decide to order an audiometric evaluation. What is the most likely finding of the audiogram?
- A. Low frequency sensorineural hearing loss (Correct Answer)
- B. Normal audiogram
- C. High frequency conductive hearing loss
- D. High frequency sensorineural hearing loss
- E. Low frequency conductive hearing loss
Functional neuroanatomy of hearing and balance Explanation: ***Low frequency sensorineural hearing loss***
- The constellation of **episodic vertigo**, **tinnitus**, **aural fullness**, and **fluctuating hearing loss** is classic for **Ménière's disease**.
- In Ménière's disease, the characteristic audiogram finding is a **sensorineural hearing loss** that predominantly affects the **low frequencies**.
*Normal audiogram*
- A normal audiogram would not explain the patient's reported symptoms of **diminished hearing** and **tinnitus**.
- These symptoms indicate an underlying auditory dysfunction, which a normal audiogram would rule out.
*High frequency conductive hearing loss*
- **Conductive hearing loss** indicates an issue with sound transmission through the outer or middle ear (e.g., **otosclerosis**, **cerumen impaction**).
- The reported symptoms and the characteristic low-frequency involvement in Ménière's disease do not align with high-frequency conductive hearing loss.
*High frequency sensorineural hearing loss*
- While sensorineural hearing loss is correct, **high-frequency loss** is more typical of **presbycusis** (age-related hearing loss) or **noise-induced hearing loss**.
- Ménière's disease characteristically affects the **low frequencies** initially.
*Low frequency conductive hearing loss*
- **Conductive hearing loss** implies a problem in the outer or middle ear, which is not consistent with the pathology of **Ménière's disease** (endolymphatic hydrops affecting the inner ear).
- While the frequency range is correct, the type of hearing loss (conductive vs. sensorineural) is incorrect for Ménière's disease.
Functional neuroanatomy of hearing and balance US Medical PG Question 5: A 56-year-old woman presents to the emergency department with several episodes in which she felt "dizzy." She has had these symptoms on and off for the past year and can recall no clear exacerbating factor or time of day when her symptoms occur. She has a perpetual sensation of fullness in her ear but otherwise has no symptoms currently. Her temperature is 97.6°F (36.4°C), blood pressure is 122/77 mmHg, pulse is 85/min, respirations are 13/min, and oxygen saturation is 98% on room air. Cardiopulmonary exam is unremarkable. The patient's gait is stable. Which of the following is also likely to be found in this patient?
- A. Gradually improving symptoms
- B. Conductive hearing loss
- C. Positional vertigo
- D. Sensorineural hearing loss (Correct Answer)
- E. Vertical nystagmus
Functional neuroanatomy of hearing and balance Explanation: ***Sensorineural hearing loss***
- The sensation of **aural fullness**, recurrent dizzy spells without clear triggers, and the episodic nature of symptoms are classic for **Ménière's disease**.
- **Ménière's disease** is characterized by the triad of **vertigo**, **tinnitus**, and **sensorineural hearing loss**, often accompanied by ear fullness.
*Gradually improving symptoms*
- **Ménière's disease** is a chronic, progressive condition, and symptoms typically **fluctuate** in severity and can worsen over time, rather than gradually improving.
- While periods of remission can occur, the underlying pathology does make a steady improvement unlikely without intervention.
*Conductive hearing loss*
- **Conductive hearing loss** results from problems with sound transmission to the inner ear, such as **earwax** or **ossicular chain dysfunction**.
- **Ménière's disease** specifically affects the inner ear (cochlea and vestibular system), leading to **sensorineural hearing loss** due to endolymphatic hydrops.
*Positional vertigo*
- **Positional vertigo** suggests conditions like **Benign Paroxysmal Positional Vertigo (BPPV)**, where vertigo is triggered by specific head movements due to otolith displacement.
- In this patient, the vertigo is described as recurrent and "on and off" without "clear exacerbating factor," which is less consistent with positional vertigo.
*Vertical nystagmus*
- **Vertical nystagmus** is typically indicative of **central vestibular lesions** or brainstem dysfunction.
- The symptoms presented, including aural fullness and episodic dizziness, point towards a **peripheral vestibular disorder** like Ménière's disease, which usually causes horizontal or rotatory nystagmus during acute attacks.
Functional neuroanatomy of hearing and balance US Medical PG Question 6: Where does the only cranial nerve without a thalamic relay nucleus enter the skull?
- A. Superior orbital fissure
- B. Internal auditory meatus
- C. Foramen rotundum
- D. Jugular foramen
- E. Cribriform plate (Correct Answer)
Functional neuroanatomy of hearing and balance Explanation: ***Cribriform plate***
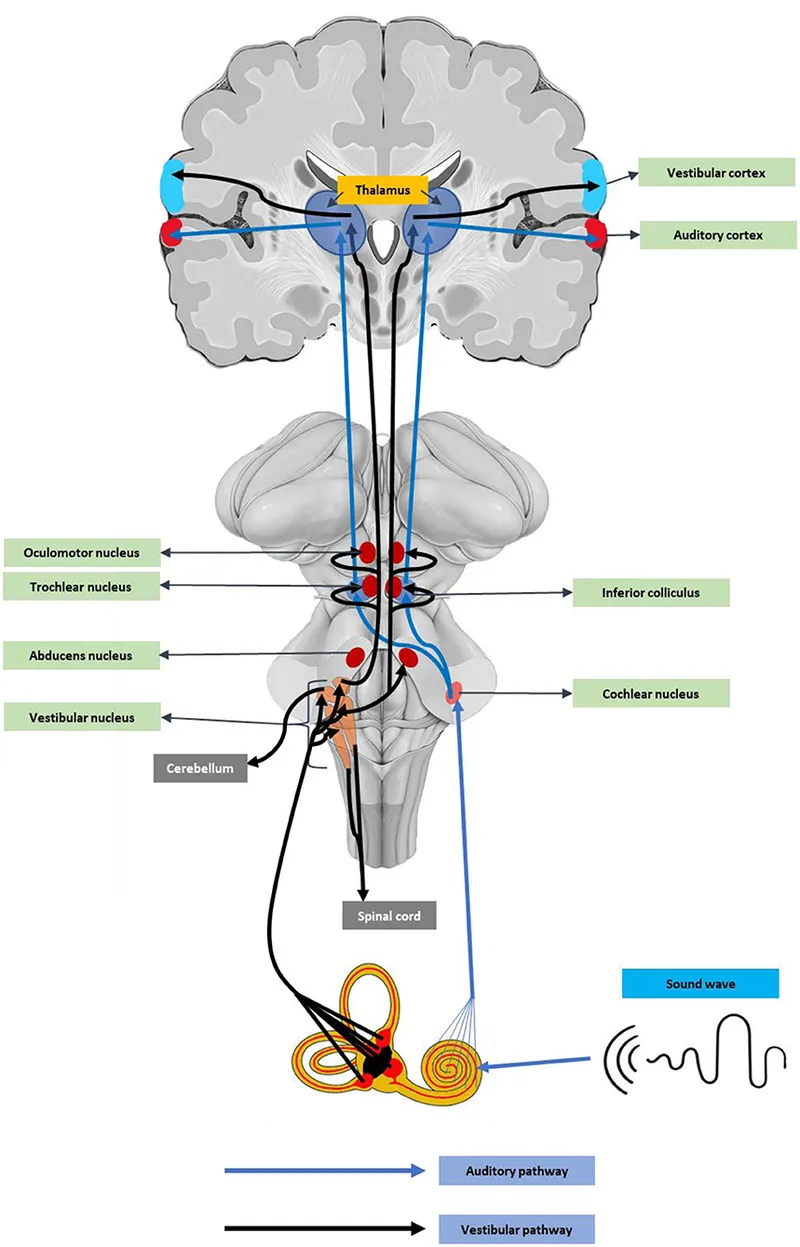
- The **olfactory nerve (CN I)** is the only cranial nerve that does not have a thalamic relay nucleus before reaching the cerebral cortex.
- It passes through the **cribriform plate** of the ethmoid bone to reach the olfactory bulbs.
*Superior orbital fissure*
- This opening transmits the **oculomotor (CN III), trochlear (CN IV), ophthalmic division of trigeminal (CN V1)**, and **abducens (CN VI)** nerves.
- These nerves all have sensory or motor components that relay through the thalamus, directly or indirectly.
*Internal auditory meatus*
- This canal transmits the **facial (CN VII)** and **vestibulocochlear (CN VIII)** nerves.
- The vestibulocochlear nerve's auditory pathway involves a thalamic relay in the **medial geniculate nucleus**.
*Foramen rotundum*
- The **maxillary division of the trigeminal nerve (CN V2)** passes through the foramen rotundum.
- Sensory information carried by CN V2 relays through the **thalamus**.
*Jugular foramen*
- This opening transmits the **glossopharyngeal (CN IX), vagus (CN X)**, and **accessory (CN XI)** nerves.
- Sensory components of these nerves, particularly taste and visceral sensation, involve thalamic nuclei.
Functional neuroanatomy of hearing and balance US Medical PG Question 7: A 67-year-old female patient is brought to the emergency department after her daughter noticed she has been having meaningless speech. When assessing the patient, she calls the chair a table, and at times would make up new words. She does not appear to be aware of her deficit, and is carrying on an empty conversation. Her speech is fluent, but with paraphasic errors. Her repetition is impaired. On physical examination, a right upper quadrant field-cut is appreciated, with impairment in comprehension and repetition. Which of the following structures is most likely involved in this patient’s presentation?
- A. Superior temporal gyrus (Correct Answer)
- B. Arcuate fasciculus
- C. Inferior frontal gyrus
- D. Frontal lobe, sparing Brodmann's area 44 and 45
- E. Arcuate fasciculus, inferior frontal gyrus, and superior temporal gyrus
Functional neuroanatomy of hearing and balance Explanation: ***Superior temporal gyrus***
- The patient's presentation of **fluent aphasia** with **paraphasic errors**, **impaired comprehension**, **impaired repetition**, and **lack of awareness** of the deficit is classic for **Wernicke's aphasia**.
- **Wernicke's area**, located in the posterior part of the **superior temporal gyrus** (Brodmann area 22) in the dominant hemisphere, is responsible for language comprehension.
*Arcuate fasciculus*
- Damage to the **arcuate fasciculus** typically causes **conduction aphasia**, characterized by **impaired repetition** with relatively preserved comprehension and fluent speech.
- However, it does not explain the significant comprehension deficits and paraphasic errors seen in this patient to the same extent as a Wernicke's lesion.
*Inferior frontal gyrus*
- The **inferior frontal gyrus** (Brodmann areas 44 and 45) is commonly associated with **Broca's area**, responsible for language production.
- Damage here would result in **non-fluent aphasia** with effortful speech and relatively preserved comprehension, which is contrary to the patient's fluent speech.
*Frontal lobe, sparing Brodmann's area 44 and 45*
- While damage to other parts of the **frontal lobe** can cause various cognitive deficits, sparing Broca's area (44 and 45) would generally not result in the specific pattern of **fluent aphasia** with severe comprehension and repetition impairment seen here.
- This option does not precisely localize the critical language areas affected.
*Arcuate fasciculus, inferior frontal gyrus, and superior temporal gyrus*
- While damage to all these areas would certainly cause severe aphasia, the specific constellation of symptoms—**fluent speech**, **poor comprehension**, **poor repetition**, and **paraphasic errors**—points most directly and primarily to involvement of the **superior temporal gyrus** (Wernicke's area).
- While some level of repetition impairment (seen in Wernicke's aphasia) implies some involvement in the broader language network, a lesion centered in the superior temporal gyrus is the most parsimonious explanation for this classic presentation.
Functional neuroanatomy of hearing and balance US Medical PG Question 8: A 55-year-old woman presents to her family physician with a 1-week history of dizziness. She experiences spinning sensations whenever she lies down and these sensations increase when she turns her head to the right. These episodes are transient, intermittent, last for less than a minute, occur multiple times in a day, and are associated with nausea. Between the episodes, she is fine and is able to perform her routine activities. She denies fever, hearing disturbances, diplopia, tinnitus, and recent flu or viral illness. Past medical history is significant for diabetes mellitus type 2, hypertension, and hypercholesterolemia. She does not use tobacco or alcohol. Her blood pressure is 124/78 mm Hg, the heart rate is 79/min, and the respiratory rate is 13/min. During the examination, when she is asked to lie supine from a sitting position with her head rotated towards the right side at 45°, horizontal nystagmus is observed. What is the next best step in the management of this patient?
- A. Dix-Hallpike maneuver
- B. Epley maneuver (Correct Answer)
- C. MRI of the brain with gadolinium
- D. Broad-spectrum antibiotics
- E. High dose steroids
Functional neuroanatomy of hearing and balance Explanation: ***Epley maneuver***
- The patient's presentation with **transient, positional vertigo** triggered by head movements, associated with nausea, and demonstrating **horizontal nystagmus** on positional testing is diagnostic of **Benign Paroxysmal Positional Vertigo (BPPV)**.
- Since the diagnostic positional maneuver has already been performed and BPPV is confirmed, the **next best step is canalith repositioning** using the **Epley maneuver**.
- The Epley maneuver is the **gold standard treatment** for posterior canal BPPV with **70-90% success rate** after a single treatment session, and it directly addresses the underlying pathophysiology by relocating displaced otoconia.
- This is recommended as **first-line treatment** by the American Academy of Otolaryngology-Head and Neck Surgery guidelines.
*Dix-Hallpike maneuver*
- The **Dix-Hallpike maneuver** is primarily a **diagnostic test** to confirm BPPV and identify the affected semicircular canal.
- The question stem describes that a positional maneuver has already been performed with nystagmus observed, effectively confirming the diagnosis.
- While repeating the diagnostic test might be considered, it is not the next management step once BPPV is confirmed.
*MRI of the brain with gadolinium*
- This investigation is generally reserved for patients with suspected **central causes of vertigo** or other neurological deficits.
- The patient's symptoms are highly suggestive of a peripheral vestibular disorder, and the absence of **ataxia, diplopia, dysarthria**, or other focal neurological signs makes a brain MRI unnecessary at this stage.
*Broad-spectrum antibiotics*
- Antibiotics are used to treat **bacterial infections**, such as bacterial labyrinthitis or meningitis, which can cause vertigo.
- The patient denies fever, recent infections, or other signs of infection, making antibiotic therapy inappropriate for this presentation.
*High dose steroids*
- Corticosteroids are sometimes used in conditions like **vestibular neuritis** or **Meniere's disease** to reduce inflammation.
- The patient's symptoms are not consistent with these conditions; the positional nature of her vertigo and lack of continuous symptoms point away from an inflammatory process.
- Vestibular suppressants (meclizine) may provide symptomatic relief but are **adjunctive** rather than definitive treatment for BPPV.
Functional neuroanatomy of hearing and balance US Medical PG Question 9: An 82-year-old right-handed woman is brought in by ambulance after being found down in her home. On presentation, she is found to be awake but does not follow directions or respond to questions. She is able to speak and produces a fluent string of nonsensical words and sounds. She does not appear to be bothered by her deficits. Subsequent neurologic exam finds that the patient is unable to comprehend any instructions and is also unable to repeat phrases. CT scan reveals an acute stroke to her left hemisphere. Damage to which of the following structures would be most likely to result in this pattern of deficits?
- A. Precentral gyrus
- B. Superior temporal gyrus (Correct Answer)
- C. Arcuate fasciculus
- D. Inferior frontal gyrus
- E. Watershed zone
Functional neuroanatomy of hearing and balance Explanation: ***Superior temporal gyrus***
- This patient presents with **fluent aphasia** (speaking nonsensical words), severely impaired **comprehension**, and impaired **repetition**. This triad is characteristic of **Wernicke's aphasia**.
- **Wernicke's area**, responsible for language comprehension, is located in the **posterior part of the superior temporal gyrus** in the dominant hemisphere (typically left).
*Precentral gyrus*
- The **precentral gyrus** contains the **primary motor cortex** and its damage would primarily cause contralateral motor deficits (e.g., **hemiparesis** or **hemiplegia**).
- This area is not directly involved in language comprehension or production of fluent but nonsensical speech.
*Arcuate fasciculus*
- Damage to the **arcuate fasciculus**, a white matter tract connecting Broca's and Wernicke's areas, results in **conduction aphasia**.
- In **conduction aphasia**, comprehension and fluency are relatively preserved, but **repetition is severely impaired**. This patient also has impaired comprehension.
*Inferior frontal gyrus*
- The **inferior frontal gyrus** houses **Broca's area**, which is responsible for **language production and motor aspects of speech**.
- Damage to this area typically causes **Broca's aphasia**, characterized by **non-fluent speech**, preserved comprehension, and impaired repetition. This patient has fluent speech.
*Watershed zone*
- **Watershed infarcts** occur at the borders between major arterial territories due to hypoperfusion, often leading to **transcortical aphasias**.
- While transcortical sensory aphasia involves impaired comprehension and fluent speech, **repetition is preserved**, which is not the case here.
Functional neuroanatomy of hearing and balance US Medical PG Question 10: Name the center shown as $X$ in the cut section of medulla which is responsible for control of respiration.
- A. Pneumotaxic centre
- B. Pre-Botzinger Complex (Correct Answer)
- C. Nucleus Para-brachialis
- D. Dorsal group of respiratory neurons
- E. Ventral group of respiratory neurons
Functional neuroanatomy of hearing and balance Explanation: ***Pre-Botzinger Complex***
- The **pre-Bötzinger complex** in the medulla is crucial for generating the **respiratory rhythm** and is the primary site of inspiratory rhythmogenesis.
- It is located ventral to the nucleus ambiguus and contains **pacemaker neurons** that fire spontaneously.
*Pneumotaxic centre*
- The **pneumotaxic center** is located in the **pons**, specifically the upper pons, and primarily regulates respiratory rate and depth.
- It works by sending inhibitory signals to the inspiratory center, thereby **limiting inspiration**.
*Nucleus Para-brachialis*
- The **nucleus parabrachialis** is located in the pons and includes the pneumotaxic center, affecting the **transition between inspiration and expiration**.
- It helps in fine-tuning respiratory patterns rather than initiating the basic rhythm.
*Dorsal group of respiratory neurons*
- The **dorsal respiratory group (DRG)**, located in the medulla, primarily controls **inspiration** and receives sensory input from chemoreceptors and mechanoreceptors.
- While it initiates the basic inspiratory muscle activity, the pre-Bötzinger complex is considered the rhythm generator.
*Ventral group of respiratory neurons*
- The **ventral respiratory group (VRG)**, located in the ventrolateral medulla, contains neurons responsible for both **inspiration and expiration**.
- The pre-Bötzinger complex is actually part of the VRG and serves as the **rhythm-generating center** within this larger group.
More Functional neuroanatomy of hearing and balance US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.